You are halfway through your very first Emergency Medicine shift. You have a 23 year old male patient who appears to be a slam dunk for acute appendicitis – he has symptoms that are consistent with the presentation, pain on palpation at McBurney’s point, a high white count, and CT findings of appendicitis. Your staff is being pulled in a thousand different directions, and asks you if you feel comfortable calling General Surgery for a consultation. You’ve never called a consultant before and feel nervous doing so. How do you effectively present your case to a consultant?
Always plan ahead
Approximately 40% of all Emergency Department visits require a consultation. As such, being able to effectively communicate with colleagues and request a consultation is a vital skill for any clinician working in the ED.1 Learning to efficiently request consults not only helps facilitate faster dispositions, a key skill when dealing with the high patient load in the ED, but it also has a major impact on patient care, most notably improving patient safety and error reduction. Despite its importance, requesting a consult is a skill that is rarely emphasized in medical school. This blog post will walk you through how to request a consultation from any specialist in an organized and effective manner.
There is no “I” in team
At baseline, the Emergency Department is a challenging environment for requesting a consult, and there are many reasons for why it may not go as planned. This includes issues on the part of the caller, issues on the part of the consultant, and external factors. With respect to issues on the part of the caller, if the consultee lacks the proper training for requesting a consult or is unprepared (e.g. has no clear clinical question for the consultant and/or does not have all of the relevant patient data accessible when making the call), the consult request may become messy and ineffective. Additionally, factors on the part of the consultant also play a role; these include being busy, disengaged, or self-serving, as well as the consultant failing to collaborate or being known for being a difficult consultant. External factors, such as perceived time stress in the ED, can also make requesting a consultation more difficult. Overall, calling a consultant is a difficult task, and as a junior learner this is sometimes further stressed by having to navigate complex hospital hierarchies.
There are a number of ways to mitigate these challenges. Try to remember that you and the consultant are on the same team, and invite an in-person discussion whenever possible. Never disparage the consultant to others and always take the time to thank the consultant for their assistance. This will go a long way in helping to keep things more amicable between you and the consultant. Additionally, a study performed by Chan et al. in 2013 found that familiarity and trust are two factors that strongly influence the referral-consultation process and relationship.2 Given that both of these factors require time to develop, this can be challenging as a learner on an Emergency Medicine rotation. However, it is still important to keep these things in mind when moving forward into your career.
How to approach the consult
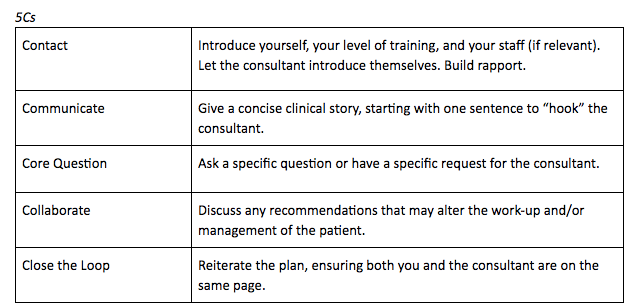
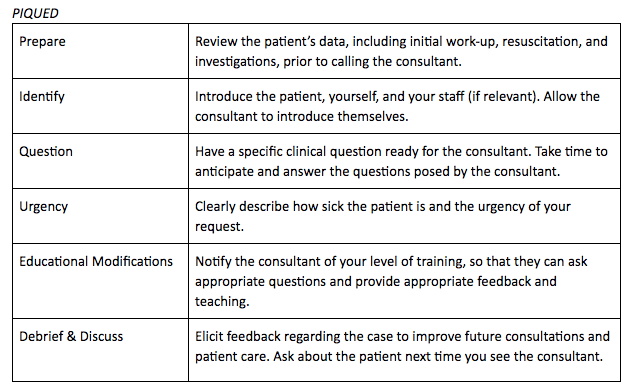
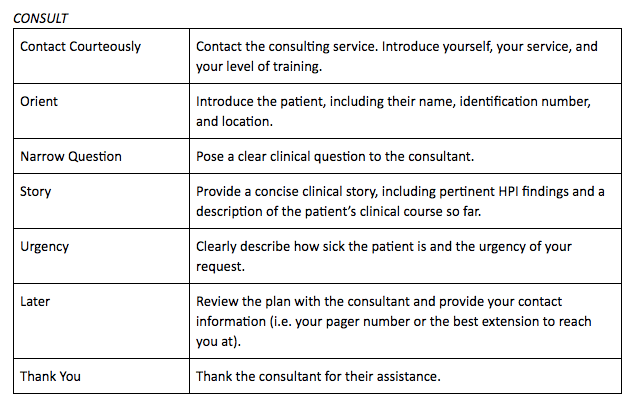
Perhaps the most important factor that will help your consultation requests go more smoothly is having a consistent and organized approach when calling a consultant. A number of different frameworks for requesting consultations have been developed, including the 5Cs, PIQUED, and CONSULT models.3 These cards on ALiEM provide a great overview of these three approaches and are useful resources. However, we will walk you through each of these approaches here as well.
All three of these frameworks have been studied and validated:
- The 5Cs model was studied extensively in medical students and has the largest body of evidence for improving the quality of consultation requests
- The PIQUED framework includes educational modifications and debriefing, allowing for more learning opportunities from each consultation request
- CONSULT is the newest model, and has been found to be beneficial after just one hour of teaching
Overall, all three models are effective in improving the ability of learners to request consultations; the most important choice as a learner is to find which approach works best for you and to stick with it. Having a consistent approach when calling a consultant will greatly improve the organization and effectiveness of your requests.4,5
Key takeaways
Although each of these three approaches are slightly different, they all have a number of core similarities. These similarities provide us with hints as to which elements are especially critical when making a consultation request. Here are key takeaways:
- Prepare, prepare, prepare: before calling a consultant, make sure that you have a specific clinical question and a one liner prepared to “hook” the consultant. Additionally, ensure that you have all of the patient’s data in front of you, including old charts, lab and imaging results, the names of previous specialists, the dates of previous procedures/important investigations, and any other pertinent clinical information. This will allow you to present a concise clinical story to the consultant and be prepared to answer any questions the consultant may ask.
- Introductions: when starting the call, introduce yourself, your level of training, your service, and the patient. This will help build familiarity between you and the consultant.
- Open strong: following introductions, start with the one liner you prepared. Then pose your clear clinical question to the consultant before providing a concise story – this will help the consultant orient themselves and decide which information is most important as they listen to your story.
- Close the loop: before hanging up the phone, reiterate the plan to ensure that both parties are on the same page with respect to next steps. Closed loop communication is critical in ensuring that everyone leaves the conversation with the same expectations and understanding.
- Thank the consultant: being polite and providing thanks will go a long way towards improving collegiality and developing a good relationship with the consultant!
It’s also important to note that certain elements of your consultation request will differ depending on which service you are consulting because different specialties prioritize different information. For example, it’s important to include information regarding birth history, developmental status, and immunization history when presenting your case to a pediatrician, whereas an orthopedic surgeon will care more about the mechanism of injury and neurovascular status of the injured limb. Prior to picking up the phone, try to place yourself in the consultant’s shoes and think about what information you would want if you were working for that service. Also check out this Referral Cheat Sheet created by Dr. Charlotte Durand; she provides a great overview of the key elements to include when requesting a consultation from the different services.
Practice practice practice!
Now that we’ve talked about the three common approaches for requesting a consultation and some key takeaways to keep in mind, it’s your turn to practice — use the practice case below to try out the three different frameworks (5Cs, PIQUED, and CONSULT) and choose which one works best for you. Having a consistent approach to requesting a consultation will go a long way towards helping you perform effective consult requests and achieve overall success on your EM rotation. Happy practicing!
It’s 2pm and your latest patient is a 57 year old female with a 4-day history of melena. She has no history of hematochezia or N/V. She looks generally well and is afebrile with a HR of 84, BP of 105/75, RR of 16, and O2 sat of 98% on room air. Her physical exam reveals epigastric tenderness and evidence of melena on DRE, but is otherwise unremarkable with no evidence of stigmata of chronic liver disease. Her current hemoglobin level is 85; her hemoglobin level three months ago was 118. Her last meal was eggs and toast for breakfast around 8:30am. Her PmHx is significant for type 2 diabetes, osteoarthritis, and hypercholesterolemia. No prior history of GI bleed or ulcer. Her medications include metformin and atorvastatin, although she does also admit to using Advil regularly to help with her joint pain (often taking 6 extra strength Advil per day for the past 5 months). She drinks approximately 7 drinks of EtOH per week and does not smoke or use recreational drugs. You and your staff feel confident that this is an upper GI bleed, and believe that she will need a scope to investigate further. Your staff asks you to consult GI.
Practice how you would approach requesting this consultation using each of the 3 frameworks described in this blog post (5Cs, PIQUED, and CONSULT) to find out which one works best for you!
- 1.Chan T, Bakewell F, Orlich D, Sherbino J. Conflict Prevention, Conflict Mitigation, and Manifestations of Conflict During Emergency Department Consultations. Yarris LM, ed. Acad Emerg Med. Published online March 2014:308-313. doi:10.1111/acem.12325
- 2.Chan T, Sabir K, Sanhan S, Sherbino J. Understanding the Impact of Residents’ Interpersonal Relationships During Emergency Department Referrals and Consultations. Journal of Graduate Medical Education. Published online December 2013:576-581. doi:10.4300/jgme-d-12-00211.1
- 3.Baylis J, Miloslavsky EM, Woods R, Chan TM. Conquering Consultations: A Guide to Advances in the Science of Referral-Consultation Interactions for Residency Education. Annals of Emergency Medicine. Published online July 2019:119-125. doi:10.1016/j.annemergmed.2018.12.004
- 4.Chan T, Orlich D, Kulasegaram K, Sherbino J. Understanding communication between emergency and consulting physicians: a qualitative study that describes and defines the essential elements of the emergency department consultation-referral process for the junior learner. CJEM. 2013;15(1):42-51. doi:10.2310/8000.2012.120762
- 5.Kessler C, Afshar Y, Sardar G, Yudkowsky R, Ankel F, Schwartz A. A prospective, randomized, controlled study demonstrating a novel, effective model of transfer of care between physicians: the 5 Cs of consultation. Acad Emerg Med. 2012;19(8):968-974. doi:10.1111/j.1553-2712.2012.01412.x
Reviewing with the Staff
This is a really, really good overview for junior learners - really for learners of all levels! Being courteous, being organized, and having an approach to this skill is an essential core competency of what we do from day to day!
For those of us who are in academic centres, I will add a proviso that as a more senior trainee or an attending that the “Educate” part of the PIQUED model can go both ways. Remember that when you are a senior trainee in the emergency department, or an attending physician, sometimes you will be “consulting” a more junior colleague who is apprenticing under their staff physician or surgeon. When calling for consults in this circumstance, it is really important to bear in mind that our junior consultants sometimes need more support than their senior counterparts. My approach to this is to consider the other person is someone who is still learning and will need my assistance in making sure that the patient as well-tended-to while they are assessing and reviewing the case. Until the new attending physician is involved (either by direct assessment or by phone review) and the patient is admitted - I always make sure that our junior consulting colleagues feel like welcomed guests in the ED, and check in on them even after their arrive. This has really helped with generating effective rapport and more effective relationships between services and can have pay offs in the long run.




