The Case
A 25-year-old woman presents with diarrhea x 3 weeks. She has reports 6-12 loose bowel movements per day with urgency and mucous which are associated with cramping abdominal pain and a 5lb weight loss. She has not noticed any blood in her stool and reports no other extra-intestinal manifestations of inflammatory bowel disease (IBD). She has not travelled recently and drinks out of a municipal water supply. None of her contacts have similar symptoms and she has had no changes to her diet. She has no family history of IBD but does have a family history of a variety of autoimmune conditions. She is otherwise healthy and has had no recent contact with the health care system or use of antibiotics. Her vital signs are normal, she looks well and her abdominal exam is normal.
You suggest basic blood work (including a CBC, electrolytes and ESR), stool cultures and a GI consult. Your staffman asks, “were there any fecal leukocytes?”.
You stare back blankly.
What are Fecal Leukocytes?
Exactly what they sound like – white blood cells in liquefied poop. They can represent an inflammatory cause of diarrhea (acutely from infection or from an initial presentation of inflammatory bowel disease). Fecal leukocytes can be found in patients with shigellosis, salmonellosis, typhoid fever, invasive E. Coli colitis, C. Difficile, ulcerative colitis and Crohn’s disease. Leukocytes are not typically seen in viral gastroenteritis.
How do you find them?
- Get a sample of the patient’s diarrhea.
- This is sometimes in and of itself a useful test. I find it a helpful piece of information if a patient with a chief complaint of diarrhea has been in the ED for 6-8 hours and is unable to provide a stool sample or passes fully formed stool.
- Look at it – yes this is admittedly gross but can be helpful.

- Do you see mucous, frank blood? Where does it lie on the Bristol stool chart? You can even have the patient download a Bristol stool chart app to collect longitudinal data on their bowel movements between when you see them in the ED and their GI appointment down the road!
- Get your methylene blue.
- If you are like my preceptor you will have to go no further than your briefcase to find this handy-dandy diagnostic tool.
- You can usually procure a small vial from your hospital lab for no cost.
- Stain the diarrhea
- Use a cotton swab or small pipette to put a small sample of representative diarrhea on a glass slide.
- Add one drop of methylene blue to the diarrhea, mix and let sit a minute.
- Gently smear the mixture to create a thin, translucent layer then cover with a thin plastic cover slip.
- Put it under the microscope
- Wipe off the dust from the scope in your department (so true)
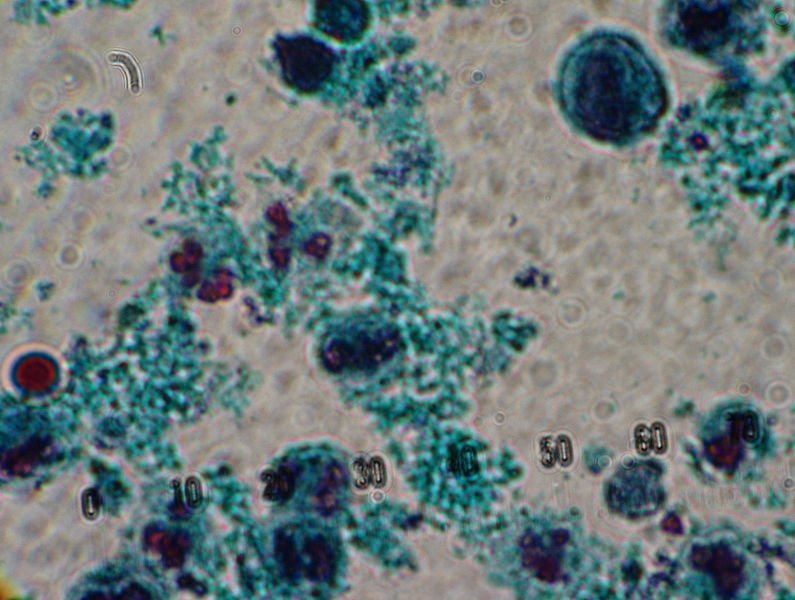
- Put the slide in and check for stained leukocytes. Even to the untrained, microscope challenged eye (me) they pop out! Did I mention that I failed the microscopy course of my science class in grade 10?
What is the Evidence?
The evidence really has to be divided into two categories
Acute – infectious
Overall the sensitivity is not fantastic but the specificity is decent.
A 2003 systematic review including 14 studies performed a meta-analysis to determine the test characteristics of fecal leukocyte staining among other stool tests for an invasive cause of acute diarrhea [1]. A threshold of 5 leukocytes/high power field was used. Importantly, this review stratified evidence between developed and resource-poor countries. This is key in the investigation of diarrhea because the culprit causes vary greatly in these two circumstances. There was a heterogenous distribution of sensitivities and specificities in both groups but seemed to be more precise in developed setting.
| Practice Setting | Sensitivity | Specificity | (-) Likelihood Ratio | (+) Likelihood Ratio |
| Developed (6 studies) | 0.73 (0.33-0.94) | 0.84 (0.50-0.96) | 0.32 | 4.56 |
| Resource poor (8 studies) | 0.50 (0.33-0.67) | 0.83 (0.74-0.89) | 0.60 | 2.94 |
Initial Presentation of Inflammatory Bowel Disease
I had difficulty finding and recent specific studies or reviews evaluating the test characteristics of fecal leukocytes in inflammatory disease diarrhea but since all of the assays being developed (lactoferrin, PMN-e and calprotectin) are surrogates for fecal leukocytes it seems fair to assume that they are an important prognostic factor for GI docs. In fact, a quick survey of the twitterverse showed that a few gastroenterologists would consider expediting a referral for patients with documented fecal leukocytes.
The “bottom” line
The test is easy to do and the presence of fecal leukocytes adds evidence to your case. This is really only applicable to outpatient diarrhea in the immune-competent, adult patients who have not had recent contact with hospitals/antibiotics.
The presence of fecal leukocytes will not make the diagnosis but will increase the likelihood that diarrhea is caused by “badness”. This may affect your decision to treat the acute diarrhea with antibiotics, while stool culture is pending or if this information is included in a referral note for the chronic diarrhea patient, it may expedite the referral to GI for a more thorough work up for inflammatory bowel disease.
The absence of fecal leukocytes is less helpful and depending on the clinical history should not prevent you from obtaining a stool culture and submitting a referral to your gastroenterology doctors as necessary.
Other Testing Options
There is some evidence that screening stool for lactoferrin and calprotectin (especially in chronic diarrhea) may be a more sensitive test for detecting inflammatory diarrhea though these tests are largely not covered by provincial health plans and as such are impractical for routine use in the ED[2].
Testing diarrhea for occult blood can again help add information to the clinical picture but is not impressively sensitive or specific.
Your best bet is to chat with your friendly neighbourhood gastroenterologist to see what is most useful for them to triage cases.
Back to the Case
Your staff shows you how to test for fecal leukocytes, which you identify on the smear! Her ESR was mildly elevated and the rest of her blood work was normal. You do send the diarrhea for culture and decide to discuss the case directly with GI. You mention the positive fecal leukocyte test and in the context of her history GI decides to see her in their urgent IBD clinic. She has a scope one week later with biopsies consistent with Crohn’s colitis.
[bg_faq_start]References
- Gill, C. J., Lau, J., Gorbach, S. L., & Hamer, D. H. (2003). Diagnostic accuracy of stool assays for inflammatory bacterial gastroenteritis in developed and resource-poor countries. Clinical infectious diseases, 37(3), 365-375.
- Pardi, D. S., & Kelly, C. P. (2011). Microscopic colitis. Gastroenterology, 140(4), 1155-1165.
Additional Resources
- Thielman, N. M., & Guerrant, R. L. (2004). Acute infectious diarrhea. New England Journal of Medicine, 350(1), 38-47.