We’ve all heard the adage that practice makes perfect and to become an expert you must complete 10 000 hours of deliberate practice1. This involves motivated, goal oriented, purposeful practice with periodic feedback. Feedback is critical to allow for growth from where you currently are as a clinical clerk to where you want to be as future practicing physician2. Even with extensive deliberate practice, you will plateau without guidance and identification of areas to improve through feedback. However, feedback can be difficult to come by in a busy emergency department. We will break down how to solicit high quality feedback as a clinical clerk on your emergency department shifts.
Reflection
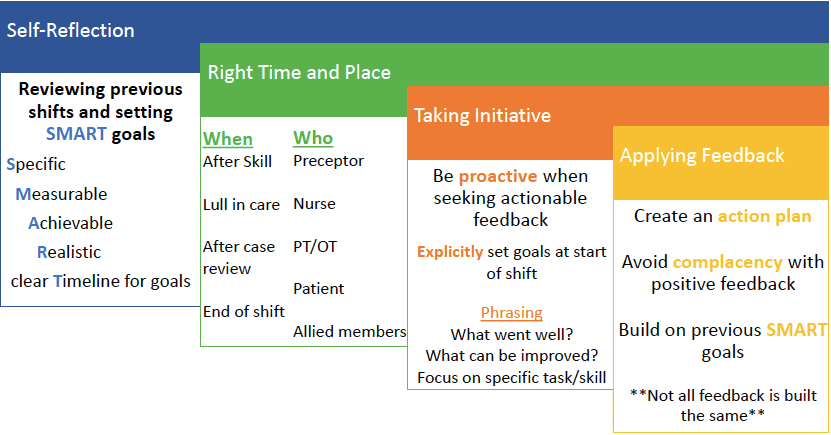
Throughout your clinical experiences as a trainee in the emergency department, you will work with many preceptors with different teaching and evaluation styles. Therefore, it will be up to you to take control of your learning and to guide the feedback you receive. This starts by engaging in reflective practice to ensure you solicit specific feedback3. After each shift, take a moment and sit down to think back on one element that went well, and one area that could use improvement. Explicitly write down these attributes and then create a plan using the SMART framework; creating Specific, Measurable, Achievable, Relevant goals with clear Timelines4,5. Ensure the goal is specific and clearly outlined. This is to avoid setting goals and future aspirations that are too general.
Vague goals are difficult to put an action plan in place to achieve. Break down clinical encounters into discrete tasks, which will better allow you to seek out meaningful feedback. The goal needs to be measurable to ensure you can quantify whether you are on track and if you have achieved the goal. The means to measure your progress can be based on an objective measure such as speed, or subjective measure such as a preceptor informing you that you have become proficient.
Additionally, the goal needs to be challenging so that you continue to grow and improve but not one that is well out of the scope of your practice. Bouncing ideas and goals off more senior learners and preceptors will ensure your goals are achievable. In the same regard, you should ensure your goal is relevant to the practice of emergency medicine. Finally, it is important to create a timeline that will keep you accountable and allow you to monitor your progress. An example of a SMART goal is “completing a thorough history and physical for the chief complaint of chest pain in under 15 minutes by the end of this elective”.
Who and When
Now that you have looked back on your previous shifts, set future learning goals, and have a general idea of what areas you would like to get feedback on; it is important to decide who to ask for feedback and when. Instinctively and reflexively your first thought will be to ask your preceptor. However, there are many other members of the team that have extensive knowledge and can provide feedback on how you are performing.
Receiving feedback from nurses, respiratory therapists, and consultants provides a unique vantage point4. It is important to capitalize on opportunities; if you order IV fluids, ask to demonstrate how you start an IV with the nurse assigned to your patient. If you are at a resuscitation, stand at the head of the bed and work alongside the respiratory therapist getting feedback on bag mask ventilation, placement of oral airways, and placement of definitive airways. After providing a consult, check in with the consultant; what information were you missing and what did you do well? It will allow you to collect more data on your skills and improve your interdisciplinary collaboration. Even asking your patients how your interview skills were or what they liked or didn’t like about your care can be very eye opening.
It can be difficult soliciting feedback from your staff person. The emergency department is a busy place, which poses a challenge for requesting feedback. Most commonly this occurs at the end of shift, when theoretically there are less interruptions and you have wrapped up the care of your patients. But with a faculty preceptor it may be of benefit to solicit feedback early during a shift, especially if you were hoping to receive feedback on a particular skill such as a procedure or common patient presentation. Soliciting feedback shortly after such a case makes it easier on the individual giving feedback and it will be more meaningful as the most salient issues or positives will be on the top of the assessor’s mind. Setting a clear objective with your staff at the beginning of your shift is helpful; it allows them to plan their day. Share your SMART goal at the start of the shift so they can keep an eye out for opportunities for feedback.
Phrasing
Not all members of the health care team will readily provide feedback. Therefore, it is important to be proactive when seeking feedback. At the beginning of each shift, explicitly set out some goals and areas you are hoping to get feedback on to your preceptor6. After setting the stage for an open dialogue by making your goals explicit, you will invariably stumble upon a perfect opportunity in your shift to ask for feedback, a rare lull in which all the sick patients are now stable, and you are awaiting the results of various investigations. Now it is important to phrase your request effectively, here are the key points to keep in mind:
- Ask for both things that went well and areas that you could improve on
- Focus on a task or skill
- Ex: I am hoping to improve blank. Do you have any suggestions?
- The request needs to be specific and allow for tangible feedback. An error learners often make is simply asking for feedback on history taking skills or broadly asking at the end of shifts if there were any areas they could improve on.
- A good example if you were hoping to improve on how to obtain a history would be “ Could you observe my interaction with the next patient and provide suggestions on how I can improve my history taking around chest pain? What areas did you find that went well and how can I improve my approach in the future?”. This example is specific, solicites both positive and negative feedback, and asks for the assessor to draw on their inherent expertise.
Creating an Action Plan
You’ve aerated the soil by broaching the topic of feedback, planted the seed by setting discrete goals, and provided water by soliciting focused feedback. To your astonishment the fruit of your labour produced a bounty of eloquent, concise, and well thought out feedback. Unfortunately, the hard work does not end here. Next you need to take the feedback and create an action plan to ensure that you continue to grow and develop as an individual and clinician6. It is important to utilize both the positive and constructive feedback you receive to identify areas to improve on and means in which you will do so. Do not allow positive feedback to make you complacent; this is not an affirmation that you have arrived and can now stop. It is simply reassurance that you are on the right track and to continue to push for improvement. Ensure that when you reflect on the feedback you received, you implement the SMART framework to create an action plan.
Above all else it will be up to you to implement judgment and discretion when soliciting feedback. There may be many shifts that do not afford you opportunities to solicit effective feedback. As well, you will come across preceptors that may not provide practical feedback. Do not be discouraged; not all learning experiences will be ideal. However, when you come across a clinical preceptor that you connect with, do your best to foster that relationship and seek support and feedback from them, whether it be by seeking out future shadowing experiences, organizing shifts, or adjusting your schedule to ensure more exposure to that preceptor7. The best feedback comes from individuals that are invested in your growth and development.
Senior Editor: Dr. Alim Nagji
Junior Editors: Megan Chu and Julia Heighton
- 1.Ericsson KA, Krampe RT, Tesch-Römer C. The role of deliberate practice in the acquisition of expert performance. Psychological Review. 1993:363-406. doi:10.1037/0033-295x.100.3.363
- 2.Hattie J, Timperley H. The Power of Feedback. Review of Educational Research. March 2007:81-112. doi:10.3102/003465430298487
- 3.Maneshi A. CanadiEM. How to survive (and like) your emergency medicine clerkship core rotation. https://canadiem.org/how-to-survive-and-like-your-emergency-medicine-clerkship-core-rotation/. Published May 4, 2015. Accessed March 26, 2020.
- 4.O’Gorman C. CanadiEM. 10 Tips from Nurses to Rock Your EM Clerkship. https://canadiem.org/10-tips-from-nurses/. Published August 14, 2014. Accessed March 26, 2020.
- 5.Wade DT. Goal setting in rehabilitation: an overview of what, why and how. Clin Rehabil. March 2009:291-295. doi:10.1177/0269215509103551
- 6.Algiraigri AH. Ten tips for receiving feedback effectively in clinical practice. Medical Education Online. January 2014:25141. doi:10.3402/meo.v19.25141
- 7.May N. ST.EMLYN’S EMERGENCY MEDICINE #FOAMED. Be a better learner – Part 1. St.Emlyn’s. https://www.stemlynsblog.org/better-learning/be-a-better-learner-part-1-st-emlyns/. Accessed March 26, 2020.
Reviewing with the Staff
Requesting/getting feedback can be an extremely stressful experience but the more often you seek it the easier receiving it becomes, and the more opportunities you have to modify your behaviours and improve. Always ask specific questions like “what is one thing I could have done better in that history and physical?”. Unfortunately sometimes even though you have asked for specifics, you will still receive a vague answer from your preceptor. Follow-up with “could you explain what you mean” or “could you give me an example of how you think this could have been done better”. Especially if you work with that same preceptor again, demonstrate that you have heard their feedback by incorporating it into your next interaction. They will definitely notice this growth and be even more inclined to give you further feedback. And finally, don’t just obtain feedback from your supervising preceptor, ask the nurse who was in the patients’ room when you took a history and physical, the physician who you consulted for feedback, the patient and their family who you took care of. Every interaction has the ability to provide you with feedback if you seek it out.




