Thank you to all those who contributed to the discussion in Episode 1 of The Case of the Missing Awake Intubation Kit. In Episode 2, I compile the feedback from the first part of the series and some pearls from a discussion with local airway expert, Dr. Nick Kuzak. I have also included advice and instruction from emergency physicians Drs. Paul Linden and Nick Balfour, both qualified AIME (Airway Intervention and Management in Emergencies) course instructors.. This series is about the logistical challenges of not having a ready awake intubation kit, and a call for input from the social media community. – Jared
As Mario Francispragasam acknowledged in his comment on our original article, ‘not all awake intubations are the same, and not all operators are the same’. With that in mind, we consulted local experts Drs. Nick Kuzak, Paul Linden, and Nick Balfour. We have compiled both their thoughts and those from the comments made in Part 1 to devise a proposed awake intubation kit.
Dr. Nick Kuzak is one of our local cardiac anesthesiologists dual certified by the Royal College of Physicians and Surgeons of Canada in Emergency Medicine and Anesthesiology. He also completed a fellowship in cardiac anesthesia. He was kind enough to meet with me on two separate occasions to discuss his recommendations for an awake intubation kit. We also dug through the supply room to see what is available in our shop.
Based on our discussion, the best way to approach putting together a kit is to break it down into the key components required for awake intubation:
- Systemic medications – Important for sedation, anxiolysis, managing secretions, and preventing emesis.
- Tools and medications for topicalization of the airway – Important for minimising glottic closure, cough, and gag reflexes [1].
- Equipment – Required for visualization of the larynx and intubation of the trachea
It is prudent to have back-up equipment available for any attempt at advanced airway intervention. This should include a bag valve mask with PEEP, nasal prongs, an alternate intubating device, an extraglottic airway device for rescue above the cords, and a cricothyrotomy kit for rescue below the cords.
Disclaimer: All of the medications and pieces of equipment listed above are our best attempt to cover a wide range of necessary items in a kit that would apply to the vast majority of awake intubation scenarios in the emergency department. This was based on expert opinion both locally and through the FOAMed world, and a review of the relevant literature. The indications for awake intubation, and the particular approach, will vary among centres and practitioners. Choice of tools will also vary. The products mentioned in this article are just a sampling of what is available. None of the proprietary names mentioned equate to an endorsement or recommendation of that particular product. For an approach to awake intubation, see the EMCrit and emupdates articles in our reference section [2, 3, 4].
Systemic medications for an Awake Intubation Kit
a. Glycopyrrolate (Antisialogogue)
Decreases airway secretions through anticholinergic action [3]. Dose range is 0.2-0.6 mg IV push. This should be administered 10 to 15 minutes prior to awake intubation.
b. Dexmedetomidine (Sedative)
This medication is touted by Dr. Nick Kuzak as the go-to for awake intubation sedation. It is a highly-selective alpha-2 agonist with anxiolytic and analgesic properties [6]. A recent study in the Journal of Anesthesiology [1] found that patients were less likely to remember their intubation and were more satisfied with the process when Dexmedetomidine was used in awake intubation instead of Remifentanyl; generalizability may be limited because subjects were presurgical patients intubated in the operating room. The dose used in this study was 1.5 mcg/kg IV over 10 mins followed by an infusion of 0.7 mcg/kg/hr. In our centre, Dexmedetomidine is on formulary in the ICU only, and not in the ED. In a informal poll of UBC residents and staff, we found that 12 of 14 had either never used Dexmedetomidine or were not comfortable using it, suggesting that more experience with the medication will be necessary before widespread ED implementation. We would recommend Dexmedetomidine as part of your awake intubation kit if available in your ED. We are working toward this in our centre.
c. Haldoperidol (Sedative, Anti-Psychotic)
Haloperidol is the preferred agent in delirium related to critical care because of its rapid onset, minimal sedative effects, anti-emetic properties, and relatively benign hemodynamic profile [8]. Adverse effects include extrapyramidal effects and QTc prolongation. Dose ranges vary from 2.5-5 mg IV and 5-10 mg IM [8,9]. We recommend Haloperidol as an option in combative or agitated patients who require awake intubation. Remember, the goal is to have a cooperative patient, not a deeply sedated patient. Less is more in this case and we recommend the intravenous route for ease of titration.
d. Benzodiazepines (Sedative, Anxiolytic)
There is not much direct evidence for benzodiazepines in awake intubation,. Nevertheless, several sources name midazoloam as a useful adjunct, providing anxiolysis and sedation, with doses ranging from 0.5-4 mg IV [2,3]. Judicious use to avoid respiratory depression and oversedation is prudent.
e. Ketamine (Sedative, Analgesic)
There is ongoing debate regarding the use of ketamine in awake intubation Nevertheless, it remains an excellent agent for anxiolysis and analgesia, and preserves respiratory drive and blood pressure. Patient cooperation is needed to perform an awake intubation and too much ketamine will result in dissociation. Two FOAMed articles on awake intubation [2,3] suggest sub-dissociative doses, such as 20 mg IV q2min to effect or 20 mg IV followed by 10 mg IV q1min titrated to effect. Sub-dissociative dosing also reflects local practice patterns in our area; in our poll, 10 of 13 residents and staff selected standard sub-dissociative dosing for awake intubation. Keep in mind that ketamine We recommend starting low and going slow so that your intubation remains “awake.”
f. Fentanyl (Analgesic, Sedative)
Fentanyl came up in our conversation with local experts as a potentially useful agent. It provides mild sedation and analgesia, and suppresses the cough reflex. A 2008 article in the Journal of Perioperative Medicine [12] outlined an approach to awake intubation with fibre optic laryngoscopy. In the article, the authors recommend a Fentanyl dose of 25 mcg IV in increments to a maximum of 1-1.5 mcg/kg.
g. Ondansetron (Anti-Emetic)
Scott Weingart [3] advocates for Ondansetron 4 mg IV to blunt the gag reflex and prevent vomiting, reducing the risk of aspiration.
Tools and medications for topicalization for an Awake Intubation Kit
a. Lidocaine cream
A small amount of 4% lidocaine cream can be placed on the patient’s tongue until it melts. Then the patient should gargle for 1-2 minutes. This should be repeated 3 times to adequately anesthetize the base of the tongue and the tonsillar pillars.
b. Lidocaine jelly
This can be painted onto the base of the patient’s tongue using a tongue depressor.
c. Viscous lidocaine
Useful for gargling as described above.
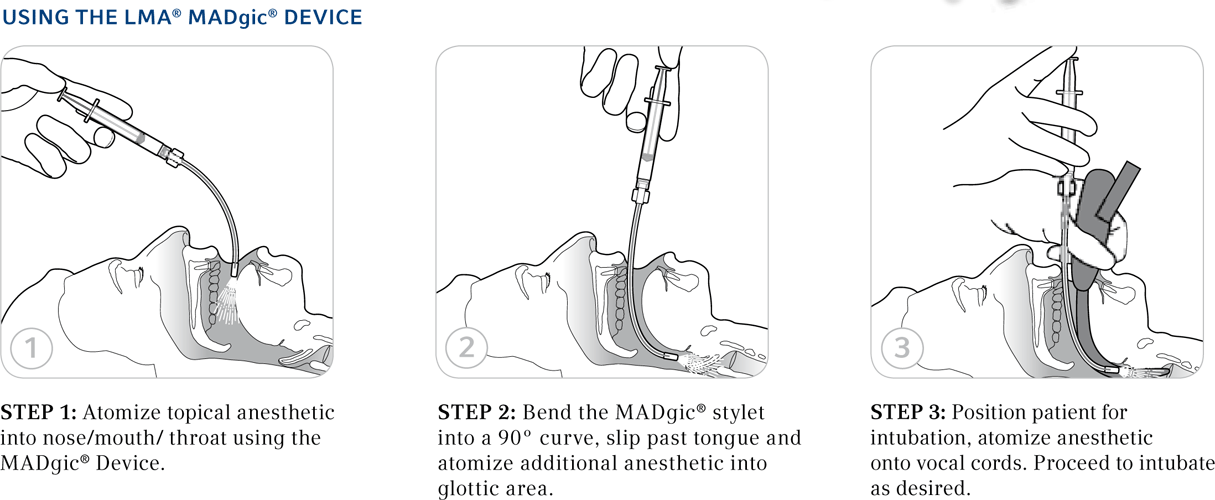
d. Atomization device
There are several. In our shop we have the MADgic device. The cost is approximately $7 US each [13]. The advantage to this device is that you can use a 5 mL syringe and the regular 2% lidocaine that comes in plastic ampules stocked in most shops. Another option suggested by George Kovacs from AIME Airway [4] is the EZ Atomizer. Both of these devices allow precise control of the directionality of the anesthetic spray, which avoids inadvertent over-administration of the drug to the highly absorbent trachea.
e. Lidocaine ampules for nebulization (preservative free)
At Kelowna General, we have 2% lidocaine for this purpose. We do not currently have 4%, although several sources cite 4% as the preferred agent [2,3].
f. Pledgets soaked in viscous lidocaine
These can be placed on the tonsillar pillars and base of the tongue for several minutes to achieve topicalization of these regions. Remember to keep the strings hanging out the mouth to prevent aspiration.
3. Equipment for laryngoscopy and intubation of the trachea for an Awake Intubation Kit
In Kelowna, the CMAC is the agent of choice, but we also have access to fibre optic scopes and a Glidescope. Below is a list of equipment that can be included in your awake intubation kit if they are available at your centre:
a. Direct “line of sight” devices:
• DL (or video laryngoscope with standard MAC format)
b. “See around the corner” devices
- Glidescope or another hyperangulated video laryngoscopy
- Potentially offers the benefit of less manipulation of the oropharynx or hypopharynx in order to achieve an adequate view
- Requires the use of a bougie to help control endotracheal tube delivery
c. Fiber Optic Scope
- Requires additional skill set for operation can provide excellent visualization for endotracheal tube delivery
d. Bougie
- Allows you to place a guide over which to intubate the trachea in situations where using the endotracheal tube alone proves difficult
Other important considerations for an Awake Intubation Kit
1. Lidocaine toxicity
There is a paucity of literature describing maximum doses of topical lidocaine for the pharynx and larynx. Expert consensus is that the maximum is 8 mg/kg [14]. The following factors should be considered when topicalizing an airway with lidocaine [15]:
- The presence of a deep neck infection that causes hyperemia and edema may enhance transmucosal absorption of topical lidocaine.
- Conditions such as hypercarbia, dysphagia, and hepatic disease are known to lower the serum lidocaine concentration threshold for toxic neurologic effects.
The trachea has high lidocaine absorption capabilities so use caution [1]. Here are some strategies we recommend to reduce the risk of lidocaine toxicity:
- Calculate the toxic dose of lidocaine in mL prior to starting the procedure.
- Pay attention if your patient starts complaining of peri-oral numbness or tinnitus during lidocaine administration [15].
- Beware of the potential for increased absorption in the setting of hyperemia and edema, as well as conditions that may lower the serum lidocaine concentration required for toxic effects.
- Spray only 2-3 mL of lidocaine when topicalizing the vocal cords and trachea to minimize tracheal absorption.
- Have suction available at the bedside so that you can immediately suction excess from the oropharyns after a patient has gargled lidocaine.
2. Nasotracheal intubation
In the anesthesia literature, there is discussion of nasotracheal intubation using a fiber optic scope [12]. We will not review nasotracheal awake intubation in this article, beyond mentioning it as a potential adjunct.
3. Laryngeal nerve block
Another adjunct to the awake intubation sequence is the use of local nerve blocks such as the recurrent laryngeal nerve block. The reason we are not including tools for this in our kit is two-fold. First, all you need is a needle, syringe, and local anesthetic; all of which may be found in any trauma/resuscitation bay. Second, depending on where you work this may be beyond your scope of practice.
Conclusion
Episode 3 of our series will highlight our completed kit once we achieve administrative approval and sort out the logistics of who will stock the kit and where it will be stored. We will also put together a short video highlighting our approach to awake intubation where we will put our kit to the test. Stay tuned!
In the mean time, we would love to hear your input. Please comment below if you have any thoughts or contributions. Questions to consider include:
- What dose of Ketamine should we be aiming for in awake intubation? Subdissociative or dissociative?
- If we use dissociative doses is it still a truly awake intubation?
- How did you go about getting Dexmedetomidine stocked in your ED?
- Are you and the rest of your ED group comfortable using Dexmedetomidine?
References:
- Hu, R., Liu, J., & Jiang, H. (2013). Dexmedetomidine versus remifentanil sedation during awake fiberoptic nasotracheal intubation: A double-blinded randomized controlled trial. Journal of Anesthesia, 27(2), 211-217.
- Strayer, R. (2013). Awake Intubation: A Very Brief Guide. Retrieved March 10, 2015, from http://emupdates.com/2013/07/07/awake-intubation-a-very-brief-guide/
- Weingart, S. (2010). Podcast 18 – The Infamous Awake Intubation Video. Retrieved March 10, 2015, from http://emcrit.org/misc/awake-intub-video/
- Weingart, S. (2015). Podcast 142 – Airway Things I Learned from George Kovacs at the NYC Airway Course. Retrieved March 16, 2015 from http://emcrit.org/podcasts/airway-kovacs/
- Photo retrieved March 16, 2015 from https://www.flickr.com/photos/demonbaby/3721262528/
- Toronto General Hospital Department of Anesthesia. Perioperative Interactive Education: Awake Bronchoscopic Intubation. Retrieved March 10, 2015 from http://pie.med.utoronto.ca/BI/BI_content/BI_module4.html#decision2
- Dexmedetomidine: A Clinical Review. Retrieved March 16, 2015 from http://hartleymedical.com/blog/dexmedetomidine-a-clinical-review/
- Wang, E., Mabasa, V., Loh, G., & Ensom, M. (2012). Haloperidol Dosing Strategies in the Treatment of Delirium in the Critically-Ill. Neurocritical Care, 16(1), 170-183.
- Retrieved March 10, 2015 from http://www.stars.ca/mcgs/3_1_Analgesia_Sedation.htm
- Photo retrieved March 16, 2015 from http://sheilawilson.hubpages.com/hub/What-is-Haldol
- Photo retrieved March 16, 2015 from http://pedemmorsels.com/delayed-sequence-intubation/ketamine/
- Peiris, K., & Frerk, C. (2008). Awake Intubation. Journal of Perioperative Practice, 18(3), 96-104.
- Photo retrieved March 10, 2015 from http://www.naloxone-hydrochloride.com/madgic-laryngo-tracheal-mucosal-atomization-device-25-box.html
- Hagberg, CA. The Difficult Airway: A Practical Guide. Oxford: Oxford University Press.
- Giordano, D., Panini, A., Pernice, C., Raso, M., & Barbieri, V. (2014). Neurologic toxicity of lidocaine during awake intubation in a patient with tongue base abscess. Case report. American Journal of Otolaryngology, 35(1), 62-65.

![Figure 1: The oropharynx post-glycopyrrolate; dry like the New Mexico desert [1].](http://canadiem.org/wp-content/uploads/2015/07/1-300x200.png)
![Figure 2: Dexmedetomidine [7].](http://canadiem.org/wp-content/uploads/2015/07/2.png)
![Figure 3: IM Haldol [3].](http://canadiem.org/wp-content/uploads/2015/07/3.png)
![Figure 4: “Special Ketamine” [2].](http://canadiem.org/wp-content/uploads/2015/07/4-300x206.png)


![Figure 7: How to use the MADgic Mucosal Atomization Device [5].](http://canadiem.org/wp-content/uploads/2015/07/7-300x123.png)

![Figure 9: Pledgets for use in topicalizing the tonsillar pillars and the base of the tongue [4].](http://canadiem.org/wp-content/uploads/2015/07/9-300x200.png)
![Figure 10: Fiber optic scope [11].](http://canadiem.org/wp-content/uploads/2015/07/10-300x206.png)