You have seen the patient, collected a thorough history of pertinent positives and negatives, completed a comprehensive physical, generated a differential diagnosis, presented the case to your attending and ordered all the appropriate investigations. The next step in providing the best care in the emergency department is reassessing, reassessing, and reassessing.
The Emergency Department is unique in that there is minimal continuity of care. Once the patient is discharged from the department you will likely no longer be involved in their care. However, on other services such as Internal Medicine, patients spend days to weeks on the ward and you are afforded the opportunity to round each day on your patient; this allows for ongoing assessments. Similarly, while on your Family Medicine rotation you may see the same patient several times over multiple weeks; this affords you the opportunity to assess how your intervention is impacting their health. The Emergency Department reassessment can be conceptualized as rounding or a follow-up appointment in a family practice. However, it occurs within the same patient interaction, over a shorter temporal period.
Four Important Questions
As a clerk completing a thorough and timely reassessment demonstrates initiative and ownership of patient care to your attending. It allows you to monitor the patient’s trajectory and intervene before they deteriorate. In a busy emergency department, it can be easy to get caught up in the new trauma that just rolled in or the patient in cardiac arrest that is 20 minutes out, but it is important to stay organized and reassess your patients. When reassessing your patients, it is important to keep the four questions in mind:
- How is my patient doing?
- Have I documented the encounter?
- Do we have a plan for appropriate disposition?
- Have I addressed all of their concerns?
How is your patient doing? The re-interview
Before presenting a reassessment to your attending physician, you first need to complete all the data collection. It is imperative to re-interview the patient to assess if their symptoms have changed and to complete a tailored physical exam. At this time, you can address the first golden rule; have you treated the patient’s symptoms. You need to assess whether the treatment plan has helped the patient. Often it can be difficult for patients to express whether their symptoms have improved or worsened. One important tool to use is the previous pain rating given by the patient in the initial history. This creates a reference point and limits recall bias, allowing you to better identify the trajectory of their symptoms. If you ask a patient “ When I first saw you, you said your pain was 7/10, how would you rate it now?”, this allows you to better identify if the analgesic has been effective or if the antiemetic has benefited the patient1.
Have I documented the encounter? How to rock your ED documentation on your reassessment
Once you have collected all the relevant information, including laboratory and radiological results, the information needs to be synthesized and documented. A “SOAP” note (Subjective, Objective, Assessment, Plan) will ensure that medico-legally you and your attending are covered but also communicate to others on the health care team what has happened in the interim with the patient. Next it is important to create an impression of the patient. The original differential should be re-visited to see which disease processes can be ruled out and which can be ruled in. Or whether a new hypothesis needs to be generated.
Attending note: The old adage is that “If a tree falls in the forest and no one was there to chart it… it doesn’t count!” All joking aside, writing a proper reassessment shows that you care about how the patient is doing, and that you are trending their progress. Remember to date and time the new note; similar to other services, we need to demonstrate we are “rounding” on our patients again – usually about every 1-2 hours to move the mark on something in the patient’s life. If the patient is unstable you will see that your residents and attending physicians will often round more often on the patient (e.g. every half hour, or even more frequently). Sometimes it will be to give more pain meds, sometimes it will be to make a disposition decision based on new labs or imaging results.
Do we have a plan for appropriate disposition?
Next you need to address the final golden rule; do I have an appropriate disposition for my patient. After considering all the data points and reviewing the goals of the patient and the most likely diagnosis, it is important to determine a final destination for your patient. Are they safe to go home, will they need follow-up as an outpatient, or will they need to be admitted under a hospital service.
Have I addressed all their concerns? Asking about and addressing your patient’s fears
When collecting new information, you should keep in mind the second golden rule: “Have I addressed the patient’s concern?” Your agenda may widely vary from the concern and goals of your patient. Always keeping in mind the wise old question, why now, why today, why has this patient decided to seek emergent care.
Often it can be because they once read an article that gastric cancer often can present with shooting abdominal pain, or they knew someone who ignored the same symptoms and ended up dying one week later. If you do not address their concerns then you will have done a disservice to your patient and it may lead to repeated emergency department visits.
Attending note: You may not be able to take care of these concerns on your own – and in fact, many patients will want to hear things from your supervising attending emergency physician. That is okay! Remember, your job is to gather the questions that you want answered, and then bring your attending into the mix. Remember that being patient centered is key.
Rules of the Reassessment
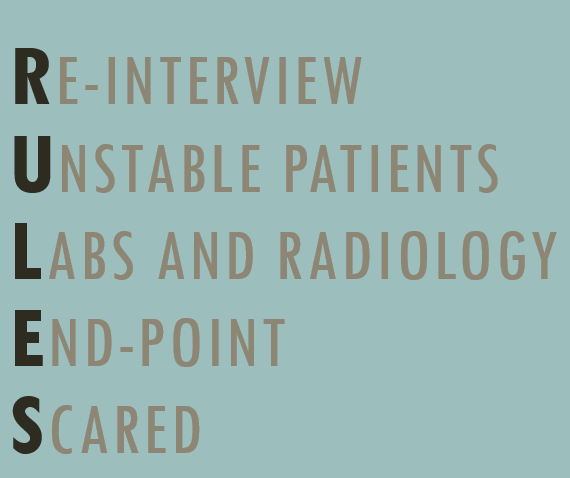
Seeing patient after patient it can be easy to forget about the reassessment. However, if you utilize the breaks and downtime in your shift then you can master the reassessment. If your staff is busy with a procedure, reviewing with a resident, or you find yourself with ten minutes of alone time it is important to run through the RULES mnemonic for each patient you are following.
First, it is important to Re-interview patients to assess if their symptoms are improving or worsening. Such as the patient with a 9/10 migraine who was given pharmacological analgesia or the seven-year-old with gastro who was given antiemetics and IV fluids. This is an opportunity to trial a new intervention, if the previous management strategies haven’t been working.
If there are any patients you are worried about that may become Unstable, it would be worthwhile to review their vitals and perform another physical exam.
Next, you should check if any Labs or radiology reports have returned for your patient. Perhaps that d-dimer is negative on your possible pulmonary embolism or the head CT for the patient whose head trauma demonstrates an intracranial bleed.
As you begin to collect new data it is important to determine an End-point. Perhaps all the investigations on a particular patients have returned and all the emergent pathologies have been ruled out and they can go home. Conversely, perhaps you clearly identified worsening chronic kidney function in a patient that led to a congestive heart failure exacerbation and the patient can be referred to internal medicine.
Finally, have you addressed what the patient is most Scared about; it is important to understand the patient’s concerns and answer any questions they may have to ensure continuity of care. Utilizing each break to consider what needs to be done and who needs to be seen again will make your reassessments run smoothly.
Wrapping Up
The final step involves presenting the reassessment. A high level summary of the patient’s chief complaint and symptoms should be provided, including all the previously discussed components. Connecting the information collected during the reassessment, with the initial history and differential will allow you and your attending to confirm or dispute your working diagnosis2.
Completing a thorough and timely reassessment in the emergency department is critical to identify deteriorating patients. It also allows lower acuity patients to be seen and discharged quickly so other patients can be seen in a timely manner. Often patients will require multiple reassessments throughout a shift, which can be helpful when there is a lot of new information for the patient to digest or your patient is quite anxious. The key is to address the three golden rules; allowing for better patients outcomes and fewer bounce backs in the emergency department3.
This post was edited and uploaded by Megan Chu.
- 1.Crystal M. Self-Reported Pain Scales. Don’t Forget the Bubbles. https://dontforgetthebubbles.com/self-report-pain-scales/. Published February 19, 2018. Accessed March 26, 2020.
- 2.Maneshi A. How to survive (and like) your emergency medicine clerkship core rotation. CanadiEM. https://canadiem.org/how-to-survive-and-like-your-emergency-medicine-clerkship-core-rotation/. Published May 4, 2015. Accessed March 26, 2020.
- 3.Nickson C. Managing the Emergency Department . Life in the Fast Lane. https://litfl.com/managing-the-emergency-department/. Published March 21, 2019. Accessed March 26, 2020.
Reviewing with the Staff
I’ve jotted some thoughts down alongside Arthur’s wonderful piece as I was editing it. This is definitely a post I would have wanted to read when I was getting started in emergency medicine. I didn’t even KNOW that we had to reassess patients well into my clerkship, but it totally makes sense when you think about it… We have some of the most rapid testing, most immediate response times, and sometimes the sickest patients in the hospital - we should be trying to move the mark every few hours to ensure we are taking care of them well.
Most lengths of stay are around 4-6 hours, and so within that time we should aim to see our patients and talk to them once more. As someone who has been a patient, those 2-3 hours between the times you see the physician can seem excruciatingly long… so having a smiling, friendly face of a clinical clerk checking on you once in a while is a welcome sight.



