This post about how to perform a hip nerve block was created as part of the 2020 Manitoba Emergency Medicine Research Day 2.0 FOAMed competition. The authors have no disclosures of funding or conflicts of interest.
Having a healthy understanding of regional anesthesia changes the game in Emergency Medicine. Whether you are relocating joints, fishing glass out of heels, or providing analgesia for painful fractures, depending less on narcotics and procedural sedation can be good for patients and good for your department. A hip nerve block for a proximal femur fracture is the perfect example.
Objectives:
- Recognize the prognostic severity and impact of hip fractures in elderly patients
- Understand the innervation of the hip capsule
- Know the various ultrasound-guided regional anesthesia choices for hip fractures
- Develop awareness of possible procedural complications
The fall is only the beginning
As the population ages, we will no doubt encounter an increasing number of patients with hip fractures. At the turn of the century, the world was already experiencing over 1.5 million proximal femur fractures per year!1 These injuries are painful, and we do a poor job of adequately addressing that pain while balancing the risks of over or under treatment.2 Considering 10% of patients with a hip fracture die within the first month and one third die within the year3, many quality improvement papers have explored various strategies for the management of pain in order to improve care and reduce the risk of related adverse events, such as rehab delays, delirium, and prolonged hospital stays.
Why we hurt
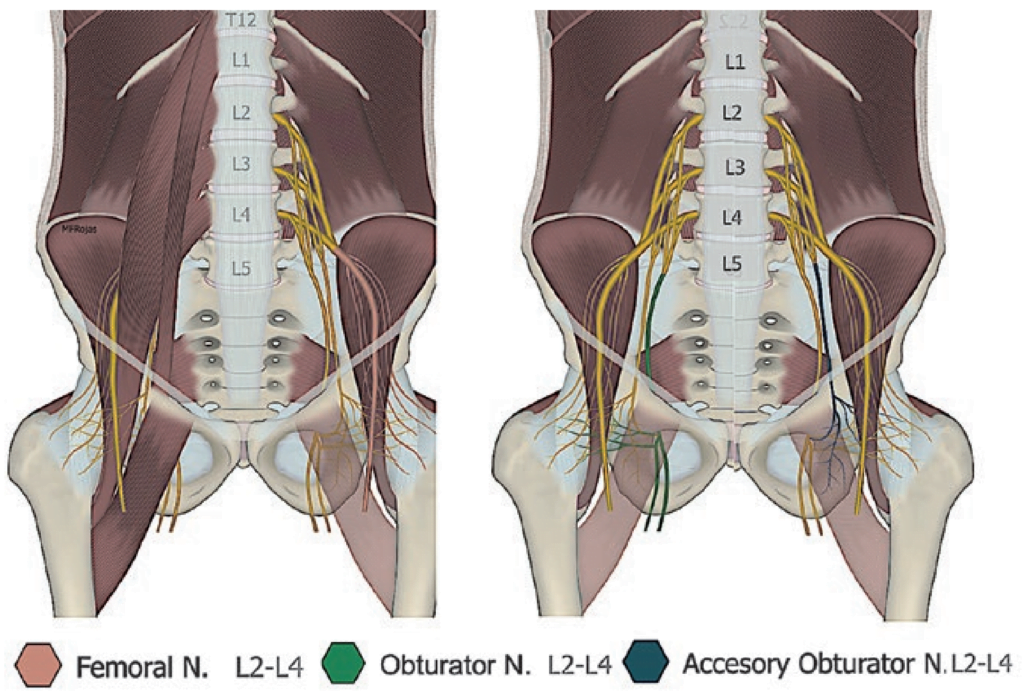
The most richly innervated part of the hip joint is the anterior capsule, with three major nerves playing a role in pain: the Femoral Nerve (FN), Obturator Nerve (ON), and Accessory Obturator Nerve (AON).4
How we access these nerves has become more elegant through medical history. In years past, blind groin pokes feeling for a “double pop” were used (gasp), but thankfully we live in the age of bedside ultrasound. Ultrasound-guided nerve blocks of the hip performed by emergency physicians are feasible and effective procedures.5,6 Let’s make sure at least one technique for a hip nerve block is within your wheelhouse!
Ditch the narcotics and pull out your probes
In all of the below techniques, the patient should be supine with the affected leg slightly abducted and ideally, externally rotated. In all techniques, the view is obtained with an ultrasound probe in transverse axis and the needle is inserted laterally using in-plane technique.
Images in the following sections are curtesy of NYSORA.com, which allows open and free use of their content.
[bg_faq_start]1) Femoral Nerve Block
External Landmark
- Femoral crease, distal to the inguinal ligament
Internal Landmark
- Femoral Artery and Vein
- Pro Tip: If you are too distal, you will see the Deep Artery of the Thigh (DAT) coming off the Femoral Artery (FA)

Too distal. 
Just right.
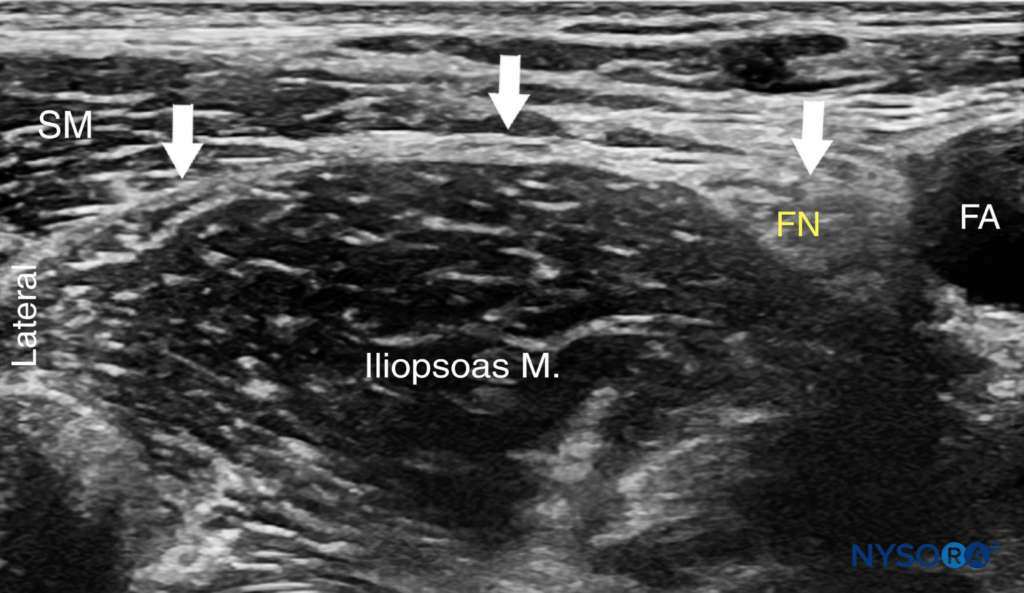
Your ultrasound view should look similar to transverse landmarking for placing a femoral central line or arterial line. The femoral nerve (FN) will be a grape-like cluster just lateral to the femoral artery (use slow sweeps of the probe to find the angle that exaggerates the hyperechogenicity of nerves!).
Using in-plane technique, insert your needle from the lateral and advance until the tip is immediately adjacent to the lateral side of the nerve and initial injection of anesthetic surrounds the nerve. Displacement of the FN or anesthetic filling the planes above and below the nerve confirm your anesthetic placement.
Need a deeper dive? Watch the following video on FN blocks:
Note: Heard of an alternative technique called “3-in-1”? Don’t worry about it… It is essentially a Femoral Nerve block with more volume and subsequent caudal pressure to encourage anesthetic to track proximally. The following Fascia Iliaca block is a much more elegant (and more aptly named) way to achieve proximal coverage.
[bg_faq_end][bg_faq_start]2) Fascia Iliaca Block
This hip nerve block takes advantage of the fact that the fascia iliaca sits directly on top of both the femoral and lateral femoral cutaneous nerves. The goal is to inject local anaesthetic deep to the fascia iliaca with the hopes that it spreads throughout the fascial plane and bathes both the femoral and lateral femoral cutaneous nerves. Historically (before widespread use of ultrasound) this block was achieved by advancing the needle through the femoral crease and feeling for 2 distinct pops as the needle passed through the fascia lata and the fascia iliaca. Under ultrasound guidance you simply identify the fascia iliaca and inject the anaesthetic underneath.
External Landmark
- Femoral crease, distal to the inguinal ligament
Internal Landmark
- The fascia iliaca (FI) covering the psoas muscle and FN, lateral to the femoral artery and nerve (similar to nerves, fascia shines brighter at certain probe angles… slow sweeps will help you find the fascia at its most obvious angle).
Your ultrasound view should look very similar to the femoral nerve approach, but we will be centring the fascia iliaca, lateral to the femoral neurovascular bundle.
The goal will be to introduce the needle laterally at an angle to pierce the fascia iliaca a few centimetres lateral to the FN (approx mid-fascia in the transverse view) and deposit anesthetic immediately beyond the fascia. A large volume of anesthetic should be used (20-40cc) and it should deposit easily between fascia and iliopsoas, and visibly track medially to surround the FN.

Need a deeper dive? Watch the following video on the Fascia Iliaca Block:
3) Pericapsular Nerve Group (PENG) Block
Please note this is a novel technique with emerging evidence. Definitive studies on efficacy and safety have not yet been published. All images in this section are used with permission from the Philip Peng Educational Series.
Derived from anesthesia and anatomy literature, this is another high volume block (ie: use at least 20cc, even if you have to dilute the anesthetic) that bathes the anterior pubic brim, theoretically making it more effective at knocking out the proximal Obturator Nerve (ON) and Accessory Obturator Nerve (AON) while still covering the FN.
External Landmark
- Anterior Superior Iliac Spine (ASIS)
Internal Landmark
- Anterior Inferior Iliac Spine (AIIS), Psoas Tendon, and Iliopubic Eminence (IPE)
- Pro Tip: If you sweep too caudally, the IPE will appear less linear and reveal the femoral head in the acetabulum!
This approach is quite different than the FN block or FI block, as it takes place cephalad to the femoral head. Start by palpating the Anterior Superior Iliac Spine (ASIS) on the patient and then find the ASIS on your ultrasound screen with the probe in transverse axis.

Slide the probe caudal until the Anterior Inferior Iliac Spine (AIIS) comes into view in the far field with the iliacus muscle (IL) laying anterior and medial.

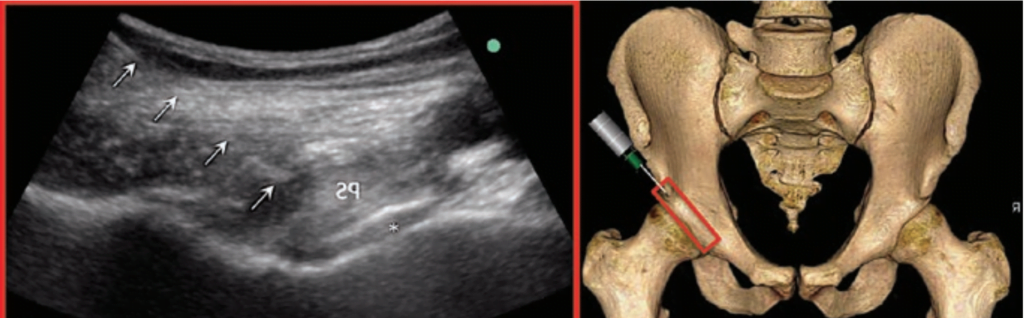
Now rotate the probe ~45 degrees to bring the iliopubic eminence (IPE) in line in the far field. The psoas tendon will appear just anterior to the IPE.
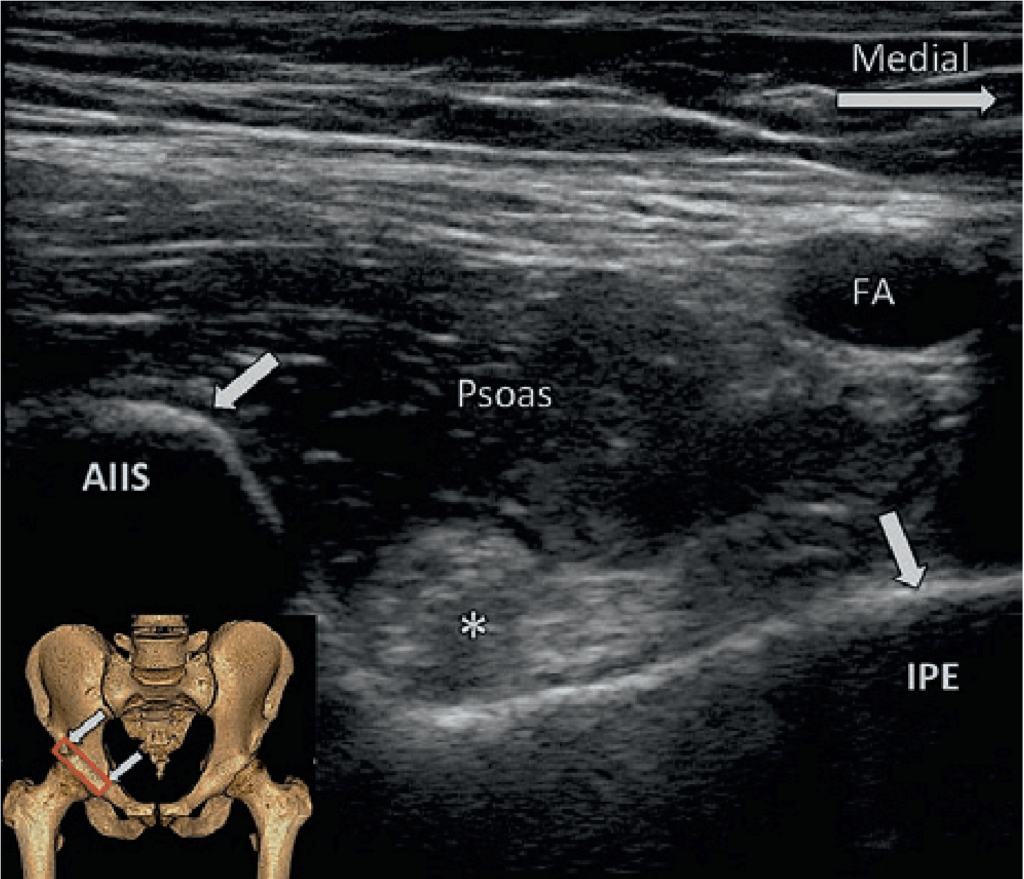
Use a lateral in-plane approach with your needle to get distal to the psoas tendon and dump local anesthetic between the tendon and IPE. It is sometimes described to advance (with the tip in view!) until the needle hits ilium before injecting.
Need a deeper dive? Confused by the new anatomy? We highly recommend watching videos of this and practicing ultrasound view acquisition. Watch the following video on the PENG Block:
Complications
Encountering a complication due to a hip nerve block using these described techniques is thankfully very uncommon. The most frequently reported complications in studies are pain at injection site and hematoma formation.7 Other potential complications include infection, allergic reaction, nerve damage, and inadvertent vascular puncture.6,7 The most feared complication of local anesthetic systemic toxicity (LAST) with neurologic or cardiovascular sequelae is rare. In a recent systematic review of regional nerve blocks of the hip, there were no reported incidences of local anesthetic toxicity in nearly 900 patients who received a regional nerve block for hip fracture.6 CanadiEM’s CrackCast team previously discussed LAST as part of their pain chapter here.
Rapid Evidence Summary
Regional blocks for hip fractures in the preoperative period appear to be at least equivalent to opioid and NSAID analgesia. There is a high rate of success and complications are uncommon.8 Regional nerve blocks for hip fractures are also associated with lower IV opioid usage.9 High quality evidence suggests lower pain scores when patient movement occurs and a lower incidence of pneumonia. There is currently insufficient evidence for reduction in delirium, length of hospital stay and mortality with the use of regional anesthesia for hip fractures compared with other analgesia strategies.10 Overall, the quality of evidence is limited by significant study heterogeneity. Randomized controlled trials are needed for more robust comparison between block techniques and to other analgesia strategies.
- 1.Johnell O, Kanis J. An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int. 2006;17(12):1726-1733. doi:10.1007/s00198-006-0172-4
- 2.Cowan R, Lim J, Ong T, Kumar A, Sahota O. The Challenges of Anaesthesia and Pain Relief in Hip Fracture Care. Drugs Aging. 2017;34(1):1-11. doi:10.1007/s40266-016-0427-5
- 3.Lisk R, Yeong K. Reducing mortality from hip fractures: a systematic quality improvement programme. BMJ Qual Improv Rep. 2014;3(1). doi:10.1136/bmjquality.u205006.w2103
- 4.Birnbaum K, Prescher A, Hessler S, Heller K. The sensory innervation of the hip joint–an anatomical study. Surg Radiol Anat. 1997;19(6):371-375. doi:10.1007/BF01628504
- 5.Nagel E, Gantioque R, Taira T. Utilizing Ultrasound-Guided Femoral Nerve Blocks and Fascia Iliaca Compartment Blocks for Proximal Femur Fractures in the Emergency Department. Adv Emerg Nurs J. 2019;41(2):135-144. doi:10.1097/TME.0000000000000242
- 6.Guay J, Parker M, Griffiths R, Kopp S. Peripheral Nerve Blocks for Hip Fractures: A Cochrane Review. Anesth Analg. 2018;126(5):1695-1704. doi:10.1213/ANE.0000000000002489
- 7.Jeng C, Rosenblatt M. Complications – Overview of peripheral nerve blocks. UpToDate. Published May 13, 2020. Accessed June 1, 2020. https://www.uptodate.com/contents/overview-of-peripheral-nerve-blocks?search=overview%20of%20peripheral%20nerve%20blocks&source=search_result&selectedTitle=1~150&usage_type=default&display_rank=1#H16
- 8.Steenberg J, Møller A. Systematic review of the effects of fascia iliaca compartment block on hip fracture patients before operation. Br J Anaesth. 2018;120(6):1368-1380. doi:10.1016/j.bja.2017.12.042
- 9.Ritcey B, Pageau P, Woo M, Perry J. Regional Nerve Blocks For Hip and Femoral Neck Fractures in the Emergency Department: A Systematic Review. CJEM. 2016;18(1):37-47. doi:10.1017/cem.2015.75
- 10.Guay J, Parker M, Griffiths R, Kopp S. Peripheral nerve blocks for hip fractures. Cochrane Database Syst Rev. 2017;5:CD001159. doi:10.1002/14651858.CD001159.pub2
Expert Review
Pain control is a major part of what we do, and having multiple ways to provide analgesia/anesthesia is critical. This post provides a great introduction to ultrasound-guided regional anesthesia for hip fractures. With multiple ways to perform this block, the first question to ask yourself is where is the fracture. My general rule of thumb is if the fractures is distal to the intertrochanter, then consider performing an isolated femoral nerve block. This works great even for femur shaft fractures and patellar fractures and dislocations. If you are dealing with intertrochanteric fractures and any fracture more proximally, then the 3:1 fascia iliaca block or the PENG block should be your go-to.
From an innervation/anatomic model, the PENG block appears to provide the most sensory innervation coverage to the proximal hip joint, and in theory, should provide superior analgesia. This is yet to be proven clinically, but studies looking at safety and efficacy are pending.
I would also encourage you to work on and optimize your in-plane needle guidance. Most emergency physicians place central or peripheral lines out of plane (meaning you see the vessel in its short axis and only see the tip of the needle). Regional anesthesia calls to master in-plane needle guidance (so you would visualize the entire length of the needle), to optimize the deposition of anesthetic, thus increasing the efficacy of your block. But also critical to avoid violating the epineural sheath, avoiding post block neuropathy and increasing the overall safety of the procedure for the patient.
Remember also that these are large volume blocks, thus it is paramount that you calculate how much local anesthetic your patient can handle before it becomes toxic. If you are mathematically challenged like I am, download the app “Safe Local” to input your anesthetic concentrations and let your phone do the math for you. Consider using bupivacaine, or for an added element of safety, use ropivacaine.











