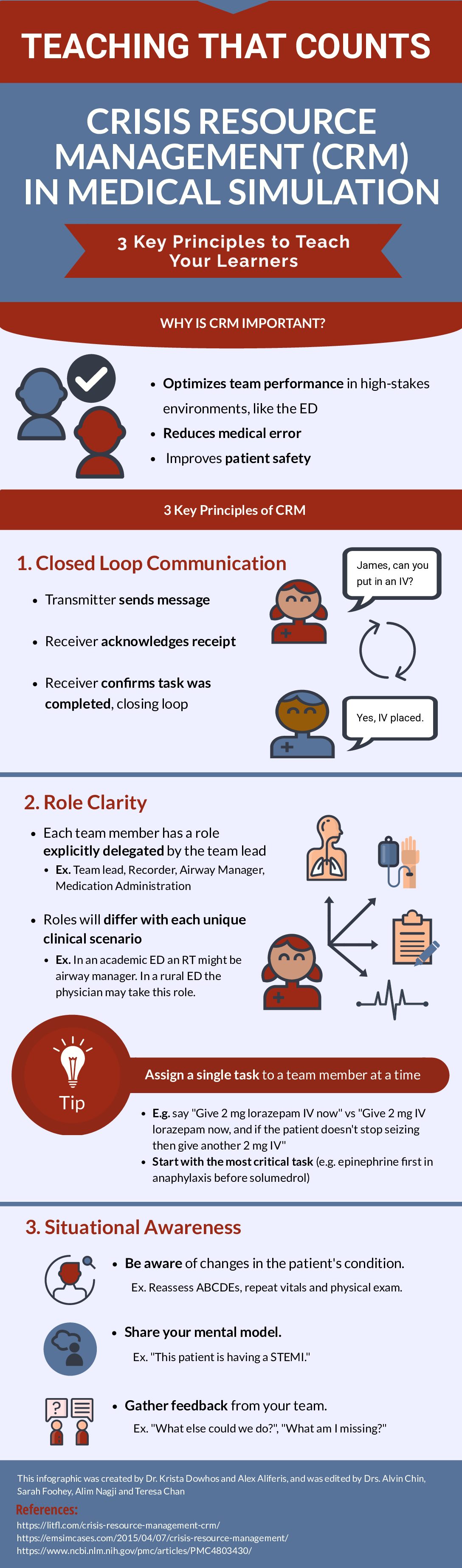
This is part of the CanadiEM Teaching That Counts Infographic Series, where we take the current research and evidence on how to teach well in the emergency department, and distill it down into bite-sized chunks that are rapidly digestible and memorable.
We all know that Crisis Resource Management (CRM) is an important skill. When done well, it enhances team performance, reduces medical error, and improves patient safety. But like many other non-technical skills, CRM can be hard to teach. It is a complex set of skills that involves interpersonal interactions, integration and translation of data, and resource utilization. If there was ever a moment to ditch the “see one, do one, teach one” model, your CRM teachable moment would be it! In this issue of Teaching That Counts, we break down three important principles of CRM into bite-sized pieces. We put it in infographic format for you to use during your next CRM teachable moment, to give to your learners as pre-reading before a simulation session, or to post in your sim lab or resuscitation room for some “just-in-time” review of CRM principles.
3 Key Principles of CRM
1. Closed Loop Communication (CLC)
Most learners will already be able to recognize that communication is foundational to responding to any crisis, but exactly what that looks like when stakes are high may not be clear. Explain CLC in three steps: 1) Team member #1 sends a message, making it clear who they are speaking to (e.g. Team lead says “James, can you put in an IV?”), 2) Team member #2 acknowledges receipt and 3) Team member #2 confirms, outloud, that the task was completed (e.g. “Jessica, I have placed an IV”). Your learner may find this method of communicating awkward or unnecessary, but by relying on step 3 (closing the loop) the learner can decrease their cognitive load as they don’t have to worry about if and when a task is completed.
2. Role Clarity
In real life situations, team members often assume their roles without explicitly being told. In simulation, all roles need to be explicitly delegated by the team lead. This is important as it increases the learner’s awareness of resources (both personnel and equipment) available to them. For example, during a simulation taking place in a rural setting with two nurses and no RTs, they may not be able to delegate airway management and need to perform this task themselves. It also helps them understand the implications of delegating tasks to team members. For example, delegating CPR to a nurse means he or she is not available to administer medications. Ask your learner to assign roles to everyone in the room at the outset of every case.
3. Situational Awareness
This principle might be one of the most difficult for your learner, especially if they are junior. It involves the integration of data from multiple sources, recognizing and avoiding cognitive errors, and anticipating likely events in situations the learner may not have had any exposure to. To make this skill more approachable, give the learner specific examples of how to increase situational awareness that they can rehearse during a simulation. Here are three ways a learner can increase their situational awareness during simulation:
Frequent reassessment
By forcing themselves to repeat a physical exam or ask for repeat vital signs intermittently throughout the case, the learner can pick-up on changes in the patient’s condition that may have otherwise gone unnoticed.
Share your mental model
Ask the learner to summarize what is going on with the patient and what they want to do next. Have them do this at least once throughout the simulation, any time they feel “stuck”, or whenever a major intervention is about to occur for the patient. For example, “we have an elderly female who is hyperthermic at 41 degrees celsius with an altered level of consciousness. Next, I would like to start cooling this patient”. This gets the learner to commit to a plan, and allows others to speak up if they have other suggestions.
Gather feedback
After every incidence of sharing your mental model, gathering feedback should follow. For example, “we have an elderly female who is hyperthermic at 41 degrees celsius with an altered level of consciousness. Next, I would like to start cooling this patient. Does anyone have anything to add or change about that plan?” This step can correct cognitive errors (e.g. fixation bias) and contributes to team functioning by making team members feel respected. It also gets the learner comfortable asking for advice during high stakes scenarios, a skill that will help them and their patients for years to come.
Practicing Crisis Resource Management skills in a safe environment like sim is a way for learners to get more comfortable taking on a leadership role during high stakes situations. These skills can seem unnatural or abstract, and it may be the first time your learner has heard of them. Break them down into concrete, actionable steps so that they can learn Crisis Resource Management and really make it count!

References
Nickson, C. (2020). “Crisis Resource Management” Life in the Fast Lane. https://litfl.com/crisis-resource-management-crm/
Caners, K (2015). “Crisis Resource Management” EM Sim Cases. https://emsimcases.com/2015/04/07/crisis-resource-management/
Murray, W. et al (2002) “Leadership Training: A New Application of Crisis Resource Management and Distance Education in a Large Group Format at a Medical Simulation Facility” Journal of Education in Perioperative Medicine, 4(2): E021. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4803430/