Case Presentation
Mohammed is an otherwise healthy 58-year-old male presenting with a 24-hour history of palpitations and light-headedness following rigorous exercise. He denies chest pain, shortness of breath, diaphoresis, syncope, or focal neurological symptoms. He has no previous chronic conditions or hospitalizations. No alcohol or drug use.
On exam, Mohammed appears somewhat anxious but is not in distress. He is tachycardic at 130, with vitals otherwise within normal limits. Cardiac exam reveals an irregular and fast heartbeat with no murmurs. No focal neurological deficits are noted. No peripheral edema or distension of JVP is noted. Respiratory and abdominal exams are normal.
ECG: Irregularly irregular QRS measured at 130BPM, no discrete P-waves identifiable. It looks like this:
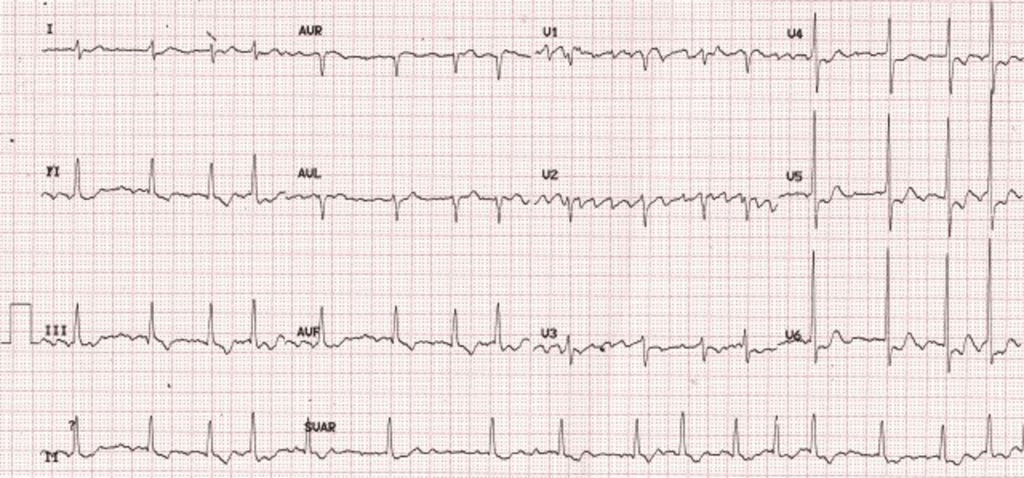
Investigations are ordered and results reviewed. Other than the ECG, all other investigations are unremarkable.
Overview
Atrial fibrillation (AF) is a supraventricular tachycardia in which the atria contract in a rapid and disorganized fashion. Untreated AF can result in life threatening complications including stroke (through the formation and transmission of emboli secondary to blood stasis in the atria), Acute Coronary Syndrome (ACS) (through reduced coronary flow and often rapid ventricular rate), and pulmonary edema/heart failure (through increased pulmonary arterial pressures secondary to increased afterload in the atria). Etiologies of AF are many and a complete discussion is beyond the scope of this article.
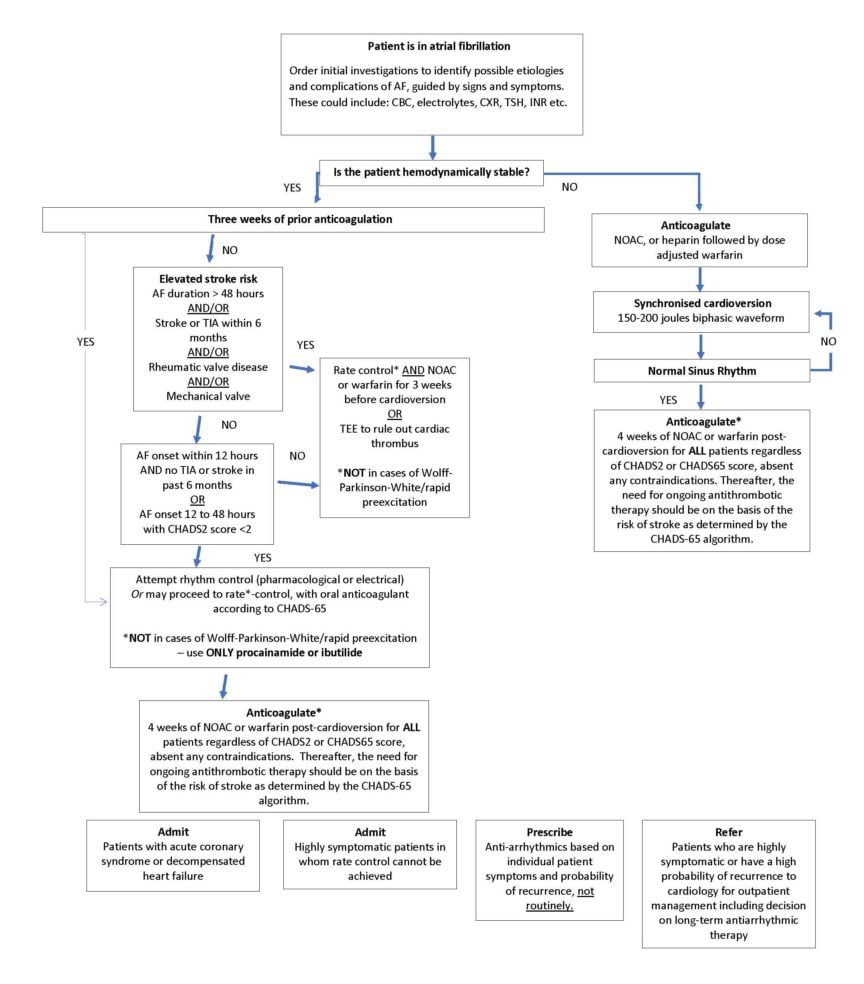
Key points in the management of non-valvular atrial fibrillation (NVAF) in the emergency department (With recent changes from the 2018 CCS Guidelines indicated)1–3
- Immediate DC cardioversion in any patient with hemodynamic instability DIRECTLY CAUSED by their AF (caution: this is rare unless the patient has severely impaired left ventricular function, one must rule out more common causes for hemodynamic instability like sepsis or bleed). Hemodynamic instability includes hypotension, ACS, or pulmonary edema. DC cardioversion should not be delayed by anti-coagulation [Strong Recommendation, Low-quality Evidence].
- For hemodynamically unstable patients, initiate anticoagulation immediately after (and preferably before) cardioversion of AF with NOAC or heparin followed by dose-adjusted warfarin in ALL patients regardless of CHADS2 or CHADS65 score. [Weak recommendation, Low Quality Evidence]
- NEW – In the absence of contraindications, ALL patients undergoing pharmacological or electrical cardioversion should receive at least four weeks of anticoagulation therapy (dose-adjusted warfarin or NOAC). Thereafter, the need for ongoing antithrombotic therapy should be based on the risk of stroke as determined by the CHADS-65 algorithm. [Weak recommendation, Low Quality Evidence]
- NEW – Pharmacological or electrical cardioversion of symptomatic NVAF WITHOUT at least three weeks of prior anticoagulation only in the following cases [Weak Recommendation, Low Quality Evidence]:
- Patients with non-valvular AF with clear onset less than 12 hours ago and no stroke or transient ischemic attack (TIA) in the past 6 months (with any CHADS2 score).
- Patients with non-valvular AF with CHADS2<2 with onset between 12 and 48 hours.
- NEW – Trans-esophageal echocardiography may be used as an alternative to at least three weeks of anti-coagulation prior to cardioversion. [Weak Recommendation, Moderate Quality Evidence]
Approach to Atrial Fibrillation
Note: For an excellent resource, which includes drug and dosing information, please see the CAEP’s Acute Atrial Fibrillation/Flutter Best Practices Checklist4, a product of close collaboration between Canadian emergency physicians, cardiologists, a methodologist, and patients.
The following approach is limited to the emergency department setting. It does not include an exhaustive search for, and treatment of, the causes of AF1–4.

*This recommendation is the subject of some controversy. In a nutshell, the CCS provides this as a “weak recommendation”. The decision to start 4 weeks of anti-coagulation of a CHADS-65 negative patient should include careful consideration of each individuals risk factors and preferences. For a complete discussion, see the commentary “The Canadian Cardiovascular Society 2018 guideline update for atrial fibrillation–A different perspective”5 in the September 2019 issue of CJEM.
Case Conclusion
Mohammed was diagnosed with atrial fibrillation and, based on his symptoms, signs, and investigations, deemed to be hemodynamically stable. He was not previously anti-coagulated but the duration of his AF was less than 48 hours, he has no history of a mechanical valve, rheumatic valve disease, or stroke. His CHADS2 score being <2, the decision was made to proceed directly to DC cardioversion. After one shock, Mohammed reverted to a normal sinus rhythm. As this was his first episode of atrial fibrillation, and probability of recurrence is low, he was not prescribed anti-arrhythmics or referred to a cardiologist for assessment and management.
As he is CHADS-65 negative, there was a discussion between patient and provider on the risks and benefits of four weeks of anti-thrombotic therapy post cardioversion. His provider explained to him that his chance of a bleed on a blood thinner is low, as is his risk of an ischemic stroke if he does not take a blood thinner. Mohammed is an active person, and based on his values and lifestyle, prefers to avoid increasing his risk of a bleeding event. His provider agrees and does not prescribe anti-coagulation.
Staff Review by Dr. Clare L Atzema
“AFib guidelines emphasize the importance of “immediate” DC cardioversion in cases of hemodynamic instability. But anyone who works clinically in the ED knows that there is usually a minute or so to ask questions and gather enough information to help inform your clinical decision to cardiovert the (likely non-anticoagulated) patient. Their instability is much more likely to be secondary to another pathology such as sepsis, GI bleed, pulmonary embolus, an acute coronary syndrome, and so on, rather than the afib they may have been in for years; not always, but usually. In these patients, cardioversion may do more harm than good. Reserve “immediate” DC cardioversion for the rare patient whose instability is DIRECTLY caused by their afib, or in whom you have identified and addressed the other potential causes and they still have ongoing instability. And if you decide to cardiovert these patients, give them some IV heparin as soon as possible, since it has the fastest onset of the OAC options.”
Appendix 1: CHADS-2 and CHADS-65 Risk Scores6
CHADS-2
| Risk Factor | Score |
| Congestive heart failure history | +1 |
| Hypertension history | +1 |
| Age equal to or greater than 75 years | +1 |
| Diabetes mellitus history | +1 |
| Stroke or transient ischemic attack history | +2 |
CHADS-65
(if all NO, can generally rule out need for anti-thrombotic therapy in atrial fibrillation/flutter)
| Risk Factor | Score |
| Age greater than or equal to 65 | YES/NO |
| Stroke OR transient ischemic attack OR hypertension OR heart failure OR diabetes mellitus | YES/NO |
| Coronary artery disease or arterial vascular disease (coronary, aortic, peripheral) | YES/NO |
This post was copy-edited by @alexsenger
References
- 1.Andrade J, Verma A, Mitchell L, et al. 2018 Focused Update of the Canadian Cardiovascular Society Guidelines for the Management of Atrial Fibrillation. Can J Cardiol. 2018;34(11):1371-1392. doi:10.1016/j.cjca.2018.08.026
- 2.Verma A, Cairns J, Mitchell L, et al. 2014 focused update of the Canadian Cardiovascular Society Guidelines for the management of atrial fibrillation. Can J Cardiol. 2014;30(10):1114-1130. doi:10.1016/j.cjca.2014.08.001
- 3.Gillis A, Verma A, Talajic M, Nattel S, Dorian P, CCS Atrial Fibrillation Guidelines Committee. Canadian Cardiovascular Society atrial fibrillation guidelines 2010: rate and rhythm management. Can J Cardiol. 2011;27(1):47-59. doi:10.1016/j.cjca.2010.11.001
- 4.Stiell IG, Scheuermeyer FX, Vadeboncoeur A, et al. CAEP Acute Atrial Fibrillation/Flutter Best Practices Checklist. CJEM. April 2018:334-342. doi:10.1017/cem.2018.26
- 5.Stiell IG, McMurtry MS, McRae A, et al. The Canadian Cardiovascular Society 2018 guideline update for atrial fibrillation – A different perspective. CJEM. September 2019:572-575. doi:10.1017/cem.2019.399
- 6.Stroke Prevention in Atrial Fibrillation. Thrombosis Canada. http://thrombosiscanada.ca/wp-content/uploads/2017/10/Stroke-Prevention-in-Atrial-Fibrillation_2017Oct15.pdf. Published 2017. Accessed March 2020.