Case:
Tom is a 38-year-old male who presents to the ED with a red left eye. It started yesterday at work and has been getting more painful. He describes feeling like something is stuck in his eye, despite washing it multiple times. His vision is “a bit blurry” in the left eye. He wears contact lenses occasionally, but mostly wears glasses. He denies headache.
Past medical history is significant for seasonal allergies, asthma, and genital herpes. He works as a car mechanic.
What is your differential diagnosis for corneal disorders in the ED? What physical exam and slit lamp findings would you look for?


Return to the Case
After a quick scroll through CanadiEM, you return to your patient Tom. You attempt to examine him but he screams “don’t touch my eye doc!”. You apply topical tetracaine, which improves his pain drastically. After 2 minutes, he allows you to examine him.
On inspection, you see a red left eye with watery discharge. His visual acuity is 20/20 bilaterally. His extra-ocular movements are normal and pupils are reactive. You move onto a slit lamp exam, carefully talking through the steps with the patient. Using plain diffuse light, you look under the eyelids, and then at the cornea. There is mild conjunctival injection but you do not see any hyphema, pus, or foreign body.
You then instill fluorescein drops into the eye, and switch the slit lamp to the cobalt blue filter. This is what you see.10
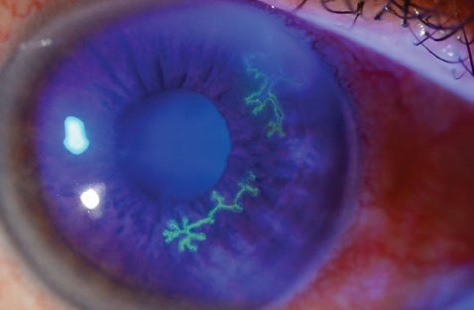
Based on the slit lamp findings, you diagnose Tom with herpes simplex keratitis. You give him a prescription for Valacyclovir 1 g TID, arrange next day ophthalmology follow-up, and give him return instructions to come back if his pain worsens or vision deteriorates.
This post was copyedited and uploaded by Kimberly Vella.
References
- Walker R, Adhikari S. Eye Emergencies. In: Tintinalli’s Emergency Medicine. New York, NY: McGraw-Hill Education.; 2015:1543–1579.
- How to diagnose and manage corneal abrasions and bacterial ulcers. eyeguru.org. https://eyeguru.org/essentials/corneal-abrasions-ulcers. Published 2019. Accessed August 25, 2019.
- Knoop K, Stack L, Storrow A, Thurman R. The Atlas of Emergency Medicine. 4th ed. New York, NY: McGraw-Hill Education.; 2016.
- Karr D. Ocular Laceration. . Cancer Therapy Advisor. https://www.cancertherapyadvisor.com/home/decision-support-in-medicine/pediatrics/ocular-laceration/. Published 2017. Accessed January 17, 2019.
- Roat M. Superficial Punctate Keratitis – Eye Disorders. Merck Manuals. https://www.merckmanuals.com/en-ca/professional/eye-disorders/corneal-disorders/superficial-punctate-keratitis. Published 2018. Accessed August 2019.
- Njoya JM, Handor H, Lezrek O, Hafidi Z, Sabrane I, Daoudi R. Herpetic epithelial keratitis. QJM. December 2014:595-595. doi:10.1093/qjmed/hcu250
- Roat M. Herpes Zoster Ophthalmicus – Eye Disorders. Merck Manuals. https://www.merckmanuals.com/en-ca/professional/eye-disorders/corneal-disorders/herpes-zoster-ophthalmicus. Published 2018. Accessed 2019.
- Shaikh S, Ta C. Evaluation and management of herpes zoster ophthalmicus. Am Fam Physician. 2002;66(9):1723-1730. https://www.ncbi.nlm.nih.gov/pubmed/12449270.
- Trobe J. The Physician’s Guide to Eye Care. San Francisco, CA: American Acad. of Ophthalmology; 2012.
- Sterling J. Herpes simplex virus . Jeffrey Sterling, MD. https://www.jeffreysterlingmd.com/tag/herpes-simplex-virus/. Published 2018. Accessed 2019.
Reviewing with the Staff
As with all things in emergency medicine, a thorough history and physical is worth its weight in gold. Patients with painful eyes are often anxious. Early topical anesthetic can help ease the discomfort of the rest of the examination. As well, talking the patient through each portion of the examination often reassures the patient and helps them follow instructions easier. This will further facilitate a better quality examination. Finally, make sure to wear gloves and wash your hands thoroughly, as these pathogens can be extremely contagious!



