As part of the Arts PRN series, we will intermittently be featuring pieces of historic art that hint at an underlying medical condition. They say a picture is worth 1000 words… can you Spot the Diagnosis after examining only a painting? Read on to learn not only about the art, but about these fascinating medical conditions. Who knows, maybe they’ll help you make a diagnosis some day (or at least help you out on Jeopardy)! After you read, consider submitting your own art to the Arts PRN Project.
This week’s Spot the Diagnosis series features two works by Peter Paul Rubens, a Flemish artist of the Baroque period. These two exquisite paintings feature the same woman around three years apart. At first glance, she is a fair woman whose sweet smile and doe-like eyes are sure to capture every viewer’s attention. Below is a painting of her three years later. With the two paintings together, can you come up with a diagnosis?

Susanna Lunden, Rubens (1625-28)
What condition does this woman have?
This woman has a features of hypothyroidism. In the first painting, she is slim but you cannot see her sternocleidomastoid muscles originate from the clavicles – which points to the findings of a goitre.1 She is also very pale and appears to have gained significant weight from the first painting to the next, which albeit were the beauty standards of the time, are also clinical manifestations of hypothyroidism.
For the most part, thyroid disorders are insidious, slow-progressing conditions that can be managed in the outpatient setting. However, in rare circumstances, thyroid disorders may worsen and become medical emergencies.

Goitre1
The two main thyroid emergencies are myxedema coma and thyroid storm. Myxedema coma occurs when there is severe hypothyroidism, and is often precipitated by illness. Thyroid storm, on the other hand, manifests when excess thyroid hormones lead to decompensated thyrotoxicosis.2
Myxedema coma
What precipitates myxedema coma?
Myxedema coma more commonly presents in elderly patients.2 It is often precipitated by illness, such as infection, congestive heart failure or cerebrovascular accident. Cold weather, trauma and sedative medications are also known triggers. Patients with myxedema coma frequently have a thyroidectomy scar, previous radioiodine therapy or hypothyroidism.3
What are the clinical manifestations of myxedema coma?
The cardinal features of myxedema coma are decreased or altered level of consciousness and profound hypothermia. Other manifestations include hypotension, bradycardia and hypoventilation. Patients may present with “myxedema madness,” which is an altered mental status that includes delirium and hallucinations. There may also be other symptoms of hypothyroidism including hyporeflexia, dry skin, and macroglossia.2
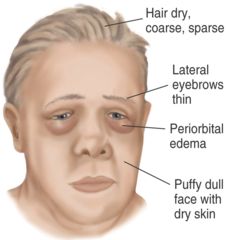
Facial findings of hypothyroidism4
Serum TSH, free T4, and cortisol levels should be obtained if myxedema coma is suspected. An elevated TSH is associated with primary hypothyroidism, while a normal or lowered TSH occurs with secondary hypothyroidism. Serum T4 levels are usually very low. Cortisol is obtained to detect concurrent Addison’s disease, which is a common comorbidity of certain thyroid disorders.2 Other possible lab findings include anemia, hypercapnia, hypoxemia, hyponatremia, and hypoglycemia.3
What is the treatment for myxedema coma?
Airway and ventilation are the most important supportive measures for myxedema coma. Patients with lowered level of consciousness and hypoventilation are unable to protect their airways and become hypercapnic, so mechanical ventilation and ICU admission are usually necessary measures.2
Typically, a combination of T3 and T4 is used to treat myxedema coma, though there is significant controversy over the optimal treatment regime. T4 has a slow onset of action (8-14 hours) as it is converted to T3 in the periphery, while T3 acts within 2-3 hours. However, T3 causes unpredictable fluctuations in serum T3 when used alone and is associated with higher mortality.2 Serum T3 and T4 levels should be monitored frequently to ensure therapy is effective.3
Glucocorticoids should be given empirically until adrenal insufficiency is ruled out. This can improve many of the associated abnormalities such as hypotension, hypoglycemia and hyponatremia.3
Finally, supportive measures including IV fluids, hypertonic saline, glucose, warming blankets and more should be used to correct hypotension, metabolic disturbances and hypothermia.3
Thyroid storm
What precipitates thyroid storm?
Thyroid storm can be precipitated by surgery, trauma, iodine therapy, and childbirth. In patients with Grave’s disease or toxic multinodular goiter, non-compliance with anti-thyroid medication can also lead to thyroid storm.3 The most common precipitant in hospitalized patients, however, is infection.2
What are the clinical manifestations of thyroid storm?
Thyroid storm typically presents with a hyperpyrexia, tachycardia and hypertension with a widened pulse pressure (may become hypotension if the patient develops shock). Patients may also experience altered mental status, including agitation, delirium, psychosis and coma. Arrhythmias, congestive heart failure and myocardial ischemia are some of the potential cardiovascular consequences of thyroid storm. Other symptoms are diaphoresis, tachypnea, dyspnea, nausea, vomiting, diarrhea and jaundice.5
Thyroid storm is a clinical diagnosis, as thyroid hormone levels are unreliable for predicting severity of disease. The Burch Wartofky Point scale can be used to determine the likelihood of thyroid storm.6
What is the work-up for thyroid storm?
Patients with thyroid storm have high free T3 and T4 levels, but at the same level as decompensated hyperthyroidism. Hence, thyroid hormone levels cannot be used to determine condition severity. TSH level is low in primary hyperthyroidism.3 Other lab findings include hypercalcemia (increased bone resorption), leukocytosis with left shift, hyperglycemia (increased glycogenolysis), and elevated liver enzymes (reduced hepatic function).2
What is the treatment for thyroid storm?
Thyroid storm should be treated with multiple drugs that target different mechanisms. Beta blockers are used to inhibit excess sympathetic activity, reducing cardiac workload. Thionamides (e.g. propylthiouracil, methimazole) are used to inhibit thyroid hormone synthesis. Potassium iodide solution blocks thyroid hormone release, but must be given one hour after thionamide to prevent the iodine from being used for thyroid hormone synthesis. Steroids can reduce peripheral conversion of T4 to T3 and treat potential adrenal insufficiency.2
Finally, supportive care such as IV fluids, acetaminophen, and dextrose may also be used. Aspirin, on the other hand, must be avoided as it can enhance conversion of T4 to T3. Any underlying infection should be identified and treated accordingly. Depending on severity, patients may require ICU admission. Definitive therapy such as radioiodine or thyroidectomy can prevent future decompensation from hyperthyroidism.56
[bg_faq_end]For more from the Spot the Diagnosis series, check out our other posts:
Spot the Diagnosis: The case of the Ugly Duchess
Spot the Diagnosis: The case of the Recluse


