Intubation in children is an uncommon but high-risk procedure in the emergency department.1 The incidence of adverse events during intubation is high, particularly desaturation and hypotension.1 Thus, pediatric airway management is an important and lifesaving skill. The pediatric airway has significant anatomical differences from an adult. To remember these variations, consider the mnemonic “CHILD”.
| How is it different? | How do we change management? | |
| Cricoid2 | Narrowest portion of airway. Risk of subglottic stenosis. | Keep cuff pressure <20cm H2O. |
| Head2 | Prominent occiput. Head naturally flexed. | Add shoulder roll to align oral, laryngeal and tracheal axes. <6 months: towel under shoulder 6 months – 5 years: no towel >5 years old: towel under head. |
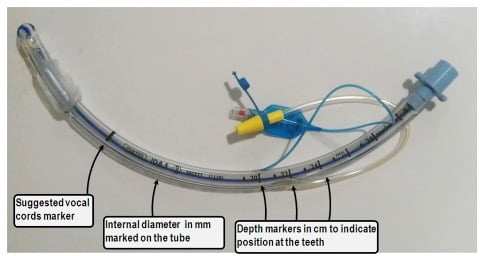
| Intubated mainstem3 | Short, funnel-shaped trachea. Risk of endobronchial intubation or accidental extubation. | Ensure that the black ETT marker lies just past the vocal cords (see Appendix 1). Alternatively, depth can be estimated by correct cuff size multiplied by 3 (see Appendix 2 for appropriate cuff size). |
| Larynx2 | Located more anterior and superior (C4-5) than in adults (C5-6). | May need to use External Laryngeal Manipulation (ELM) to improve laryngoscopic view (see Appendix 3). |
| Droopy tongue and epiglottis2 | Large tongues – prone to upper airway obstruction. Floppy epiglottis – can lead to a more challenging view. | Use airway maneuvers and oropharyngeal airway. Consider choice of straight blade to lift the epiglottis. However, providers should use the blade that they are most comfortable with and in which they have highest first pass success. |
Because symptomatic infection of Covid-19 can be common in children it is important to remember to wear all safety PPE for aerosolized procedures such as intubation.
This post was reviewed by Daniel Ting and copyedited by Samara Adler
- 1.Long E, Sabato S, Babl F. Endotracheal intubation in the pediatric emergency department. Paediatr Anaesth. 2014;24(12):1204-1211. doi:10.1111/pan.12490
- 2.Harless J, Ramaiah R, Bhananker S. Pediatric airway management. Int J Crit Illn Inj Sci. 2014;4(1):65-70. doi:10.4103/2229-5151.128015
- 3.Miller K, Kimia A, Monuteaux M, Nagler J. Factors Associated with Misplaced Endotracheal Tubes During Intubation in Pediatric Patients. J Emerg Med. 2016;51(1):9-18. doi:10.1016/j.jemermed.2016.04.007
Appendix 1
Appendix 2
| Uncuffed tube | Cuffed tube* |
| 4 + (age in years/4) | 3.5 + (age in years/4) |
Additional tubes one size larger and one size smaller than calculated should also be available
*Use formular for children 2 years of age and older. Use 3.5 mm internal diameter cuffed endotracheal tube for children 1 to <2 years of age and a 3.0 mm internal diameter cuffed for children < 1 year of age
Appendix 3
Video displaying the difference between ELM and cricoid pressure
Reviewing with the Staff
The pediatric airway can be quite challenging if unprepared and in an emergent setting. In addition to the tips above, here are some other factors to keep in mind:
- Always choose age-appropriate equipment for children and have multiple sizes available. If you can’t remember all the different formulae, use memory aids like Broselow tape or one of the medical app calculators.
- Gastric insufflation from mask ventilation can significantly compromise the ability to ventilate. Consider inserting a gastric tube early to decompress the stomach.
- Children have higher oxygen consumption and can sometimes be difficult to pre-oxygenate and are therefore prone to rapid desaturation.(2) It is important to plan well for an optimal first attempt at intubation and be prepared to oxygenate with mask ventilation or LMA if the child starts to desaturate.



