Editor’s Note:
Last Wednesday was like the night before Christmas for the BoringEM team. We had trouble getting to sleep as we awaited the Thursday release of the 2015 ILCOR / AHA / Heart & Stroke Foundation of Canada guidelines for Cardiopulmonary Resuscitation (CPR) and Emergency Cardiac Care (ECC)! We spent the prior week planning for how our team could help to translate and disseminate this material to our readers, the #FOAMed community, and around the world.
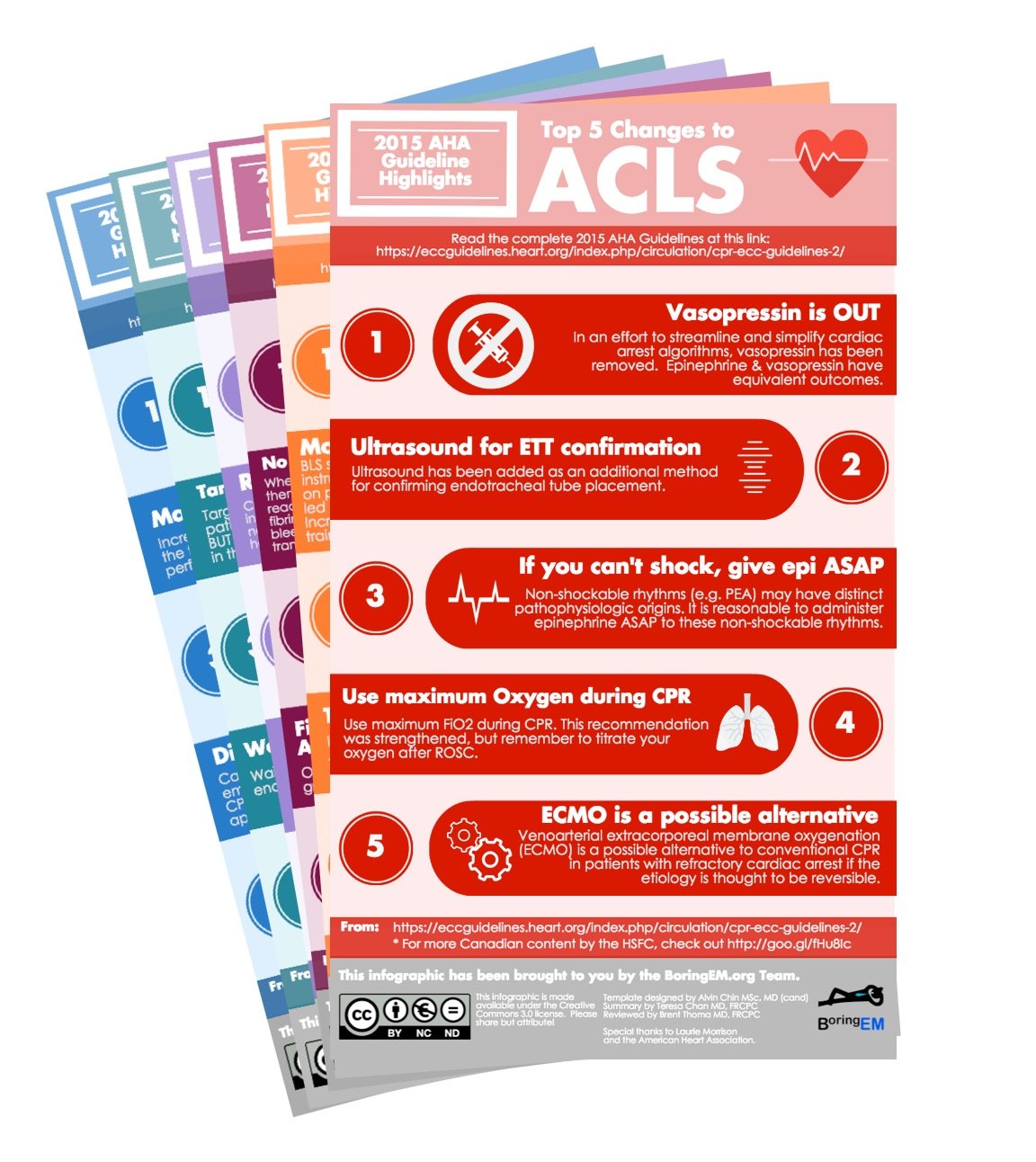
We are happy to share what we came up with today. By now, many of you have seen the results of our infographic campaign to disseminate the “Top Five Changes” from each section of the 2015 AHA Guidelines on Twitter and Facebook. Collectively, these resources have been shared and retweeted >500 times (!!) in just a few days. This blog post compiles the full collection in one place.
In keeping with our goal to help disseminate these changes as quickly as possible, we hope that you will share them either by passing this post along to your colleagues via email or social media or by printing the PDF version to paste on the walls of your hospital, ambulance bay, or hangar.
Cardiac Arrest: Why everyone should care what the 2015 AHA guidelines say
In emergency medicine, we see the sickest patients in their sickest moments. Whether you’re a respiratory therapist, registered nurse, paramedic, or physician, you have likely wondered if your resuscitation efforts are worth it; worth the time, the commitment, the money, and the emotional drain. Whether it’s moaning when someone yells “I feel a pulse!” or groaning when the patch phone rings with a “VSA 10 minutes out”, at times we all question if what we are doing right.
It’s important for us to recognize how narrow our perspective is. Patients are often comatose and unstable after a successful resuscitation and it’s easy to assume death will follow shortly after admission. However, the numbers have become more encouraging than most of us realize.
Advanced cardiac life support efforts have been described as “heroic” since the 1960’s. Researchers have trialed therapies in dogs, pigs, and people searching for a “magic bullet” – a drug, a device, a technique – that can reverse death. While defibrillation and early, high-quality CPR are often cited as “the only things that work,” the survival rates for out of hospital cardiac arrest continue to climb as we refine the ACLS algorithm. While nailing down interventions supported by P-values and confidence intervals has proven elusive, these trends indicate that we are on the right path.
Here are three points to consider the next time you’re faced with a patient in cardiac arrest:
- Cardiac arrest survival is varies from 2% to 59% depending on the rhythm (shockable or nonshockable) and where you live.
- Survival is increasing – everywhere. In Ontario, Canada survival has climbed from 4% to 10% in the last decade!
- Prognostication is hard. The guidelines now recommend waiting 72 hours before initiating exams to determine futility. Decisions to withdraw life support in the emergency department should take into account our inability to accurately prognosticate post-cardiac arrest patients in the ED. Futility is not the rule.
While many succumb to cardiac arrest, we also have survivors with remarkable stories: Children with prolonged downtimes who recover fully; middle-aged snow-shovellers who make it home for the holidays; and elderly people who survive to see the birth of a grandson or the graduation of a granddaughter. These people are the reason we dedicate ourselves to advancing the science of resuscitation; translating knowledge into practice through education, mentorship, administrative actions, and policy work; and hitting the front lines armed with two hands, two pads, and good judgment.
How high can survival from cardiac arrest go? That’s one question science hasn’t yet answered!
The Top Five Changes Project
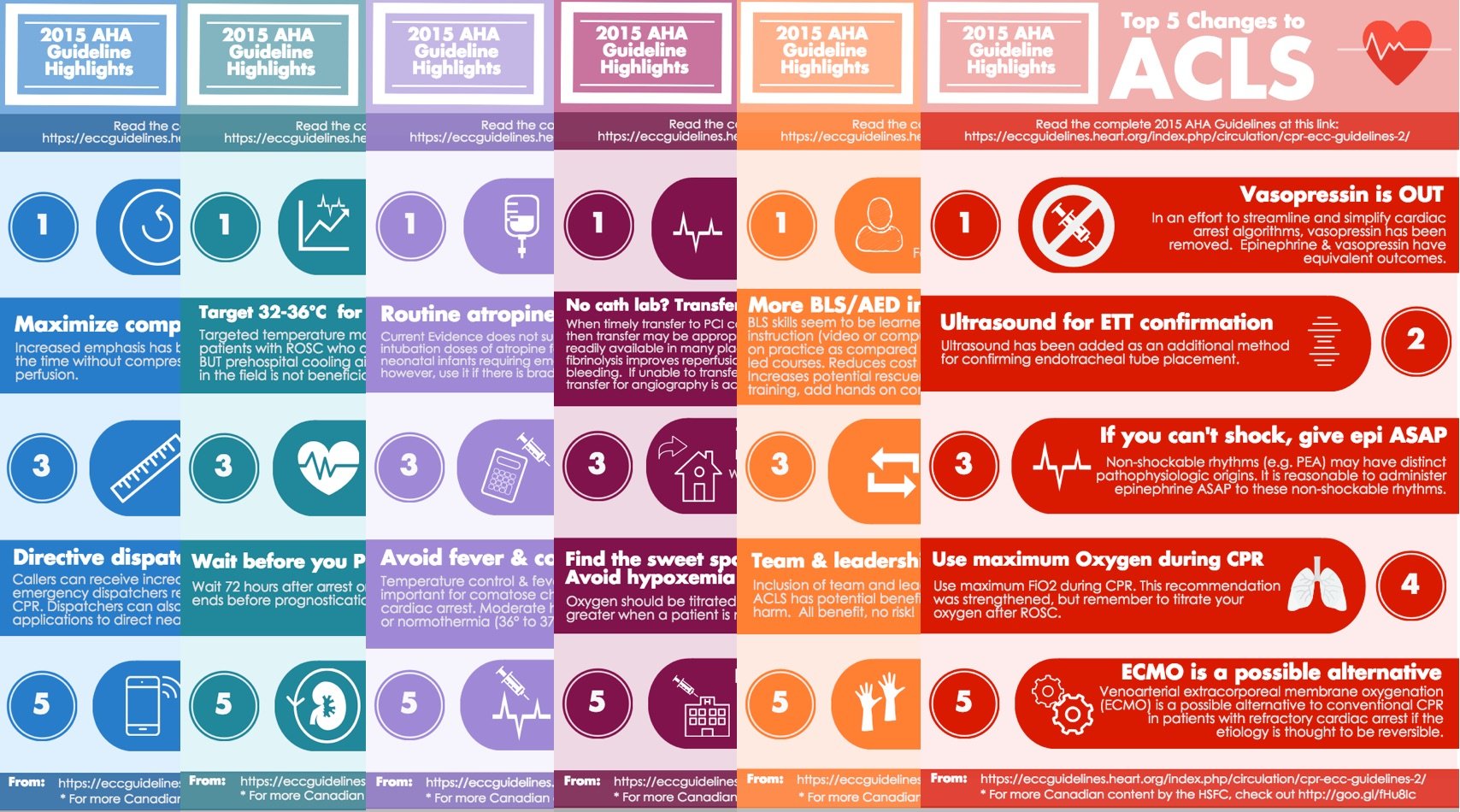
The BoringEM team believes strongly in the science and expert deliberations that resulted in the 2015 AHA guidelines. This series of infographics highlights the changes since the 2010 publication but are not meant to replace a sound understanding of the guidelines and literature, nor to fully communicate the nuances of best practices in resuscitation. We hope only that they spur those on the front lines to delve deeper into the medicine of resuscitation while hastening the translation of the best available evidence from guideline into practice.
Click on the links below to download PNG or PDF versions of each individual update infographic.
| Section | PNG Link | PDF Link |
|---|---|---|
| CPR | PNG | |
| BLS | PNG | |
| ACLS | PNG | |
| PALS | PNG | |
| ACS | PNG | |
| Special Circumstances | PNG | |
| Post-Resuscitation Care | PNG | |
| Education | PNG |
Or download all of the PDFs as a package by clicking here.
Why did we do this?
At BoringEM, we know that educators can play a key role in translating the knowledge within the pages of medical journals into actions at the bedside by creating user-friendly resources. Traditionally, this has been done using lectures, workshops, and ACLS courses… but this year we were approached by Canadian EMS / Resuscitation guru Dr. Laurie Morrison and asked to use social media to spread the word. We hope this little initiative might inspire a new wave of knowledge translation efforts for important medical literature.
Thanks to our team
Projects like these are not possible without a great team. Special thanks should be given to our writers (Blair Bigham, Sarah Luckett-Gatopoulos, Brent Thoma, Ponn Benjamin, Teresa Chan), editors (Alim Pardhan, Michelle Welsford, Teresa Chan, Brent Thoma), and designers (Alvin Chin, Teresa Chan) for putting aside other projects to concentrate on this one. Our resuscitation guru and mentor, Dr. Laurie Morrison, also deserves credit for inspiring this project.
NOTE (oct 23, 2015): A post-publication review came in from a few people re: the Special Circumstances post. The word “to” was changed to “with” in point 1, and on point 5, the term “cardiac arrest” was changed to “respiratory arrest” to fit the description for ALS providers. And now thanks for spotting the typo @SLuckettG too. Amended.