Emergency Medical Services receives a 9-1-1 call for a 52-year-old female suffering with chest pain. As Paramedics rush to the scene, they discuss the physiology of Acute Coronary Syndromes…
[bg_faq_start]About Sirens to Scrubs
Sirens to Scrubs was created with the goal of helping to bridge the disconnect between pre-hospital and in-hospital care of emergency patients. The series offers in-hospital providers a glimpse into the challenges and scope of practice of out-of-hospital care while providing pre-hospital providers with an opportunity to learn about the diagnostic pathways and ED management of common (or not-so-common) clinical presentations. By opening this dialogue, we hope that these new perspectives will be translated into practice to create a smoother, more efficient, and overall positive transition for patients as they pass through the ED doors.
[bg_faq_end]Objectives
- Review the pathophysiology of stable angina and ACS
- Review the clinical exam findings associated with ACS
A Brief Review of Physiology
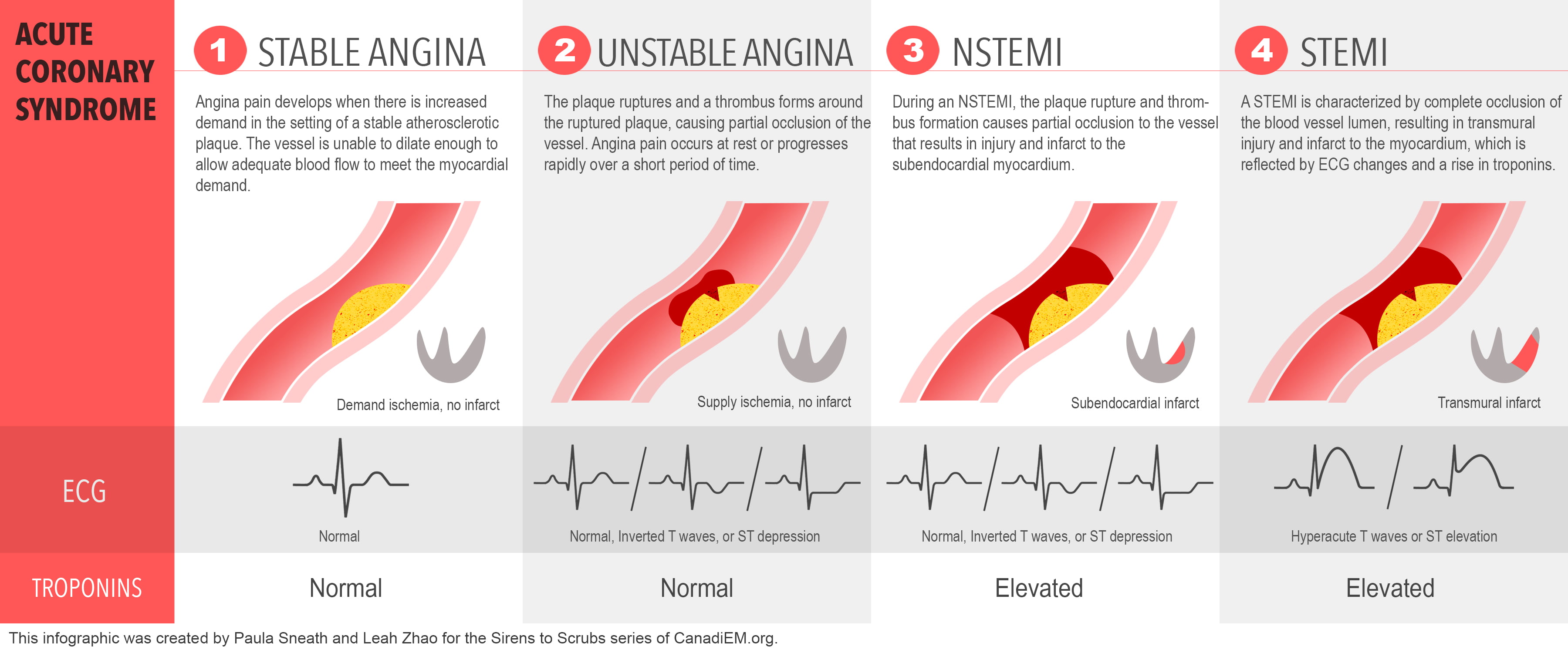
Behind the curtain of an Acute Coronary Syndrome (ACS) primarily lies the evil wizard, coronary atherosclerosis. Risk factors such as dyslipidemia, diabetes, hypertension, obesity, and smoking result in damage to the endothelium (the inner lining) of coronary arteries, resulting in physiological derangements causing increased clotting and impaired vasodilation. With the damage to the endothelium, inflammatory cells, including macrophages, are able to migrate into the artery wall in the area just below the endothelium called the subendothelium. Amongst other mechanisms beyond the scope of a short review, these macrophages consume and digest low-density lipoproteins (LDL), transforming into foam cells and contributing to the formation of coronary plaque.1–9 The pain experienced by patients suffering from stable angina is a direct result of the continued growth of this coronary plaque, without rupture or erosion. Angina pain develops when the body requires more oxygen (i.e. exertion or stress), causing the heart to work harder, but the now partially occluded coronary arteries are unable to vasodilate themselves to increase their own oxygen delivery.
If this plaque is eroded or disrupted, the subendothelial layer, with the sticky foam (and other) cells, is exposed to the circulating blood. Platelets (which are always flowing through the bloodstream) recognize this as an injury, so they do their job to plug the hole by grabbing on and creating a clot. The bound platelets are then triggered to express GP IIb-IIIa receptors (believe me, I avoid medical jargon when I can, but the importance of this particular term will become clear later). The GP IIb-IIIa receptors reach out into the circulating bloodstream to grab more platelets, as well as free-flowing fibrinogen, which all stick together to form the dreaded coronary thrombus. As the thrombus develops, a fibrin mesh is constructed which ensnares red blood cells, macrophages, and other plasma contents as it continues to grow.1,3,6–9
We’ve already discussed the story of stable angina, and now with this extra bit of pathophysiology, we can review the Acute Coronary Syndromes (unstable angina, non-ST-elevation myocardial infarction, and ST-elevation myocardial infarction):
- If the affected coronary artery is occluded, but the tissue beyond the occlusion is ischemic but uninjured, this is called unstable angina (UA). Several factors can protect the cardiac tissue from injury, such as collateral circulation (the development of extra arteries around an area of chronic narrowing), the body’s own anti-coagulation system which continuously fights to break down the clot, or the size of the occlusion. In this condition, there may be ischemic ECG changes, but there will not be ST-segment elevation (indicative of injury) or evidence of myocardial cell death on bloodwork (which is assessed by the amount of troponin, a biomarker that will be discussed later in this mini-series).
- In the next syndrome, non-ST-segment elevation myocardial infarction (nSTEMI), the coronary artery is again partially occluded, but in this case, the cardiac tissue beyond the occlusion IS injured. This may be because of inadequate collateral circulation (potentially because there has been less of a chronic process of narrowing before this event), inadequate thrombus breakdown by the body, or more severe occlusion. In this syndrome, there may or may not be ischemic ECG changes, but there WILL be evidence of myocardial cell death on bloodwork.
- Finally, when the thrombus results in a total occlusion of a coronary artery with the ECG demonstrates cardiac injury through localized ST-segment elevation on the ECG (hence the name ST-elevation myocardial infarction). Of course, there will also be evidence of myocardial cell death on the bloodwork in this syndrome as well.3,10
On arrival at the scene, Paramedics find the patient clutching her chest, pale, diaphoretic and in obvious discomfort. The patient reports a four-day history of exertional chest pains, which she has never experienced before. Whilst traveling to see her General Physician today, she experienced a sudden onset of central chest pain with radiation into her shoulders bilaterally. The pain is described as ‘crushing’, rated as a 10/10 and is neither positional nor reproducible on palpation. As her partner acquires a 12-lead ECG, the attending paramedic considers which risk factors and historical findings may indicate an acute coronary syndrome…
Incident History & Risk Stratification
It is worth prefacing this section by reiterating the need to maintain a high index of suspicion for ACS in women, the elderly, diabetic patients, and patients with a number of significant co-morbidities.4,5,11 In these patient groups, atypical is typical. It is also worth noting that no historical or physical exam finding can entirely exclude an ACS (yes, even reproducible chest pain can be ACS!), although a number of features assist in increasing the likelihood that the patient is suffering from an ACS. From a prehospital perspective, if you are unsure of your diagnosis and 12-lead ECG acquisition is available, it is a fast and inexpensive test which may literally save your patient’s life. If you are on the fence, get one.
Patients suffering from an ACS will often describe an onset of chest pain with radiation into the left, right or both shoulders (pinpoint pain decreases the likelihood of ACS). Symptoms which increase the likelihood of ACS in conjunction with chest pain include observed diaphoresis, vomiting, and pain with either began with or is worsened by exertion.4,5,11 Although positional and reproducible pain decreases the likelihood of ACS, they do not exclude it! Likewise, nitroglycerin (or glyceryl trinitrate, depending on where you read this from) is not a diagnostic tool so do not use it as such. Pain caused by ACS may be refractory to nitroglycerin therapy, whilst the pain caused by oesophageal spasm (for example), can be relieved with nitrates.1213
For a good review of the positive and negative predictive values of clinical exam findings for myocardial infarction, see the JAMA Rational Clinical Examination series, “Is This Patient Having a Myocardial Infarction?”
What if the ECG is Normal!?
Time for risk stratification! Scores such as the HEART Score and Vancouver Chest Pain Rule have been developed and validated to assist in risk-stratifying patients with chest pain who may be eligible for early discharge from the emergency room (after a single troponin measurement, for example). Although not yet validated for use in the prehospital setting, an early prospective study suggests there may be a role for modified versions of these scores in the future.14 This is of particular importance in tiered systems of Emergency Medical Service (EMS) delivery, where Advanced Care Paramedics (ACPs) may be required to decide whether to hand over clinical care to Primary Care Paramedics (PCPs) whose scope may not include cardiac monitoring, ECG interpretation, IV initiation, or administration of various medications.
Until further validation of these scores takes place in the prehospital setting they can’t be recommended for decision guidance. However, it is worth noting the scores themselves and the associated guidance provide a useful structure for history taking and clinical evaluation in patients suspected of ACS as only one component in each score is associated with biomarkers. Both scores are available on MDCalc and come with detailed instructions for use.
The Paramedics review the 12-Lead ECG which confirms a massive STEMI. With the old adage ‘Time is Myocardium’ ringing in her ears, they begin to plan their course of treatment and conveyance to the appropriate destination hospital….
Stay tuned for the next segment of “Sirens to Scrubs: Acute Coronary Syndromes” – in the meantime, find more Sirens to Scrubs articles here!
A special thanks to @LeahZhao for her artistic contributions!
As always, if you have any questions, thoughts, alternative perspectives, or requests for future topics, feel free to comments below or send me an email at [email protected]. Please keep in mind that, although I will do my best to publish information that is accurate across Canada, there will inevitably be some regional differences in both pre-hospital and in-hospital management of emergency patients. As a paramedic and Emergency Medicine resident in Ontario, some posts may wind-up being somewhat Ontario-centric, hence, I encourage anyone whose experiences differ from mine to contribute to the conversation by commenting below.


