This month we launch the first post in a new series entitled “Boring Questions”. This column will focus on reviewing key literature around common questions that might be asked during a shift. – Teresa Chan (Managing Editor)
Clinical Scenario:
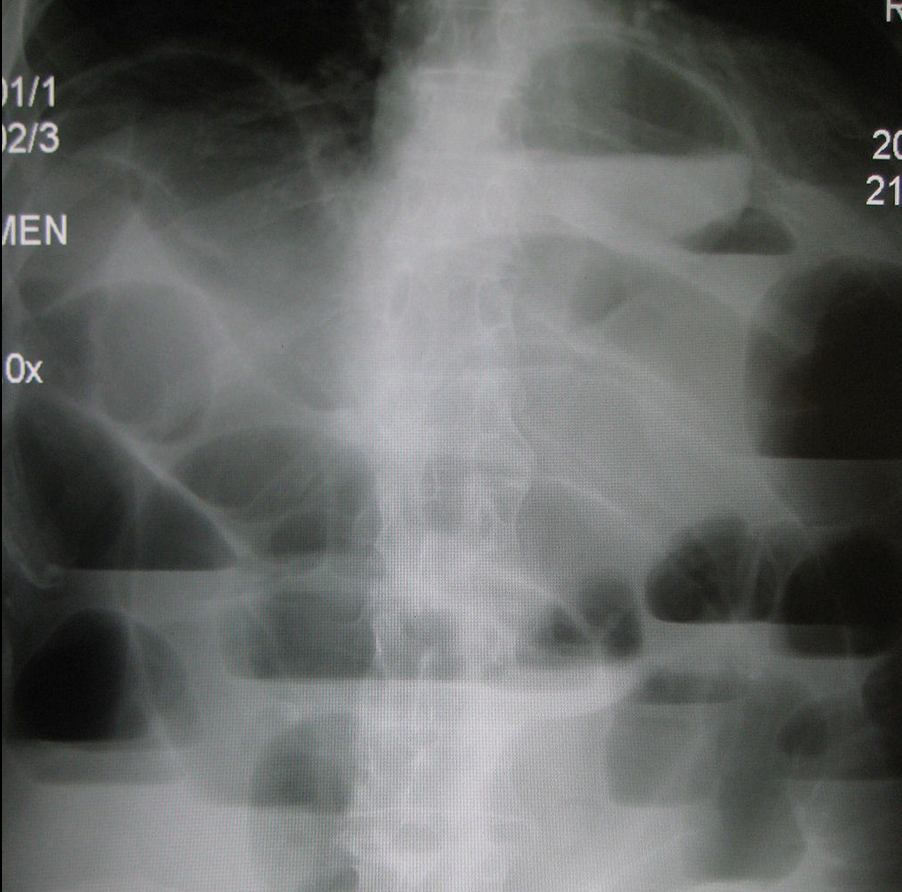
A 60-year-old female presented to the emergency department with a 24 hour history of lower abdominal pain. The pain had increased in intensity over the past day and was 7/10 on presentation. She has been nauseated for the past 12 hours with no episodes of emesis. She was not sure when her last bowel movement was and she also described feeling bloated. Her only previous surgery was an appendectomy (1980). She had no urinary complaints and had not been sexually active in the past year. She denied eating any food out of the ordinary for her.
On physical examination her vitals were:
Temp: 37.5, HR: of 80, RR: 16, BP: 132/82, O2: 98% on room air.
She was moving in bed with the seeming discomfort. Her abdomen appeared distended with no surgical scars. She did not have any rebound tenderness or guarding to palpation. She was in mild discomfort with pain to palpation of both the left and right lower quadrant. Her digital rectal examination did not reveal any occult blood per rectum (usefulness of this test to be reviewed at a later date).
The Boring Question:
How useful are bowel sounds for a patient with abdominal pain and potential small bowel obstruction?
Background:
Auscultation of the abdomen to evaluate motility and mechanical properties of the bowels is a well-established part of the physical examination but its clinical value has been understudied (1). Historically it has been taught that decreased bowel sounds may suggest ileus, mesenteric infarct or narcotic use while hyperactive bowel sounds, might suggest small bowel obstruction (SBO) (2).
Search Strategy:
Using PubMed, two separate searches were performed. These were:
- ‘Bowel Auscultation’ AND ‘Abdominal Pain’
- ‘Bowel Sounds’ AND ‘Abdominal Pain’.
The resulting abstracts were screened with relevant articles reviewed. In addition to the literature, the textbooks ‘Tintinalli’s Emergency Medicine’ and ‘Evidence-Based Physical Diagnosis’ were also reviewed.
The Evidence:
- Evidence-Based Physical Examination reviews data that suggests that 40% of SBO patients have hyperactive bowel sounds, while 25% have diminished/absent bowel sounds (4). From this, the author surmises that 35% of patients with SBO have normal bowel sounds which gives a -LR of SBO of 0.4. This is a moderate likelihood ratio that could be helpful as a diagnostic test but the author also admits that determining whether bowel sounds are hyperactive, normal or hypoactive is not objective and there are many associated variables including quadrants, time since last meal, normal bowel function etc.
- A more recent investigation by Felder et al. in 2014 prospectively recorded bowel sounds from patients with normal gastrointestinal motility and small bowel obstruction, diagnosed by CT scan and confirmed in the operating room (1). The positive predictive value for auscultation in normal versus cases of small bowel obstruction was found to be 23% (CT diagnosed) and 28% (OR diagnosed) (1).
- Similarly, a study by Bohner et al. in Germany assessed 1254 patients (3). This study found that increased bowel sounds had a sensitivity of 39.6% and specificity of 88.6% (+LR 3.5) for the detection of bowel obstruction. (3). But the same group of patients, decreased bowel sounds also had a positive predictive value was 11.2% (3). It is important to note issues with this investigation which include a broad age group from 9 to 97 years with no demographic analysis (3).
Bottom Line:
There is little literature on this physical exam technique the available evidence suggests that bowel sounds are not an objective or reliable method to assess patients for small bowel obstruction.
References
1. Felder S, Margel D, Murrell Z, Fleshner P. (2014) Usefulness of Bowel Sound Auscultation: A Prospective Evaluation. Journal of Surgical Education In Press . Link
2. Tintinalli’s Emergency Medicine-A Comprehensive Study Guide (2011). New York. McGraw Hill Companies Inc. Link
3. Lamont C. (2011). Towards evidence based emergency medicine: best BETs from the Manchester Royal Infirmary. BET 4. How useful are bowel sounds. Emerg Med J. 28 (4): 336. Link
4. McGee S. (2007). Auscultation of the Abdomen. In Evidence-Based Physical Diagnosis (588-593). Philadelphia: Saunders Elsevier. Link
Reviewed by Eve Purdy (Student Editor), and Teresa Chan MD FRCPC (Managing Editor)