Chest Pain? Better check out the HEART (Score)!
Chest pain suspected to be of cardiac origin is a common presentation in the first-world Emergency Department, but trying to decide the appropriate level of care of these patients can often be challenging. What if the chest pain is not a straight-forward STEMI that needs to be sent to the cath lab? What do we say when the troponin levels are not high enough to impress the seasoned (and disgruntled) cardiologist at 2 am in the morning? Worse yet, what if the ECG and troponin levels are both normal in a person with a very suspicious history and multiple risk factors?
HEART Score – A Tool For the ED
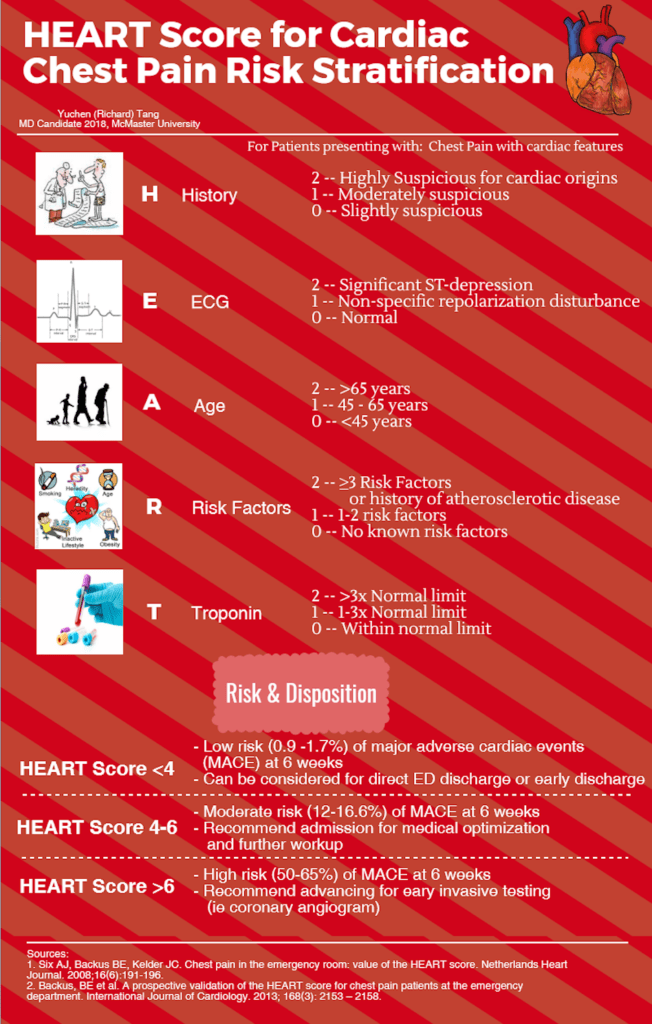
The HEART score is an excellent tool that can be used in the ED setting to prognosticate and triage patients with possible Acute Coronary Syndrome (ACS) for admission for further workup and treatment versus safely discharging home with follow-up instructions. The scoring system is based on expert opinion and validated in several ED populations worldwide. 1 2 Most importantly, the scoring system focuses on disposition via calculating the risk of a Major Adverse Cardiac Event (MACE) within 6 weeks. 1 The HEART score is highly practical for the ED to help focus on identifying low risk as well as high risk patients, in order to offer appropriate care and disposition as early as possible.
The HEART score comes with an inherent mnemonic of HEART (free of charge), making it easy to remember and use.
STOP! Not everyone needs a HEART
However, as with any other score, it is as important to know when to not use this score.
- In patients with a possible STEMI – STEMI should be a clinical diagnosis based on history and ECG results. Waiting for troponin delays door-to-needle time which can lead to poorer outcomes.
- Patients with only an elevated troponin without other risk factors– this generally suggests evidence of myocardial cell death, and whilst this could be due to other causes such as poor cardiac enzyme elimination (ie renal failure) or demand ischemia, they may require at least further workup for the cause of the “troponitis” even if the HEART score is otherwise low.
Sometimes you have to be HEART-less…
Furthermore, we should always be considering the limitations of each clinical decision rule. In this case, it includes:
- What constitutes an acceptable risk? – A false-negative of 2% for MACE in 6 weeks may be acceptable to some patients and physicians, but this could mean that out of every 50 low-risk HEART score patients seen in the ED, 1 will have a major adverse cardiac event. In busy centers, this could mean letting 1-2 patients with a brewing MACE walk out of the ED every day. In comparison with the Wells Score for Pulmonary Embolism, the recommendation has been to use a PERC score or obtain a d-dimer even when in the context of a low-risk Wells score (<2) to further reduce false-negative rates up to 0.5%. 3 Perhaps additional workup (ie a second troponin level) should be pursued further reduce the risk of MACE in conjunction with the HEART score prior to ED discharge.
- Are all components of the HEART score created equal? As previously mentioned, a troponin elevation may be sufficiently concerning to warrant admission for further cardiac workup and optimization. Therefore, are there components of the HEART score (ie history, ECG changes, troponin level) that portend higher risks for MACE?*
*Evidence Update
A Recent study by the HEART score authors compared an adjusted HEART score created based on multivariable regression analysis of 2388 chest pain patients, of whom 407 (17%) had MACE, to the original HEART score. 4 The adjusted HEART score placed a heavier emphasis on the History and Troponin components, where patients can be stratified into the intermediate risk category based on suspicious history or high troponin level alone. When compared to the original HEART score, the adjusted HEART score categorized more non-diseased patients (159/2388) as intermediate risk and identified a small fraction (54/2388) of originally intermediate-risk patients as high-risk. The authors concluded that using an adjusted HEART score had relatively small clinical gain and an increased cost of more medical resource consumption on non-diseased patients and recommended to continue using the original HEART score.
Conclusion
The HEART score is a well validated ED clinical decision tool that helps prognosticate and triage patients who present with chest pain suspicious for cardiac features. It identifies patients who are either already sick or at risk of becoming sick by estimating risk of MACE within 6 weeks of presentation to ED. It also helps identify patients who should stay in hospital for further cardiac workup and those who may be safely discharged due to minimal risk of MACE. It is easy to remember as each letter of the HEART score stands for a component of the heart score – History, ECG, Age, Risk factors, Troponin. Take this HEART score to heart when evaluating patients with possible acute heart problems!
This post was copyedited and uploaded by Jesse Leontowicz (@jleontow). The senior editor for this post was Dr. Teresa Chan (@TChanMD)
References
Reviewing with the Staff
Nice outline of the pearls and pitfalls of the HEART score. Always be smarter than the scoring system. In case of elevated troponin or ischemic ECG with a low HEART score, one should still seriously consider admission and further investigations. For further information and the latest literature on the HEART score, please visit www.heartscore.nl