You are dispatched to Jasmine, a 31yo patient, for palpitations. On arrival, you find her clinically stable in a narrow-complex, regular tachycardia at a rate of 180bpm. As you begin to coach her through vagal maneuvers and reach for your adenosine she advises you ‘I have something called Wolff-Parkinson-White – does that change anything?’ You think maybe it does, but you’re not sure.
[bg_faq_start]About Sirens to Scrubs
Sirens to Scrubs was created with the goal of helping to bridge the disconnect between pre-hospital and in-hospital care of emergency patients. The series offers in-hospital providers a glimpse into the challenges and scope of practice of out-of-hospital care while providing pre-hospital providers with an opportunity to learn about the diagnostic pathways and ED management of common (or not-so-common) clinical presentations. By opening this dialogue, we hope that these new perspectives will be translated into practice to create a smoother, more efficient, and overall positive transition for patients as they pass through the ED doors.
[bg_faq_end]Objectives
- Review the physiology of Wolff-Parkinson-White Syndrome (WPW)
- Review the management of SVT in WPW and consider potential complications
What are WPW and AVRT?
Preexcitation describes the situation in which impulses from the SA node or atrium reach the ventricle through an accessory pathway (a bypass tract) in addition to the AV node. WPW is a type of preexcitation syndrome in which there are ECG findings of an atrial-ventricular bypass tract (often, but erroneously, called Kent bundles) and the patient demonstrates related tachydysrhythmias. The most common tachydysrhythmia seen in WPW is atrioventricular re-entrant tachycardia (AVRT) – this is seen in 80% of patients with WPW and is what paramedics would most commonly be called for.
Recall that there are three mechanisms for the development of cardiac dysrhythmias:
- Triggered activity – abnormal impulses that result from afterdepolarizations (fluctuations that occur in the membrane potential as the cell repolarizes).
- Enhanced automaticity – depolarizations that either occur spontaneously in nonpacemaker cells (which wouldn’t normally depolarize spontaneously) or in pacemaker cells, but at a lower stimulation threshold than usual.
- Reentrant rhythms – conduction of impulses through a self-sustaining circuit within the heart. These circuits can be at the micro- or macro-level.
AVRT is a type of macro re-entrant tachycardia, in which the impulses travel down one pathway and up through another. In most cases, the impulses travel down through AV node and up through the accessory pathway – this leads to a narrow-complex rhythm because the impulses are travelling rapidly as they normally would through the His-Purkinje system then return to the atria via the AV bypass tract. This situation is called orthodromic AVRT. Occasionally (in 5 to 10% of patients with WPW), the impulses travel to the ventricles through the bypass tract and return to the atria via the AV node. In this case, the QRS complex will be wide, as ventricular depolarization is taking place through muscle-to-muscle conduction rather than the His-Purkinje system.
What are the ECG findings of AV preexcitation?
Most AV bypass tracts are capable of conducting impulses both anterogradely (atria to the ventricles) and retrogradely (ventricles to the atria). As long as the AV bypass tract conducts in the anterograde fashion, the bypass tract is called manifest, as it is often (but not always) seen on resting ECG when the patient is in normal sinus rhythm. Occasionally, a pathway may conduct only in a retrograde fashion, in which case it is not being used when the patient is in normal sinus rhythm and there are no ECG changes at rest (this is called a concealed pathway).
Classic ECG findings in WPW include:
- Short PR interval, >120ms (because the impulse is reaching the ventricles first through the fast accessory pathway, then through the slower AV node)
- Delta wave (a slurring upstroke of the QRS that is caused by the fusion of the early, pre-conducted impulse with the late, AV-node-conducted impulse)
- Wide QRS, >120ms (also caused by the fusion of the early, pre-conducted impulse with the late, AV-node-conducted impulse)
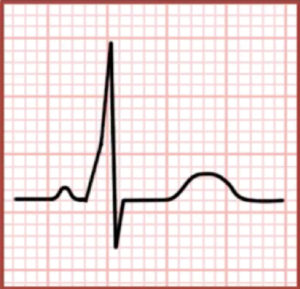
It is important to note that features of WPW are not seen when the patient is in orthodromic AVRT because the impulses are travelling down the AV node only and are using the accessory pathway for retrograde conduction only (given the rapid rate, the accessory pathway is refractory at the time that the impulse is travelling back to the ventricles).
What is the concern with giving adenosine to a patient with WPW that is in SVT?
Adenosine acts primarily by blocking conduction through the AV node. The goal of treating patients in SVT with adenosine is to break the self-sustaining circuit by blocking one arm of the circuit so that when the impulses reach the atria they are unable to travel down the AV node. Since the accessory pathway has just been used for retrograde conduction of the impulse, it remains in its refractory period and the impulse, and re-entry rhythm, die out. This allows normal, unidirectional conduction to restart.
The concern with using adenosine in patients with WPW is that if the AV node is blocked than impulses from the atria will be able to reach the ventricles at a very rapid rate, since they are not slowed down through the accessory pathway as they are at the AV node. Rapid ventricular rates (ventricular tachycardia or ventricular fibrillation) lead to incomplete ventricular filling, poor output, and cardiac arrest. This is why AV nodal blockers are contraindicated in patients with WPW and atrial fibrillation, which can see atrial rates up to 600bpm. The AV node usually blocks most of these impulses, so the ventricles see only a portion and are able to maintain adequate filling time and cardiac output. If the AV node is blocked in a patient with atrial fibrillation and an accessory pathway, the ventricles will see each and every one of these, which will lead to ventricular fibrillation.
But what about patients in regular, narrow-complex tachycardia like Jasmine? It should be safe to use adenosine in her right? It will block the AV node, terminate the re-entry rhythm as described in the first paragraph of this section, and allow a normal sinus rhythm to take over – right? Right. Usually. Sort of. But not always. Ask many emergency providers and they will have a story for you about a WPW/SVT that was treated with adenosine and quickly deteriorated into a very scary ventricular tachyarrhythmia. The reason for this isn’t entirely clear, but may be multifactorial:1
- The patient may have multiple accessory pathways (5 to 10% of patients with bypass tracts). Blocking the AV node in this case just causes the re-entry rhythm to move to involve bypass tracts only (which conduct very quickly)
- Another underlying tachydysrhythmia. 50% of patients with WPW also have paroxysmal atrial fibrillation, 60% have atrial flutter (which can see atrial rates of up to 300bpm), and others have atrial tachycardia. Blocking the AV node may break the re-entrant circuit associated with the AV bypass tract, but if there is an underlying supranodal tachycardia, this will also lead to rapid conduction of too many atrial beats for the ventricles to handle.
- Adenosine is recognized to actually trigger atrial tachyarrhythmias, including atrial fibrillation, atrial tachycardia, and atrial fibrillation – even in patients without WPW. If an atria tachydysrhythmia occurs after administering adenosine, while the AV node is still blocked, the rhythm may deteriorate into a rapid, non-perfusing ventricular response.
How should you manage Jasmine?
Despite the complications just discussed, the recommended approach to managing SVT in the context of WPW is the same as approaching any narrow complex tachycardia.2 The one thing I might change going forward is to have the defibrillation pads applied to the patient in advance of giving the adenosine – just in case!
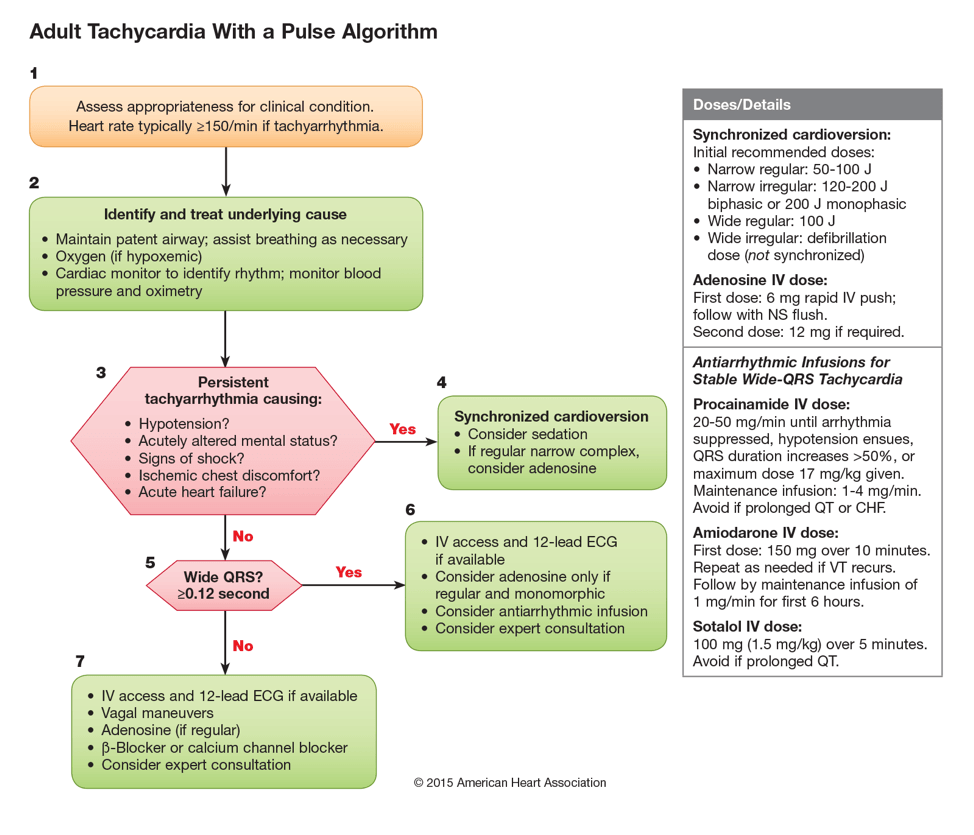
2015 AHA guidelines on the management of tachycardia3
Specifically, the AHA recommendations for acute treatment of orthodromic AVRT include:4
- Vagal maneuvers are recommended (Class I recommendation);
- Adenosine is beneficial (Class I recommendation), but electrical cardioversion should be available in case of deterioration into atrial fibrillation with rapid ventricular response;
- Synchronized cardioversion should be performed for acute treatment in hemodynamically unstable patients with AVRT if vagal maneuvers or adenosine are ineffective or not feasible (Class I recommendation);
- Synchronized cardioversion is recommended for acute treatment in hemodynamically stable patients with AVRT when pharmacological therapy is ineffective or contraindicated (Class I recommendation);
- Synchronized cardioversion should be performed for acute treatment in hemodynamically unstable patients with preexcited atrial fibrillation (Class I recommendation);
- Ibutilide or IV procainamide is beneficial for acute treatment in patients with preexcited atrial fibrillation who are hemodynamically stable (Class I recommendation);
- IV diltiazem, verapamil, or beta blockers can be effective for acute treatment in patients with orthodromic AVRT who do not have preexcitation on their resting ECG during sinus rhythm (Class IIa recommendation);
- IV beta blockers, diltiazem, or verapamil might be considered for acute treatment in patients with orthodromic AVRT who have preexcitation on their resting ECG and have not responded to other therapies (Class IIb recommendation);
- Intravenous digoxin, intravenous amiodarone, intravenous or oral beta blockers, diltiazem, and verapamil are potentially harmful for acute treatment in patients with pre-excited AF (Class III recommendation)
Interestingly, Adenocard (the brand name adenosine product) specifically lists SVT associated with WPW as an indication for its use.5
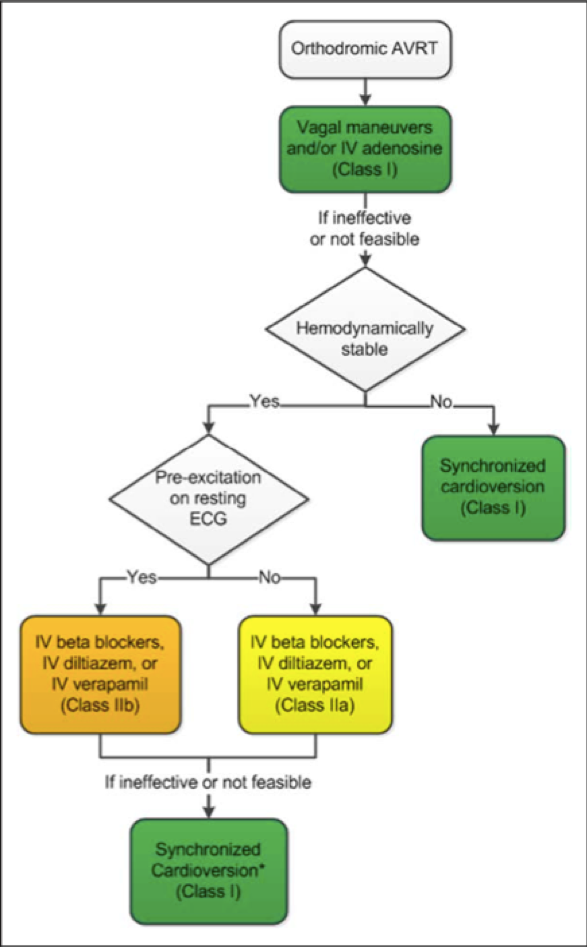
AHA algorithm for the acute treatment of orthodromic AVRT4
That’s it! If you have any questions, thoughts, alternative perspectives, or requests for future topics, feel free to comments below or send me an email at [email protected]. Please keep in mind that, although I will do my best to publish information that is accurate across Canada, there will inevitably be some regional differences in both pre-hospital and in-hospital management of emergency patients. As a paramedic and Emergency Medicine resident in Ontario, some posts may wind-up being somewhat Ontario-centric, hence, I encourage anyone whose experiences differ from mine to contribute to the conversation by commenting below.
Click here for more articles in the Sirens to Scrubs series!
- 1.Mallet ML. Proarrhythmic effects of adenosine: a review of the literature. Emergency Medicine Journal. July 2004:408-410. doi:10.1136/emj.2004.016048
- 2.Biase L, Walsh E. Treatment of symptomatic arrhythmias associated with the Wolff-Parkinson-White syndrome. UpToDate. https://www.uptodate.com/contents/treatment-of-symptomatic-arrhythmias-associated-with-the-wolff-parkinson-white-syndrome. Published September 17, 2018. Accessed May 23, 2019.
- 3.Web-based Integrated Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care – Part 7: Adult Advanced Cardiovascular Life Support. American Heart Association. https://eccguidelines.heart.org/. Published 2015. Accessed May 23, 2019.
- 4.Page RL, Joglar JA, Caldwell MA, et al. 2015 ACC/AHA/HRS Guideline for the Management of Adult Patients With Supraventricular Tachycardia. Circulation. April 2016. doi:10.1161/cir.0000000000000311
- 5.Adenocard Product Monograph. Astellas Pharma Canada, Inc. https://www.astellas.ca/Uploads/pdf/2014-09-15-%20Adenocard%20PM%20-%20Approved.pdf. Published August 15, 2014. Accessed May 23, 2019.

