Overview
The following are three key steps that you can take to start “thinking like an emergency physician”. Unlike other clinical services, the emergency department is often quite chaotic and requires a different mindset for organization of time and workflow. Check out this video made by the McMaster University Demystifying Medicine program alumni.
Step 1: Stable vs. Unstable
Look at your patient. The emergency medicine mindset is that you should be addressing your patient’s emergent needs (e.g. ABCs), using their vital signs (HR, RR, O2 sat, BP, and point-of-care glucose) to guide your thinking. It is imperative to consider who is sick and requiring immediate attention, and who is well enough to wait. The determination of stable versus unstable is of the utmost importance.
Step 2: Commit to your Disposition
It is worth conceptualizing the ED as a corridor rather than a ward. New patients are always coming in so the ones under your care have to be diagnosed, managed, and dispositioned so as to create room for more.
Decide early in the encounter if the patients are likely going home, staying or shall be decided upon after investigations and/or consults.
One way to think about this is to sort the patients into 3 groups – Red (Critically ill), Yellow (Needs testing and perhaps admission), and Green (Needs some investigations to rule out and minor treatments). Thinking about your red-green-yellow decisions will help you think ahead.
Step 3: The Two-Step Differential Diagnosis Process
In emergency medicine, we always have to bear in mind the worst differential diagnoses (WORST CASE DDx) when we walk in the room. Until proven otherwise, all of our chest pain patients have aortic dissection, coronary artery disease, pulmonary embolism, and a pneumothorax. Although this is a bizarre way to think, it increases your sensitivity for bad things if you go in thinking about how you have to rule these out with your history and physical exam. We like to rule out the top-most deadly causes at first and work our way down to the common and likely, with highlights to red flags and documenting these on the chart.
Once you’ve spoken to your patient and examined them as best you can, REFINE your initial worst-case DDx to improved differential diagnoses of those conditions are still on your list – the bespoke DDx.
Within this bespoke list, consider creating a prioritization system. Some like to sort and prioritize the DDx by three levels: Critical, Emergent, and Common.
Step 4: Managing Multiplicity
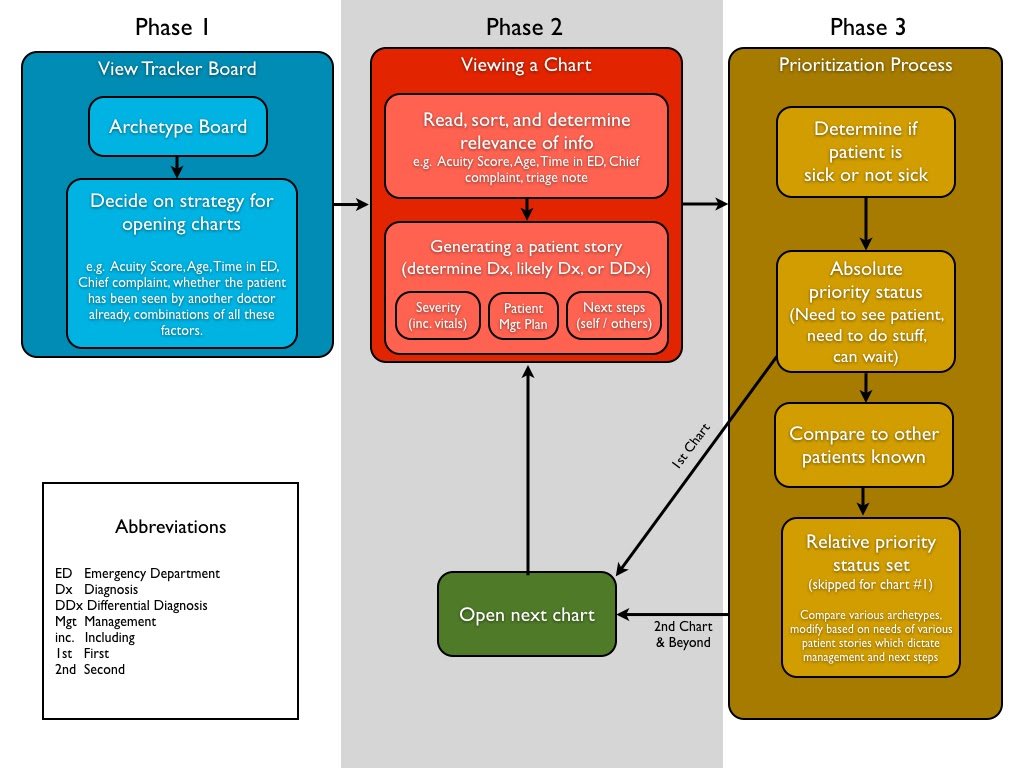
Recent literature has found that emergency physicians manage multiple patients at once by quickly assessing and labelling each patient with temporary labels that encapsulate their story and ED trajectory.1 The figure below highlights this process.
Once you have a sense of what each patient is requiring (e.g. bloodwork, CT, admission) you get a feel for the ebb and flow of the department. You will start to develop an internal sense of how long labs will take, or whether or not you’ll have a big queue for ultrasounds. This anticipatory ability will allow you to better bounce between patients. Like a master chef or an experienced barista, you’ll start to be able to anticipate your workflow needs.
Until you do, here are some simple procedures you can adopt to help optimize your workflows while you’re guest-starring in the ED:
- “Round” upon (i.e. reassess) your current patients every hour or so. Review all their labs/tests, see what’s back. Once the labs are back, see how they are doing clinically, and make sure you DOCUMENT that you did so.
- Run the board with your team – with the doc in charge or the charge nurse, go through the whole list of patients on the go, and see if there are themes that arise. If everyone is having trouble getting CT results back, someone probably needs to reach out to the radiology team to see what’s going on. It may be that work from the other part of the hospital is affecting some of your needs (e.g. the troponin machine is down).
- After each resuscitation, make sure to sit down and reassess your patients. Some resuscitations (especially ones related to COVID-19) may require you to be sequestered in full PPE for a good chunk of time (e.g. 45 minutes to an hour). Upon completing that case, make sure to return your tracker board to figure out what the situation in the department is like. Things may have drastically changed since you looked at it last!
Step 5: Playing “Tetris” with Time
Efficiency will come after you’ve gotten a sense of timing. Within increased anticipatory ability, you will slowly become able to predict which patients require a full work-up and which ones don’t. You’ll also most likely get more accustomed to the way that our triage nurses communicate via their initial assessment notes.
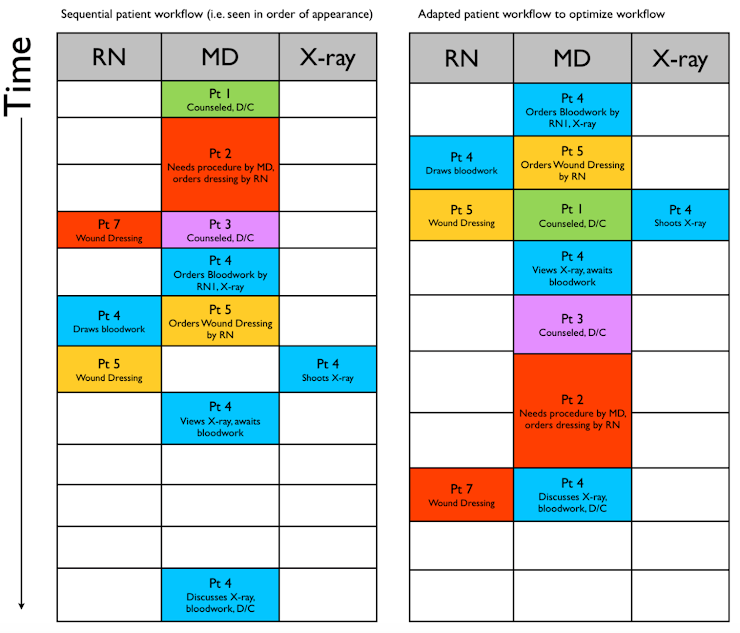
Once you get in the swing of things, you’ll start spotting patterns and find ways to be more efficient. The diagram below highlights the importance of optimizing your own personal workflow.
One other pro-tip – chart as you go! If you chart on paper, you won’t be able to take your charts home to finish (due to COVID-19 considerations), so don’t spend many extra hours in the ED writing notes – integrate note writing into your workflow. Similarly, for those charting electronically, it is a huge bummer to have to spend time at home charting when you can be recovering and resting between shifts.
Most Importantly…
And most importantly, stay aware and safe. Take care of your physical and emotional needs especially during this crunch time- you are precious!
Recommended reading, videos and podcasts
- Closler blog: The Balancing Act: Learning to Thrive in Multipatient Environments (Canadian Content on American Blog)
- Reuben Strayer at Western University’s EM Rounds – Emergency Thinking (Canadian-Trained American)
- REBEL EM: The EM Mindset (CAUTION: American resource)
The following is part of the CanadiEM Frontline Primer. An introduction to the primer can be found here. To return to the Primer content overview click here.
This post was edited by Dr. Brent Thoma MD FRCPC. This post was copyedited and uploaded by Evan Formosa.
References
- 1.Chan TM, Mercuri M, Van Dewark K, et al. Managing Multiplicity. Academic Medicine. May 2018:786-793. doi:10.1097/acm.0000000000002081
- 2.Chan T. What’s next? COgnitive Task Analysis of Emergency Physicians’ Experience in Multi-Patient Environments. October 2016. https://indigo.uic.edu/articles/What_s_Next_Cognitive_Task_Analysis_of_Emergency_Physicians_Experience_in_Multi-Patient_Environments/10915484/1.



