Upper Respiratory Infection symptoms like cough or sore throat are still some of the top reasons for Canadian emergency department visits, and will likely be even higher in the upcoming months and in Urgent Care Centres.1 The most common organisms responsible for uncomplicated acute pharyngitis are viral agents at 50-80% and Streptococcal agents, specifically Group A Beta-Hemolytic Strep, at 5-36%.2 It is clinically significant to differentiate between these two pathogens as patients with the latter would benefit from antibiotic therapy, and patients with the former should not have antibiotic therapy due to deriving no benefit.
| Modified Centor Score | |
| Symptoms or Signs | Points |
| 1. History of Fever or measured temperature >38oC | +1 |
| 2. Absence of Cough | +1 |
| 3. Tender/Swollen anterior cervical lymphadenopathy | +1 |
| 4. Tonsillar swelling or exudate | +1 |
| Age < 3-14 years* | +1 |
| Age 15 – 44 years | 0 |
| Age ≥ 45 years | -1 |
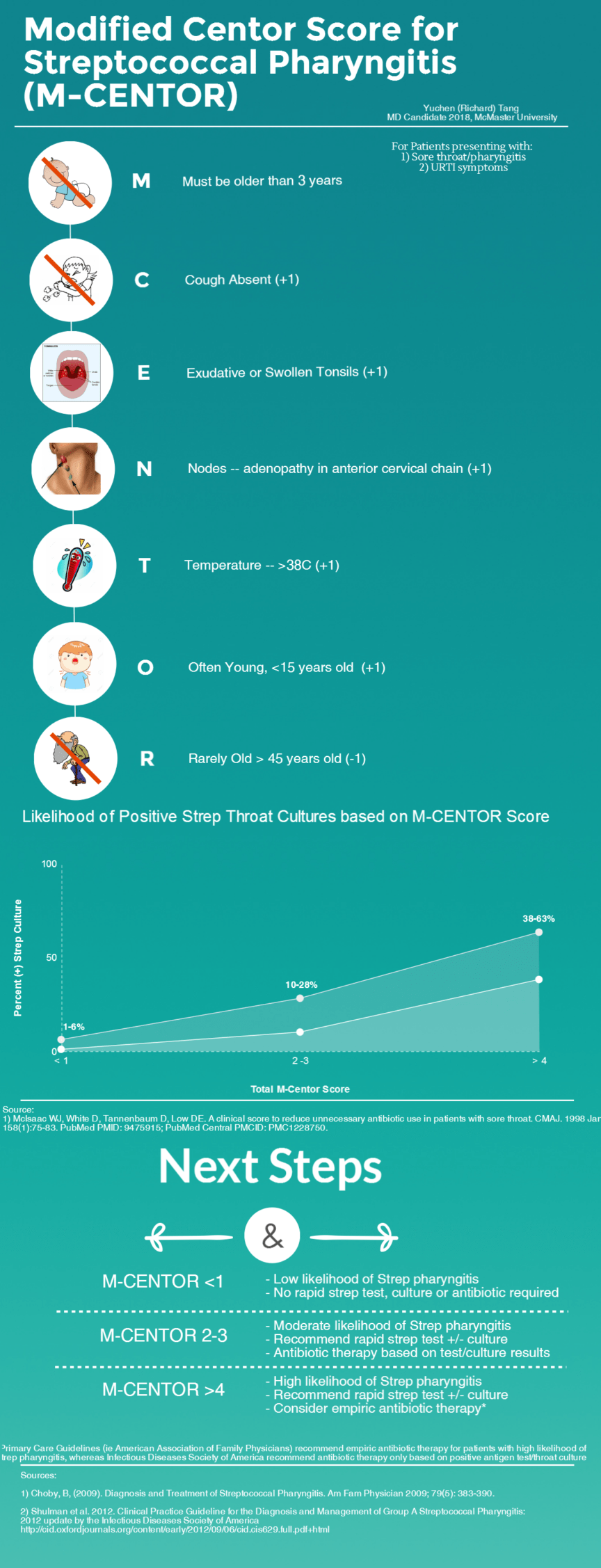
Figure 1: McIssac Modification of the Centor Score. Data from group of 167 children >3 years and 453 adults in university-affiliated family medicine center in Toronto, ON Canada. The study and subsequent score excluded patients under 3 years of age as strep throat is very rare in this population.3
The Modified Centor Score (also known as the McIssac Score or the McIssac Modification of the Centor Score) helps predict the probability of streptococcal pharyngitis by taking into consideration risk factors such as patient’s age, symptoms, and physical exam. This score is easy to use as it requires no bloodwork or imaging and completed with a quick medical history, a thermometer and a penlight. It has also been validated in family clinic and ED settings and in pediatric populations, thus increasing the utility of this decision rule.4–6
The mnemonic for the Modified Centor decision rule (a.k.a. the McIssac Score) is relatively straight forward: M-CENTOR!
Must be older than 3 years old
Cough — No Cough (+1)
Exudates or Swelling — Tonsillar exudates/swelling (+1)
Nodes — Anterior Cervical adenopathy (+1)
Temperature — Hx of fever or Temperature >38 (+1)
Only Young — patients <15yo (+1)*
Rarely Elder — Patients >45 (-1)
What do the numbers mean?
| Interpretation of Modified Centor Score | |||
| Total Points | Risk Level | Percentage of patients with Strep Pharyngitis (based on cultures) | Suggested Management |
| < 1 | Low risk | 1-10% | No culture or antibiotics necessary, return if worse |
| 2 – 3 | Moderate risk | 10-28% | Culture all, treat if culture result positive |
| > 4 | High risk | 38-63% | Culture all, treat empirically with antibiotics |
Figure 2: Interpretation of Modified Centor Score and subsequent management3.
What to do next?
Recommendations in the original McIssac paper and by the American Association of Family Practice (AAFP) in 2009 were that low risk patients can be discharged home with no further testing or antibiotics indicated.7–8 Moderate risk patients can be offered throat culture or rapid antigen detection test (RADT) and treated if culture/RADT was positive, and high risk patients with scores >4 were to be empirically treated with 10 day course of oral antibiotics – Penicillin VK for us Canadians.8 Erythromycin is commonly patients with a penicillin allergy.8
More recently, the Infectious Disease Society of America (IDSA) 2012 pharyngitis guidelines recommended against empiric antibiotic therapy for acute uncomplicated pharyngitis and to instead offer RADT/throat culture to all moderate and high risk patients and treat them based on results of the tests due to the increase availability and accuracy of RADT as well as low incidence of streptococcal pharyngitis complications such as peritonsillar abscess and rheumatic fever9. This approach would present additional challenges to the Emergency Medicine setting, where low-acuity patients are rarely followed by the ED physician following discharge. Some potential practice patterns include having throat culture results faxed to the ED to be followed up by another colleague, having the patient’s family physician follow up on the throat culture results, and ED physician follow up on the throat culture results on his/her own time. There are advantages and drawbacks to each of these solutions, and would likely depend on ED physician and group preferences/practices.
Some emergency physicians also believe that there is little benefit to routine treatment of uncomplicated streptococcal pharyngitis in adults due to the low incidence of suppurative and non-suppurative complications, and modest evidence of symptom relief – however this a topic outside the scope of the discussion today.10
The Bottom Line:
In summary, the Modified Centor Score is a quick, reliable and useful bedside tool to gauge the risk of streptococcal pharyngitis in a patient with sore throat complaints. As a firm believer keeping mnemonics simple, I recommend to just use the name of the score (M-CENTOR) as the mnemonic!
This post was copyedited by Michael Bravo (@bravbro).
References
Expert Peer Review
Thank you to Richard for a wonderful mnemonic about this very important topic. Choosing wisely around when to prescribe antibiotics and when NOT to do so is an imperative that all of us must take to heart in these coming years. Indeed, everyone MUST do their part to avoid antibiotic overuse, and the likely zombie apocalypse that we may cause if we do not. Antibiotic resistance is a real phenomenon, and it is incumbent on all doctors and trainees to think about the appropriate use of antibiotics. This M-CENTOR mnemonic helps us to more easily remember and apply the McIssac modification of the CENTOR score, and I think that is great. Even in the ED, we should be thinking about how to identify those patients in whom we should consider treating (i.e. post-test probability of about 30-60%), those in which we should hold back and wait for culture results, or those in whom we should provide reassurance and counsel to return if worse. Yes, this might mean for ED docs we have to follow-up on the occasional culture result, or arrange follow-up for a patient’s primary care provider – but all in all, it’s time we all stood up and did our part in the fight against antibiotic overuse!