The Case
A 26 year old female presents with acute vision loss. The patient states her symptoms have been getting progressively worse over the last week, and she feels her color vision is “a little wonky.” It didn’t concern her too much until she had to run out of the sauna today because of extreme pain and foggy vision in her right eye.
What is Optic Neuritis?
Optic neuritis is inflammation of the optic nerve. It typically presents with loss of vision, dyschromatopsia (color vision impairment) and ocular pain.
On history, patients may describe changes in their colour vision. This is demonstrated with the ‘red desaturation test’ where a patient is asked to look at a dark red object with one eye. The affected eye will see the object as pink or light red. The patient will have a normal fundoscopic exam, but a positive Marcus Gunn pupil on Relative Afferent Pupillary Defect (RAPD) test (swinging-light test where the pupils will constrict less and appear to dilate, when a bright light is swung from the unaffected to the affected eye). Uhthoff’s phenomenon is a worsening of neurologic symptoms of MS when the body’s temperature rises – such as exercising, using a sauna or on a hot day, and patients may find that warm temperatures cause worsening vision and pain.
In young adults, optic neuritis is the most common cause of acute unilateral visual loss, with an incidence of 1-5 in 100,000 every year. Women between the ages of 15 and 49 are the most frequently affected. Most cases of optic neuritis are idiopathic and categorized as idiopathic inflammatory demyelinating diseases, but it is important to recognise that optic neuritis is strongly associated with multiple sclerosis. Approximately 50% of patients diagnosed with optic neuritis will develop multiple sclerosis within 15 years.
What is the approach and differential of acute vision loss?
A helpful approach to vision loss starts by differentiating painful from painless visual loss. This will guide your differential and investigations.
| Acute visual Loss – WITHOUT Pain | Acute visual loss – WITH Pain |
| Lens changes, post trauma | Optic Neuritis |
| Vitreous hemorrhage | Papilledema |
| Posterior uveitis | Corneal abrasion |
| Acute maculopathy | Keratitis |
| Retinal detachment | Corneal edema |
| Retinal artery/vein occlusion | Hyphema |
| Ischemic optic neuropathy | Anterior Uveitis |
|
| Endopthalmitis |
| Lens dislocation, causing acute glaucoma |
History
A thorough history, focusing on differentiating features among conditions, can guide you to an appropriate diagnosis.
With ophthalmological complaints, important historical features include:
- Medications
- Past Medical History – vascular conditions, recent eye surgery
- Contact lenses
- Timing — sudden onset versus gradual
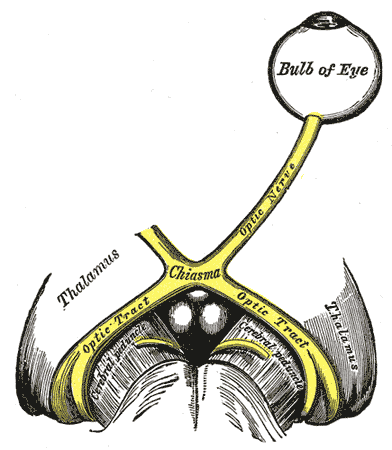
- Laterality — Bilateral loss suggests a retrochiasmal visual pathway disorder such as pituitary tumours. Monocular loss may suggest retinal detachment, ischemic optic neuropathy or central retinal vein occlusion/central retinal artery occlusion.
- Quality — Peripheral versus central visual loss (suggesting macular abnormalities)
- Pain — See table above for painful vs painless acute visual loss.
- Conjunctival erythema — found in patients with keratitis, corneal abrasions, cute glaucoma and uveitis.
- Associated symptoms:
- – homonymous defects post stroke
- – Nausea and vomiting associated with elevated intracranial pressure
- – Difficulty with balance / depth perception associated with a neurological insult (posterior stroke)
- History of trauma:
- Mild – keratitis or uveitis
- Severe – Hyphema, vitreous haemorrhage, cataract, retinal detachment, ruptured globe with sharp or blunt object injury
- Refractive error
What should be done on physical examination?
[bg_faq_start]Full ophthalmological exam: Three part video series from Academic Life in Emergency Medicine (ALiEM):
Part 1 – Eye Exam Introduction: Eye Exam Introduction
Part 2 – Visual Acuity Exam: Visual Acuity
Part 3 – Using a Slit Lamp: Slit Lamp
Full Neurologic exam: 3 minute neurologic exam video: Neuro Exam
[bg_faq_end]What lab investigations, imaging, or interventions may be necessary?
- Erythrocyte Sedimentation Rate (ESR)
- Antinuclear-Antibody (ANA)
- MRI
- Lumbar Puncture (in some cases).
What is your disposition and treatment?
The patient in our case appears to be exhibiting signs and symptoms of optic neuritis. An astute emergency physician will remember the findings of the Optic Neuritis Treatment Trial and will start IV methylprednisolone followed by a tapering course of oral prednisone accelerating visual recovery by a few weeks. She will need to be admitted for an expedited workup, which includes an MRI, LP and neurology consult. To help speed restoration of her vision and delay MS development, treatment will consist of IV methylprednisolone 1g per day and 11 days of oral prednisone at 1mg/kg per day with a taper of oral prednisone.
[bg_faq_start]References
- Tintinalli’s Emergency Medicine Manual 7the edition, page 739 to 752
- Clinical Emergency medicine LANGE
- Voss, E., Raab, P., Trebst, C., & Stangel, M. (2011). Clinical approach to optic neuritis: pitfalls, red flags and differential diagnosis. Therapeutic Advances in Neurological Disorders, 4(2), 123–134. http://doi.org/10.1177/1756285611398702
- Uptodate article: Optic neuritis: Pathophysiology, clinical features, and diagnosis
- Optic Neuritis Treatment Trial Information
- Beck, R., et al. (1992). A randomized Controlled Trial of Corticosteroids in the Treatment of Acute Optic Neuritis. New England Journal of Medicine, 326, 581-588. http://www.ncbi.nlm.nih.gov/pubmed?term=1734247