How to use this section?
- This is a quick refresher on ECGs commonly seen in the ED. We have provided one-liner introductions to each, and the answers are below the ECG. For those looking for a challenge, cover up the answer and quiz yourself.
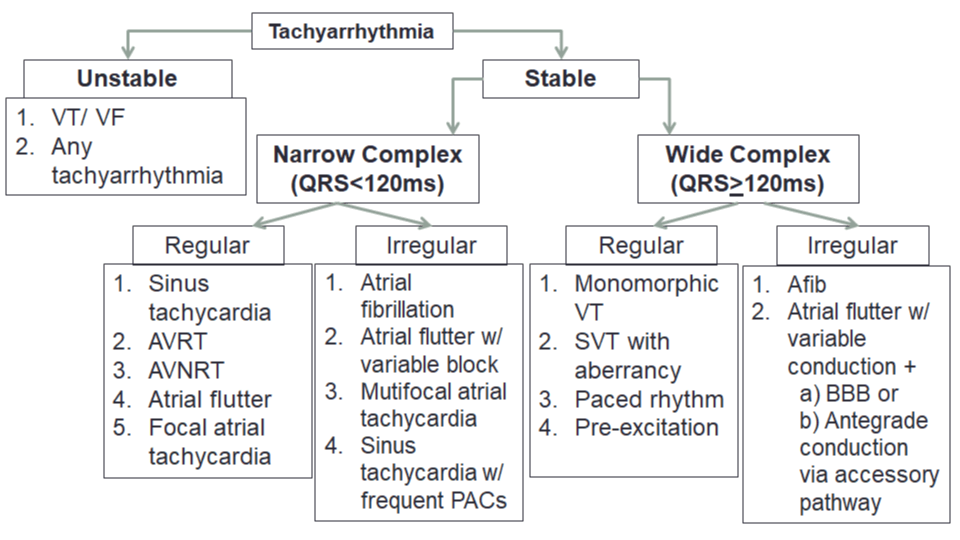
1. ECG – Tachyarrhythmias
ECG Cases Questions – What is the ECG and your next step?
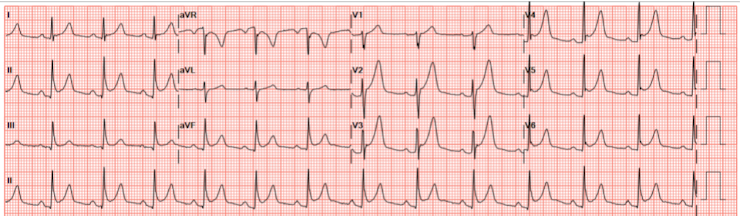
[bg_faq_start]Case 1
25-year-old male. Feels very anxious watching the news. Very worried he is going to get COVID-19. The redeployed nurse from the pediatric ward apologizes profusely for the wandering baseline, but that is the best ECG they could get because the patient is very anxious.

Answer
Interpretation: Sinus Tachycardia
Key Features: HR>100 BPM, Normal P wave morphology (P wave upright in I and II)
What is your next step: Determine the underlying cause of tachycardia and treat the underlying cause.
Case 2
38-year-old female was out for a jog, sudden felt palpitations. Tried vagal maneuvers herself, but it didn’t resolve. Continued jogging to the ED.

Answer
Interpretation: Supraventricular tachycardia – differential diagnosis includes AVNRT or AVRT
Key Features: Narrow complex, regular tachycardia – HR 180bpm
What is your next step: Try a vagal maneuver (carotid sinus massage or Valsalva maneuver) if vagal maneuver does not work, try adenosine (6 or 12 mg IV push).
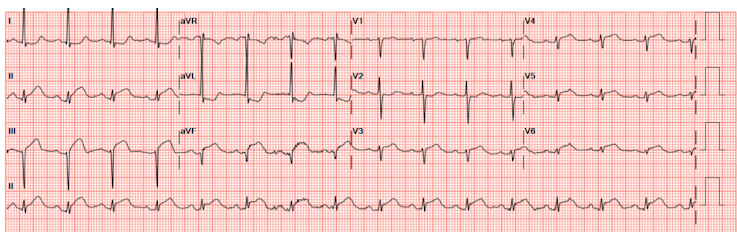
Case 3
87-year-old female. Here in ED with a dry cough, worried about COVID-19. Also, ran out of her warfarin recently.

Answer
Interpretation: Atrial fibrillation
Key Features: Irregularly irregular rhythm with no P waves
What is your next step: Determine time of onset. Choose between rate control or cardioversion (electrical or chemical). Stroke Prevention: use CCS CHADS65 to determine what antithrombotic to prescribe.
Case 4
55-year-old male. Palpitations and lightheadedness.

Answer
Interpretation: Atrial Flutter with 2:1 conduction
Key features: Narrow complex, regular tachycardia. F waves (flutter waves).
What is your next step: If unstable, cardioversion. If unsure if this is AFlutter or SVT, may trial a dose of adenosine, which will show underlying sawtooth pattern. Otherwise, treat similarly to atrial fibrillation. Chose between rate control or cardioversion (electrical or chemical) – CCS algorithm
Stroke Prevention: Use CCS CHADS65 to determine what antithrombotic to prescribe.
Case 4b
Same 55-year-old male from last ECG. Recently prescribed metoprolol for his “heart condition” and now feels light headed when rising quickly.

Answer
Interpretation: Atrial Flutter with 4:1 conduction
Key features: Narrow complex, regular tachycardia. F waves (flutter waves).
What is your next step: If unstable, cardioversion. If unsure if this is AFlutter or SVT, may trial a dose of adenosine, which will show underlying sawtooth pattern. Otherwise, treat similarly to atrial fibrillation. Chose between rate control or cardioversion (electrical or chemical) – CCS algorithm
Stroke Prevention: Use CCS CHADS65 to determine what antithrombotic to prescribe.
Case 5
72-year-old male with extensive cardiac history. He has been feeling weird palpitations in his chest and wants it checked out.

Answer
Interpretation: Pre-excited atrial fibrillation
Key Features: “wacky tacky” irregularly irregular rhythm. QRS width varies between narrow and wide.
What is your next step: Unstable – cardiovert. If stable – procainamide. Perform ECG when in sinus rhythm to confirm the patient has pre-excitation (delta waves). Consult cardiology.
Case 6
65-year-old male with history of psychiatric disorder was recently prescribed levofloxacin for his bacterial pneumonia. He now presents feeling worse.

Answer
Interpretation: Torsades de pointes
Key Features: Polymorphic ventricular tachycardia secondary to long QT.
What is your next step: Unstable – cardiovert. If stable – give Magnesium Sulphate, correct electrolyte abnormalities, stop all QT-prolonging medications, consider overdrive pacing. Consult cardiology.
Case 7
45-year-old male. Unconscious. BP 75/45. COVID-19 positive.

Answer
Interpretation: Ventricular tachycardia
Key Features: Wide complex, regular tachycardia. The presence of a capture beat confirms that this is ventricular tachycardia.
What is your next step: If there is a pulse – synchronized cardioversion. If no pulse – start CPR, defibrillate, and follow ACLS algorithm. Consult cardiology.
Recommended Reading, Videos, and Podcasts
2. ECG – Bradyarrhythmias
This review is all about differentiating really slow rhythms. Remember, SOME asymptomatic bradycardias can be managed as an outpatient.

ECG Cases Questions – What is the ECG and your next step?
[bg_faq_start]Case 1
75-year-old from retirement home. Had syncopal event today. Has been feeling lightheaded for 2 weeks, but didn’t want to cause a big scene because of all the COVID-19 stuff.

Answers
Interpretation: Second degree AV block (2:1 block). HR 30 bpm.
Key Features: Every other P wave is not conducted.
What is your next step: Consider isoproterenol infusion. External pacing if unstable. Consult Cardiology.
Case 2
63-year-old male. Has been feeling really dizzy.

Answers
Interpretation: Complete heart block.
Key Features: AV dissociation (P-waves separate from the QRS complexes). Wide complex escape rhythm with right bundle branch block morphology.
What is your next step: Consider isoproterenol infusion. External pacing if unstable. Consult Cardiology. Placement of a transcutaneous transvenous pacemaker may be warranted.
Recommended Reading, Videos, and Podcasts
- CanadiEM The Boring Guide to ECG’s: Fascicular blocks
- CanadiEM Medical Concept: ECGs in Syncope
- CanadiEM Management of Hyperkalemia with ECG Changes
- CanadiEM Pacemaker Essentials: How to Interpret a Pacemaker ECG
- Natalie’s Casebook (CAUTION British Resource)
3. ECG – ST Abnormalities
This review is all about spotting ST- and T-wave changes.
ECG Cases Questions – What is the ECG and your next step?
[bg_faq_start]Case 1
47 year-old male with left sided retrosternal chest pain, which resolves a bit with nitro spray.

Answer
Interpretation: High-risk NSTEMI (consider left main stenosis or triple vessel disease)
Key Features: Diffuse ST Depression with AVR elevation
What is your next step: Acute coronary syndrome treatment (ASA< Plavix, anticoagulation), consider nitroglycerin and beta-blocker. Consult cardiology/internal medicine.
Case 2
39-year-old male. Has had this before, was on Colchicine last time.
Answer
Interpretation: Pericarditis, a STEMI mimic
Key Features: Diffuse ST elevation. Diffuse PR depression.
What is your next step: High dose NSAIDs or ASA are first line. Colchicine x 3 months may also be warranted to prevent complications. Consider adding a proton pump inhibitor (PPI) to prevent gastrointestinal bleeding with high dose NSAIDs. Outpatient Cardiology consult for follow-up and echocardiogram to assess for pericardial effusion.
Case 3
75-year-old male. Was cutting his lawn by herself this morning. Felt some heaviness in hisPart chest that has not been relieved by his wife’s nitro spray.
Answer
Interpretation: Inferolateral STEMI
Key Features: ST elevation in the inferior and lateral leads with reciprocal ST depressions in I and AVL.
What is your next step: Consult interventional cardiologist. Consider primary PCI or thrombolysis. If thrombolysis is chosen, consult local protocol and determine if patient has any contraindications to thrombolysis.
Case 4
56-year-old female. Has been having indigestion all morning. Which is odd because she didn’t have anything abnormal.

Answer
Interpretation: Anterolateral STEMI
Key Features: ST elevation in V1-V3, I, and AVL. Reciprocal ST depression in the inferior leads. Poor R wave profession. Sinus tachycardia. Left axis deviation.
What is your next step: Consult interventional cardiologist. Consider primary PCI or thrombolysis. If thrombolysis is chosen, consult local protocol and determine if patient has any contraindications to thrombolysis.
Interested in more?
The following is part of the CanadiEM Frontline Primer. An introduction to the primer can be found here. To return to the Primer content overview click here.
This post was copyedited and uploaded by Johnny Huang.
Font heading for “Cases X” has to be H3 for Drop-down menu to work




