After a mass casualty incident involving a hotel fire, the Seattle Grace Hospital was in chaos. As in every episode, the emergency department was run entirely by surgeons. Patients were handed off between residents with little communication as they ran from one case to the next and additional casualties were wheeled in. Ultimately, one crucial mistake during the assessment of patient C. Becker led to her demise.
Mrs. Becker was a 30-year-old female brought to the ED by ambulance from the hotel fire. It was unknown how long she was exposed for, but she stated she and her son were out quicker than the others because they were on the first floor. On initial assessment, she was alert and oriented, in no acute distress, and breathing comfortably with stable vitals. There was no hoarseness to her voice, and on examination of the chest, there was equal air entry bilaterally with no adventitious sounds. She had a burn over her left anterior shoulder and chest that was soft, erythematous, blistering, blanched with pressure, and was intensely painful to pinprick testing. She also had a burn on her left anterior shin that appeared deeper, stiff, waxy, white, and was non-blanchable with no sensitivity to pinprick.
For the burn on her shin, plastic surgeon (Dr. Mark Sloan, also known as McSteamy) was consulted to debride the wound and coat it in silver sulfadiazine. Her wounds were dressed, and the patient was left unattended while awaiting morphine for her pain. At some point, she took a turn for the worst and was found in her bed in acute respiratory distress. A series of attempts to resuscitate her ensued, including an unsuccessful intubation and cricothyrotomy (notably, this was the 2nd cricothyrotomy performed by a resident in the past five years; an anomaly given their rarity). Eventually, the patient suffered from ARDS, DIC, ventricular fibrillation, and cardiac arrest secondary to their injuries.
So what went wrong in Mrs. Becker’s case, what can we learn from this oh-so-dramatic episode, and how can you avoid a cricothyrotomy, a bad outcome, and a resident being fired for missing a crucial step in your patient’s assessment?
Overview
Let’s start with a brief review. Burns are thermal, chemical or electrical insults causing damage to the skin and underlying tissues.1 Management starts with the usual ABC’s, discussed in more detail below, followed by a secondary survey that includes determining the percentage of the patient’s Total Body Surface Area (TBSA) that has been burned and assessment for other injuries. Treatment including the provision of adjusted fluid rates (outlined in the circulation section below) and wound care should also be provided.1 General guidelines for burns management follow Advanced Trauma Life Support (ATLS) and Advanced Burns Life Support (ABLS).
The skin has three main layers: the thinner epidermis, the thicker underlying dermis and the subcutaneous layers.2 The four main functions of the skin1 relate to some of the serious consequences of a burn.
- Protects from infection and injury (sepsis)
- Prevents body fluid loss (hypovolemia)
- Regulates body temperature (hypothermia)
- Environmental interaction via sensory receptors
Classifying burns
Burns should be classified by depth and size (% total body surface area), as each will affect prognosis and management.2
Estimating burn depth
Burn depth is typically estimated clinically, though this is only 50-75% accurate.2 Laser Doppler imaging is a more advanced technique shown to increase the accuracy of burn depth assessment by about 15% on the same day as the burn occurs, though its use is mostly limited to burn centres and research.3
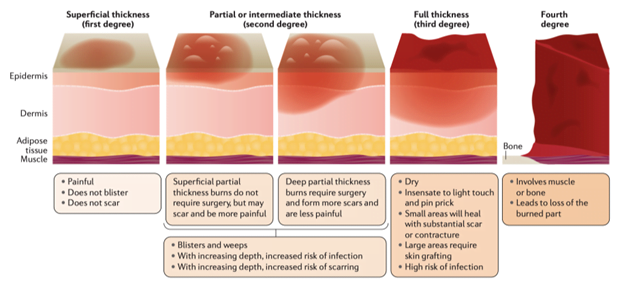
Burns are classified by the degree of involvement of the dermis: 1st degree (no involvement), 2nd degree (partial involvement), or 3rd degree (complete involvement) (Figure 1).4 Burns involving underlying tissues such as muscle or bone are considered 4th degree.
Estimating burn depth: physical examination
The physical exam maneuvers that may help assess burn depth include assessing the color, presence or absence of blisters, skin pliability, capillary refill, and sensation (to touch or needle prick) (Table 1).2
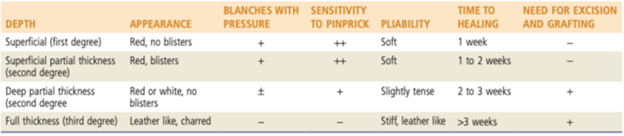
In Mrs. Becker’s case, based on the physical examination, the burn over her left anterior shoulder and chest would be most consistent with a partial thickness 2nd degree burn(soft, erythematous, blistering, blanches to pressure and sensitive to pinprick) and the burn on her left anterior shin is most consistent with a 3rd degree burn (stiff, waxy, white, does not blanch, no sensitivity to pinprick).


Estimating body surface area
Similar to depth, the affected body surface area should be estimated to guide prognosis and fluid resuscitation. Notably, when estimating burn area only areas impacted by at least a 2nd degree burn should be included.2
The two most common methods for estimation are the Wallace’s Rule of Nines and the Lund & Browder chart.5 While the Rule of Nine’s may be slightly easier to use, it is less accurate in morbidly obese patients6 and children.7 However, the Lund & Browder chart does have pediatric adjustments and is thus the chart of choice for pediatrics. Alternatively, smaller burns may be estimated in comparison to the size of the patient’s palm, which represents roughly 1% of body surface area.2
In either case, it is important to recognize that providers tend to overestimate burn size.2 This can lead to inappropriate transfer to burn centres and over-administration of IV fluids leading to compartment syndrome and/or ARDS.2

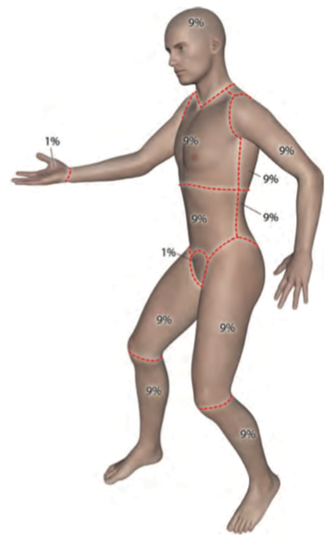
The burns over Mrs. Becker’s chest and leg represent approximately 3% and 2% of body surface area respectively, for a TBSA of 5%.
Airway & Breathing
Airway assessment and consideration of early intubation is paramount in burn patients because inhalation injuries can cause delayed airway edema. In Mrs. Becker’s case, this ultimately led to her demise. The resident saw that her vitals were normal, lung sounds were clear, and just as she was about to ask Mrs. Becker to open up to visually assess for soot or particulate in the airway, a patient with an axe injury to the chest was being wheeled in to the ED causing her to become distracted and forget to check. This may be a rare instance where a dramatic medical TV episode actually portrays a useful real-life lesson: while it is a bit far-fetched that the rest of her physical exam was completely normal, anything can happen and a thorough assessment is always best, as smoke inhalation patients can decompensate quickly.
There are three types of inhalation injury: thermal injury (to the mouth, oropharynx or larynx), lung parenchymal injury (due to inhaled particulates or chemicals seeding more deeply into the lungs), and metabolic asphyxiation (most commonly due to carbon monoxide or hydrogen cyanide).9
Identifying possible inhalation injuries
Not every burn patient will have an inhalation injury – so how do we identify those at higher risk? Rosen’s Emergency Medicine offers facial burns, hoarseness, drooling, carbonaceous sputum, and singed nasal hairs as indicators for a possible inhalation injury.2 One study of 1148 patients in Australia, mostly with <10% TBSA burned, had an 11% prevalence of inhalation injuries.10 Risk factors in this study for inhalation injury included historical features (involvement of a flame, being in an enclosed space, dyspnea) and physical examination findings (higher %TBSA, hoarse voice, facial burns, and having soot in the mouth).10 In Mrs. Becker’s case, while her case initially appeared relatively benign and it was thus surprising for her to deteriorate, she did have at least two of these risk factors (flame, enclosed space). Alas, we will never know if she had soot in her mouth.
Indications for intubation
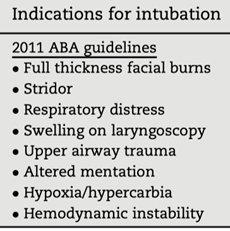
Deciding which patients require intubation is difficult and there are no agreed upon criteria; however, when in doubt, early or even prophylactic intubation is traditionally generally encouraged.2 Nonetheless, intubation is not a risk-free procedure11, and there are documented adverse effects of aggressive intubation in burn patients.12 A recent retrospective study attempted to define appropriate criteria for intubation in thermal burn patients, and described the “Denver criteria”, which added singed facial hair and suspected smoke inhalation to the already-existing American Burn Association (ABA) criteria (Figure 4), increasing the sensitivity to 95% (though lowering the specificity from 46% to 24%) for predicting patients who would require long-term intubation (≥2 days in the 28d period).13 Overall, employing the Denver criteria would result in very few patients who require intubation being missed, but many patients would be needlessly intubated.

Breathing
Of the three types of inhalational injury described above, lung parenchymal injury and metabolic asphyxia are most relevant in the assessment and management of breathing, and should have been evaluated in Mrs. Becker’s case. Patients with suspected inhalation injury should receive supplemental humidified O2 to achieve saturations >92%, in addition to mechanical ventilation if this cannot be achieved.2 100% FIO2 should be given to patients with suspicion of CO poisoning. Inhaled beta-agonists may also be employed to reverse airway bronchoconstriction.2 To assess for metabolic asphyxia, CO levels and cyanide toxicity should be monitored.
Circulation
Burns increase vascular permeability which leads to “third spacing”, low effective circulating volume, and hypotension.4 The goal of fluid resuscitation in burn patients is to provide enough fluid to perfuse the organs and prevent shock, while at the same time avoiding complications of over-resuscitation such as compartment syndromes (extremity, abdominal or orbital) and pulmonary or cerebral edema.1,4 Fluid resuscitation is generally required for adults with burns >20% BSA and children with burns >10% BSA.2 Therefore, in Mrs. Becker’s case of a 5% BSA burn, no fluid resuscitation was required.
Conversely, on the same episode another patien, Evan Lang, a 20-year-old 68kg male, presented with 2nd and 3rd degree burns over 20% TBSA:

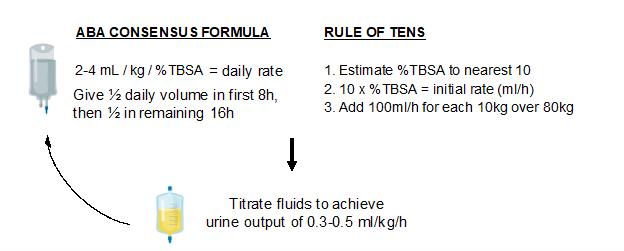
For patients like Mr. Lang who require fluid resuscitation, 2 large-bore IVs should be inserted. A balanced crystalloid solution, such a Ringer’s Lactate, is most commonly used.1 Then, the initial fluid infusion rate should be calculated.4 Assessing the initial infusion rate depends on the %TBSA burned (Figure 5). Historically, the Parkland formula was the preferred method (4mL/kg/%TBSA = total amount of crystalloid to deliver in first 24h), though this has fallen out of favour as it may lead to complications of over-resuscitation described above (compartment syndromes, pulmonary edema etc.).14 The current recommendation from the ABA is to target 2-4mL/kg/%TBSA burned.4 Alternatively, the Rule of Tens was recently described as a simple method for estimating initial infusion rates: 1) estimate the %TBSA to the nearest 10; 2) multiply that by 10 to get your initial infusion rate in ml//h; 3) for every 10kg bodyweight above 80kg, add 100ml/h.15
Importantly, after your initial resuscitation, you should no longer rely on a formula to guide fluid administration. Following your initial resuscitation, fluid rates should then be titrated to achieve a target urine output of 0.3-0.5 ml/kg/hr.4 Based on Mr. Lang’s case, his starting rate would be 2-4 ml x 68kg x 20%TBSA = 2720 – 5440 ml/d (by the ABA formula), of which half of this amount will be given within the first 8h = 1360 – 2720 ml/8h or 170 – 340 ml/h as an initial fluid rate. Alternatively using the Rule of Tens, 20% TBSA x 10 = 200ml/h is the initial fluid rate. Regardless of which formula is initially used for fluid resuscitation, the calculated rate should be abandoned and instead titrated to achieve a urine output of 0.5 mg/kg/hour in adults.4
Local wound care
Burns should be covered with a clean dressing to minimize pain and further trauma during transport.2 For partial thickness burns, as on Mrs. Becker’s chest, management is primarily topical antibiotics (preferably ointments or impregnated dressings, though creams or liquids are okay) and absorptive, nonadherent dressings.2 Most dressing protocols involve silver as the antimicrobial, as it has antimicrobial properties.4
In this episode, Mrs. Becker is treated with topical silver sulfadiazine, but this is actually no longer recommended except for heavily contaminated or infected burns (notably, the episode as shot in 2009).2 Nonetheless, there is no clear evidence favouring any particular topical antimicrobial and/or dressing regimen over another, and choice is often made on availability or regional practice.4
Whether or not blisters should be ruptured is a topic of debate with insufficient comparative trials to give a clear answer. A review of the topic suggests favouring rupture of blisters that are larger (>6mm, as they are likely to rupture on their own or thin-walled (thicker blisters on the palms and soles may be left intact).16 Early surgical debridement and excision is the definitive treatment for burns deeper than superficial 2nd degree, though it is unclear whether this should be done within the first 24h or after 2-3 days of stabilization.4 A 14-year single centre analysis of 3561 patients that those who had surgical intervention on an average of day 6 as opposed to day 15 had had shorter hospital stays of 14 days relative to 23 days17 suggesting delayed debridement may be more appropriate.
Case resolution
Unfortunately, Mrs. Becker succumbed to her injuries. This case illustrates the importance of recognizing inhalational injury and acting rapidly in patients with an impending loss of airway. Applying the Denver criteria to Mrs. Becker’s initial assessment, she did not meet 6 of the 8 criteria for intubation: she did not have facial burns, stridor, respiratory distress, upper airway trauma, altered mentation, hypoxia or hemodynamic instability. Despite Chief Weber being certain that if Dr. Kepner had “looked in her throat”, she would have seen soot, we do not know if Mrs. Becker met either of the other 2 criteria (swelling on laryngoscopy or upper airway trauma). Ultimately, one should maintain a low index of suspicion for possible inhalation injury and remember the ABCs. Dr. Kepner was fired because of this case but rehired in a later episode when Dr. Derek Shepherd (also known as Dr. McDreamy) takes over as Chief.
Take home points
- Primary survey first! Remember the risk factors for inhalation injury (involvement of a flame, being in an enclosed space, dyspnea, higher %TBSA, hoarse voice, facial burns, and having soot in the mouth), and consider intubation early.
- Secondary survey: estimate burn depth and TBSA (Lund and Browder chart, Rule of Nines, palm size for small burns, or your institution’s preferred method).
- For adults with TBSA >20%, or children >10%, fluid resuscitate using the ABA consensus formula or Rule of Tens, then titrate to urine output.
- Treat locally with a topical antimicrobial agent and an absorptive, nonadherent dressing. Refer for surgery if the burns are deep partial thickness or deeper.
References
- 1.Advanced Burn Life Support: Provider Manual 2018 Update. American Burn Association; 2018.
- 2.Walls R, Hockberger R, Gausche-Hill M. Rosen’s Emergency Medicine: Concepts and Clinical Practice. 9th ed. Elsevier; 2018.
- 3.Hoeksema H, Van de, Tondu T, et al. Accuracy of early burn depth assessment by laser Doppler imaging on different days post burn. Burns. 2009;35(1):36-45. doi:10.1016/j.burns.2008.08.011
- 4.Jeschke M, van B, Choudhry M, Chung K, Gibran N, Logsetty S. Burn injury. Nat Rev Dis Primers. 2020;6(1):11. doi:10.1038/s41572-020-0145-5
- 5.Miller S, Finley R, Waltman M, Lincks J. Burn size estimate reliability: a study. J Burn Care Rehabil. 1991;12(6):546-559. doi:10.1097/00004630-199111000-00010
- 6.Williams R, Wohlgemuth S. Does the “rule of nines” apply to morbidly obese burn victims? J Burn Care Res. 2013;34(4):447-452. doi:10.1097/BCR.0b013e31827217bd
- 7.Chan Q, Barzi F, Cheney L, Harvey J, Holland A. Burn size estimation in children: still a problem. Emerg Med Australas. 2012;24(2):181-186. doi:10.1111/j.1742-6723.2011.01511.x
- 8.Minimas D. A critical evaluation of the Lund and Browder chart. Wounds UK. Published online 2007.
- 9.Cancio L. Airway management and smoke inhalation injury in the burn patient. Clin Plast Surg. 2009;36(4):555-567. doi:10.1016/j.cps.2009.05.013
- 10.Dyson K, Baker P, Garcia N, et al. To intubate or not to intubate? Predictors of inhalation injury in burn-injured patients before arrival at the burn centre. Emerg Med Australas. Published online August 27, 2020. doi:10.1111/1742-6723.13604
- 11.Cook T, MacDougall-Davis S. Complications and failure of airway management. Br J Anaesth. 2012;109 Suppl 1:i68-i85. doi:10.1093/bja/aes393
- 12.Duek O, Ben N, Bar-Lavie Y, Bahouth H, Ullmann Y. Pneumonia Risk in Urgently Intubated Burn Patients. Isr Med Assoc J. 2018;20(12):737-740. https://www.ncbi.nlm.nih.gov/pubmed/30550001
- 13.Badulak J, Schurr M, Sauaia A, Ivashchenko A, Peltz E. Defining the criteria for intubation of the patient with thermal burns. Burns. 2018;44(3):531-538. doi:10.1016/j.burns.2018.02.016
- 14.Blumetti J, Hunt J, Arnoldo B, Parks J, Purdue G. The Parkland formula under fire: is the criticism justified? J Burn Care Res. 2008;29(1):180-186. doi:10.1097/BCR.0b013e31815f5a62
- 15.Chung K, Salinas J, Renz E, et al. Simple derivation of the initial fluid rate for the resuscitation of severely burned adult combat casualties: in silico validation of the rule of 10. J Trauma. 2010;69 Suppl 1:S49-54. doi:10.1097/TA.0b013e3181e425f1
- 16.Sargent R. Management of blisters in the partial-thickness burn: an integrative research review. J Burn Care Res. 2006;27(1):66-81. doi:10.1097/01.bcr.0000191961.95907.b1
- 17.Munster A, Smith-Meek M, Sharkey P. The effect of early surgical intervention on mortality and cost-effectiveness in burn care, 1978-91. Burns. 1994;20(1):61-64. doi:10.1016/0305-4179(94)90109-0
This post was copy-edited by @alexsenger.



