A 30-year-old male presents to the ER with right forearm redness, swelling and pain. On exam, you are unsure whether this infection represents cellulitis or abscess. You wonder if point-of-care ultrasound (POCUS) can be helpful.
Superficial soft tissue infections are a common ED presentation. Cellulitis appears as an area of erythema, edema and tenderness. An abscess is suspected when a discrete fluctuant mass is palpated within the infected tissue. However, relying on these features can be problematic as there is often overlap. Accurately determining the presence or absence of an associated abscess has significant treatment implications. Cellulitis can be medically managed with antibiotics while an abscess generally requires an incision and drainage (I&D). Misdiagnosing one as the other can lead to delay of the appropriate care and worsen the infection. Unfortunately, the physical exam alone, is inadequate to differentiate between the two diagnoses.1 Berger et al. in 2012 found that clinical exam was only 76% sensitive and 83% specific in detecting an abscess. Yikes. Prior observational studies suggest that bedside ultrasound has high diagnostic accuracy in distinguishing between the two presentations and can reduce the risk of treatment failure.2 3
[bg_faq_start]SOFT TISSUE POCUS
Ultrasound is safe, quick and available is most emergency departments. A high frequency linear probe is used. Figure 1, clip 1 and 2 demonstrate the classic POCUS findings of normal tissue, cellulitis and abscess. Once a fluid collection is identified, the size and depth of the abscess can be used to directly guide I&D.
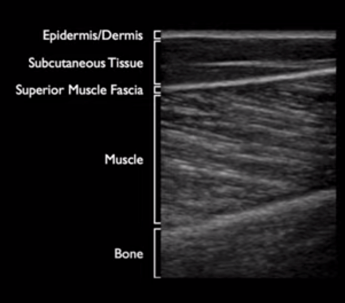
Fig 1. Normal soft tissue: well-organized tissue layers.4
Clip 1. Cellulitis: cobblestoning (hypoechoic fluid separating subcutaneous tissue and fat), loss of fascia planes and hyperemia on color flow doppler.5–7
Clip 2. Abscess: well-circumscribed compressible anechoic lesion (+/-internal echoes of pus/debris) with hyperechoic posterior acoustic enhancement (acoustic energy of the ultrasound beam is minimally reduced when passing through fluid compared to solid tissue). 6,8
There are significant pitfalls with POCUS to consider. False positives include hematoma, vessel, lymph node, pseudoaneurysm or herniated bowel.5 False negatives can occur as some abscesses may be isoechoic or hyperechoic, and therefore more difficult to see.5 When there is ambiguity, color doppler mode on POCUS could be effective in determining between a cyst lymph node or abscess.9 It is important for the user to be familiar with normal and pathologic soft tissue sonoanatomy before integration into practice.
[bg_faq_end][bg_faq_start]THE EVIDENCE
A recent excellent systematic review and meta-analysis from Gottlieb et al. looked at this clinical question. 14 studies with 2656 total patients were identified. POCUS was 94.6% sensitive (89.4-97.4%) and 85.4% specific (78.9-90.2%), with LR + of 6.5 (4.4-9.6) and LR – of 0.06 (0.03-0.13) for diagnosing abscesses.10 Among cases with a high pretest suspicion for abscess or cellulitis, POCUS is 93.5% sensitive and 89.1% specific, whereas among cases that are clinically unclear, POCUS is 91.9% sensitive and 76.9% specific.9 Despite the lower accuracy in diagnostic unclear cases, POCUS clearly outperforms physical examination alone in these scenarios.9 Overall, POCUS led to a correct change in management in 10.3% of cases and led to an incorrect change in management in 0.7% of cases.10
CASE RESOLUTION
You perform a bedside POCUS which showed a superficial 5x5cm anechoic collection with posterior shadowing. You appropriately drain the abscess and prescribe antibiotics for associated cellulitis on discharge.
BOTTOM LINE
The accuracy of POCUS to differentiate between cellulitis and abscess is far superior compared to physical exam alone. So bring out the ultrasound machine for your next patient with soft tissue infection so we can continue to provide better and safer patient care.
[bg_faq_end]This post was copyedited by Jeremi Laski (@JeremiLaski)
- 1.Berger T, Garrido F, Green J, Lema P, Gupta J. Bedside ultrasound performed by novices for the detection of abscess in ED patients with soft tissue infections. Am J Emerg Med. 2012;30(8):1569-1573. doi:10.1016/j.ajem.2011.08.002
- 2.Subramaniam S, Bober J, Chao J, Zehtabchi S. Point-of-care Ultrasound for Diagnosis of Abscess in Skin and Soft Tissue Infections. Acad Emerg Med. 2016;23(11):1298-1306. doi:10.1111/acem.13049
- 3.Barbic D, Chenkin J, Cho D, Jelic T, Scheuermeyer F. In patients presenting to the emergency department with skin and soft tissue infections what is the diagnostic accuracy of point-of-care ultrasonography for the diagnosis of abscess compared to the current standard of care? A systematic review and meta-analysis. BMJ Open. 2017;7(1):e013688. doi:10.1136/bmjopen-2016-013688
- 4.Soft tissue . The Pocus Atlas. Accessed April 21, 2021. https://www.thepocusatlas.com/softtissue-2
- 5.Schick M. Point-of-care Ultrasound for Soft Tissue. Sonostuff. https://sonostuff.com/2016/09/12/pocus-for-soft-tissue-cellulitis-abscess-nec-fasc-foamed-foamus-meded-ultrasound/
- 6.Adhikari S, Blaivas M. Sonography first for subcutaneous abscess and cellulitis evaluation. J Ultrasound Med. 2012;31(10):1509-1512. doi:10.7863/jum.2012.31.10.1509
- 7.Cobblestoning in cellulitis . The Pocus Atlas . Accessed February 2, 2021. https://www.thepocusatlas.com/softtissuemsk/2019/1/26/cobblestoning-in-cellulitis
- 8.Soft Tissue Abscess . The Pocus Atlas. Accessed February 2, 2021. https://www.thepocusatlas.com/softtissuemsk/2019/1/26/soft-tissue-abscess
- 9.Gottlieb M, Sundaram T, Kim D, Olszynski P. Just the facts: point-of-care ultrasound for skin and soft-tissue abscesses. CJEM. Published online April 22, 2021. doi:10.1007/s43678-021-00132-9
- 10.Gottlieb M, Avila J, Chottiner M, Peksa G. Point-of-Care Ultrasonography for the Diagnosis of Skin and Soft Tissue Abscesses: A Systematic Review and Meta-analysis. Ann Emerg Med. 2020;76(1):67-77. doi:10.1016/j.annemergmed.2020.01.004
REVIEWER COMMENTS
Real-time POCUS for soft tissue infections is easy to learn and quick to perform. I have found it particularly helpful in certain situations. A patient may initially appear to have an uncomplicated soft tissue abscess requiring a simple I&D. However, when the probe is placed over the area, the abscess may be significantly larger and deeper than what the external appearance suggests, and the patient would benefit instead from CT evaluation and assessment by surgery for I&D in the OR. Alternatively, the fluid collection may be too small or contain very dense pus, and the most appropriate treatment would be a course of antibiotics and close follow-up without an I&D. Sometimes, the scan may show significant internal loculations within the abscess, which will require special attention during the procedure to ensure they are properly opened up. I also like to repeat the POCUS post-I&D to ensure adequate resolution to minimize treatment failure and return ED visits.


