
Our patient for today’s case is Kang Sae-byeok, also known as Player 067. A North Korean defector struggling to make ends meet as a pickpocket in Seoul, Sae-byeok accepts an invitation to compete in the mysterious “Squid Game” for the chance to win millions of won and improve the lives of her and her family. She eventually comes to learn that the Squid Game competition pits hundreds of participants against one another in a series of childhood games with only two outcomes: win or die. Sae-byeok’s sharp cunning and street smarts allow her to survive the first five games without harm. Almost immediately after winning the fifth game, however, a large shard of glass from an exploding glass bridge causes a penetrating lower abdominal injury.
Observations
On exam, a penetrating anterior abdominal wound to the left suprapubic region is noted with an approximate 10 cm by 3 cm penetrating glass shard in situ. While difficult to assess, the wound width is estimated at approximately 3 cm with an unknown depth. A large amount of dried and fresh blood was seen surrounding the wound, but an accurate quantitative assessment could not be obtained. Approximately 30 minutes after her injury, the patient self-extracted the penetrating implement and loosely dressed the area with an article of clothing. Post-extraction blood loss was difficult to quantify. Local wound exploration was not performed, and it is unclear if any penetrating shrapnel remained in situ. The patient was fully alert throughout but appeared moderately pale and significantly weakened. No further examination was performed.

Discussion
In the minutes following the explosion, Player 067 attempts to tend to her injuries in private. Her efforts are in vain, however, as competing Player 218 eventually notices her vulnerability and slits her throat as she lies weakened in her bed, leading to immediate hemorrhage, airway compromise, and death. While Player 218’s actions are not condoned by the author, Player 067 would have likely decompensated into hemorrhagic shock from her penetrating abdominal wound within in a matter of hours, particularly with the Squid Game administration’s unsurprising lack of interest in resuscitating acutely unwell participants. Her decision to self-extract the penetrating shard would have likely hastened this decompensation due to loss of a possible tamponading effect from the shard.1 Even if she had been able to avoid life-threatening hemorrhage, she would have eventually succumbed to infection in the absence of appropriate antibiotic coverage.2

Characterizing Abdominal Trauma
When it comes to approaching abdominal trauma, it helps to have an anatomical framework. Along with our traditional four-quadrant system, traumatic abdominal injuries are more broadly characterized into four main regions based on their relative risk of intra-abdominal injury. Penetrating abdominal injuries should generally be considered with any injury below the nipple line anteriorly and inferior scapula posteriorly, based on the location of the diaphragm at end-expiration through injuries close to this region should be assumed to occur in both abdomen and chest.

| Region of Injury | Complications |
|---|---|
| Thoracoabdominal | **Risk of intra-abdominal (IA), mediastinal, and thoracic injuries4 |
| Anterior abdomen | *44% risk of IA injury5 |
| Flank | *29% risk of IA injury5 |
| Back | *15% risk of IA injury5 |
**Lower incidence of diaphragmatic injury with right-sided thoracoabdominal penetrating wounds due to protection from liver
Initial Approach to Abdominal Trauma
Along with location, abdominal trauma should be characterized into penetrating versus blunt injury. Penetrating abdominal injuries can further be separated into low velocity (e.g., knife, scissors) and medium to high velocity (e.g., gunshot, explosion).6 Regardless of the mechanism or velocity, the goal of diagnostic evaluation is to answer two main questions6:
- Was there peritoneal violation?
- Is there intra-abdominal injury?
Although the answer to these questions is typically obvious in unstable patients, they can be more challenging to identify in the stable patient. For most patients with blunt and/or penetrating abdominal trauma, physical examination plus E-FAST (FAST + bilateral lung views), often followed by contrast-enhanced CT, tends to be the diagnostic pathway of choice.6 For the stable patients with negative or equivocal imaging findings, further diagnostics typically involve a combination of local wound exploration and serial examinations.
For unstable patients, diagnostic work up should not delay emergent surgical management. Indications for emergent OR (typically laparotomy) in abdominal trauma include hemodynamic compromise, peritoneal signs, evisceration, or left sided diaphragmatic injury. Relative indications include GI hemorrhage (hematemesis and/or hematochezia), implement in situ, and intraperitoneal air.6
This leads to a critical question and the main topic of today’s discussion: How can we, as ED providers, temporize the patients who are unstable or who have arrested due to hemorrhage while they await definitive surgical management?
Resuscitative Endovascular Balloon Occlusion of the Aorta (REBOA)
Traditionally, resuscitative thoracotomy (RT) with aortic cross-clamping has been the intervention of choice for achieving control of non-compressible torso hemorrhage (NCTH) for patients in extremis (i.e., severe hemodynamic compromise). This is, of course, a temporizing measure until definitive surgical management can be obtained.4 Despite what the writers of Grey’s Anatomy or ER want us to think, survival rates following ED thoracotomy for penetrating abdominal trauma are somewhat disheartening (around 9% based on 25 years of data from 2000).7
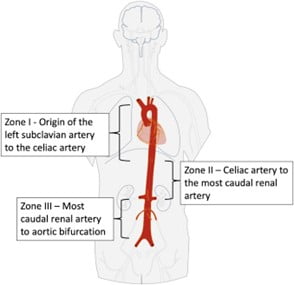
In more recent literature, resuscitative endovascular balloon occlusion of the aorta (REBOA – not to be confused with country music sensation, Reba) has been suggested as an alternative to RT for achieving NCTH control for life-threatening bleeds.8 As the name suggests, REBOA involves deploying an occluding balloon in the distal thoracic or distal abdominal aorta (depending on the site of injury), typically via the femoral artery, to gain hemorrhage control and thus improve proximal perfusion to the brain and coronaries.9
Although similar techniques are long-familiar to vascular surgeons for non-resuscitative purposes, balloon occlusion of the aorta for hemorrhage control is less well-established in the trauma literature.8
First described by military surgeons during the Korean War in the 1950s, REBOA has continued to play an important role in military trauma since then.10 For civilian trauma, however, REBOA has remained in relative obscurity up until a rather dramatic resurgence in popularity over the past few years.8
In the setting of abdominal trauma, both RT and REBOA are based on the same principle: occlude the aorta and you’ll stop the downstream bleeding. Where REBOA shines is in how much less invasive it is than RT. No longer must you boldly crack open the chest of your crashing patient and massage their dying heart back to life, much to the chagrin of TV medical drama writers across the globe. By utilizing familiar skills such as arterial line placement and the Seldinger technique, REBOA can be safely and efficiently performed by emergency and critical care physicians (although it does still require specialized training).9 Not only does this make it less invasive and more efficient than RT, but it can also be performed without interrupting ATLS protocols and other critical interventions.
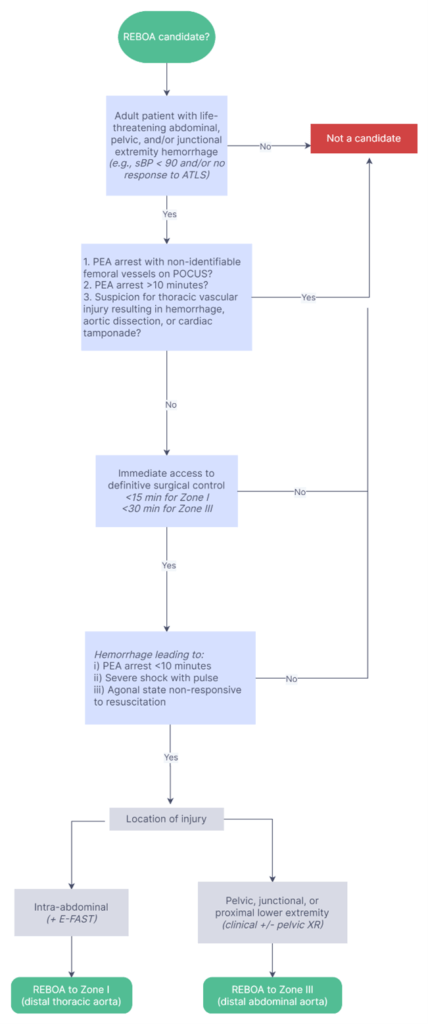
When it comes to abdominal trauma, both REBOA and RT are indicated to temporize noncompressible subdiaphragmatic hemorrhage. In its simplest form, this means hypotensive trauma patients with clear or suspected intra-abdominal hemorrhage (typically identified with a positive E-FAST, with the caveat that pelvic and junctional limb hemorrhage may have a negative E-FAST). The major difference is that only RT is indicated for thoracic vascular injuries such as cardiac injuries and cardiac tamponade, as it allows for manual decompression of the pericardium and manipulation of the heart.8,9 Not only is REBOA unable to address thoracic vascular injuries, it is actually contraindicated in these scenarios given its risk of exacerbating any hemorrhage proximal to the balloon occlusion point. Conversely, REBOA is contraindicated for these proximal injuries, given its risk of exacerbating existing vascular injuries that lie proximal to the balloon occlusion point9
While civilian trauma REBOA research is still in its infancy, most studies suggest a significant survival advantage when compared to open aortic occlusion (via RT) and a less clear benefit compared to non-REBOA controls.11–13 Most recently, a 2022 meta-analysis comprised of 8 studies and 3241 patients found a significant mortality benefit and shorter length of ICU stay with REBOA compared to RT, while there was no significant difference length of hospital stay.11 Similarly, a 2021 meta-analysis (11 studies, n = 5866) found a significant mortality benefit for REBOA versus RT but no significant benefit for REBOA compared to no REBOA.12 The caveat is that most of the current REBOA data is based on low to very low quality evidence, comprised of retrospective data and highly variable population characteristics. 9,11–13 The absence of high-grade evidence has led to uncertainty surrounding the specific indications for REBOA, meaning that current recommendations are largely based on expert consensus.8,10 In general, the main indication for REBOA is subdiaphragmatic abdominal, pelvic, or junctional extremity hemorrhage (without concurrent thoracic trauma) that is unresponsive or transiently responsive to resuscitation.8 While there is no evidence to suggest an optimal “trauma to balloon” time for REBOA, it should be implemented within the same window as would RT and should be avoided for PEA arrest greater than 10 minutes.8,9 These criteria are summed up in the algorithm below.
How do we perform REBOA?
When it comes to performing REBOA, the technique can be broken down into five sequential steps: arterial access and sheath positioning, balloon selection and positioning, balloon inflation, balloon deflation (and definitive management), and sheath removal.10 The aorta zone classification system (pictured below) is used to determine where best to inflate the balloon.
| Site of Injury | Site of REBOA placement9,12 (External landmark) |
|---|---|
| Sub-diaphragmatic abdomen | Zone I (mid-sternum to xiphoid) |
| Pelvic and/or junctional extremity | Zone III (umbilicus) |
A video demonstrating this technique with the ER-REBOA catheter system can be viewed here: ER-REBOA™ Procedure – YouTube
What are the complications of REBOA?
No procedure is without complication, and REBOA is no exception. While complications directly related to the use of REBOA tend to be infrequent, they can lead to serious harms.13 In general, complications can be classified into local vascular (e.g., local arterial dissection or embolization), distant vascular (e.g., ischemia), and non-vascular (e.g., reperfusion injuries).9 Of these, local vascular injuries, embolization (air, thrombus, or foreign material), and ischemia are the most common. Fortunately, many of these can be mitigated with appropriate patient selection and proper REBOA technique.9
Outcome and Conclusion
Unfortunately, the Squid Game facilities lacked an established REBOA program (or any trauma service whatsoever) at the time of Player 067’s death. Moreover, her rapid demise secondary to a penetrating neck wound at the hands of Player 218 would have terminated any further resuscitative efforts. While we would like to think her death was not in vain, the Squid Game administrators are unlikely to implement a REBOA program in the future given their obvious conflict of interest of killing their participants for sport. Thankfully, the same can not be said for Canadian Level 1 and 2 trauma centres, one in five of which have implemented REBOA programs as of mid-202114 – a number that is all but certain to climb alongside a rapidly growing body of REBOA research. Ultimately, this rising presence will allow for the collection of better data that provides richer insights into the effectiveness of REBOA in these settings. In the end, it is hoped that such insights might lead to meaningful improvements in patient outcomes, perhaps allowing us to spare future patients with a fate reminiscent of Player 067.
References
- 1.Kong V, Khan Z, Cacala S, Oosthuizen G, Clarke D. Retained weapon injuries: experience from a civilian metropolitan trauma service in South Africa. Eur J Trauma Emerg Surg. Published online May 1, 2014:161-166. doi:10.1007/s00068-014-0405-8
- 2.Morales CH. Intra-abdominal Infection in Patients With Abdominal Trauma. Arch Surg. Published online December 1, 2004:1278. doi:10.1001/archsurg.139.12.1278
- 3.Chalwell L. Penetrating Abdominal Trauma. In: CorePendium. CorePendium, LLC; 2022:6. Accessed April 13, 2022. https://www.emrap.org/corependium/chapter/recx0KCu5EgXdkwzB/Penetrating-Abdominal-Trauma#h.ekd19x4bq51
- 4.Legome E, Shockley LW, eds. Trauma: A Comprehensive Emergency Medicine Approach. Cambridge University Press; 2011.
- 5.McCarthy MC. Prediction of Injury Caused by Penetrating Wounds to the Abdomen, Flank, and Back. Arch Surg. Published online August 1, 1991:962. doi:10.1001/archsurg.1991.01410320044004
- 6.Tintinalli J. Tintinalli’s Emergency Medicine: A Comprehensive Study Guide. 9th ed. McGraw Hill; 2022. Accessed April 11, 2022. https://accessemergencymedicine.mhmedical.com/content.aspx?bookid=2353§ionid=183421313
- 7.Rhee P, Acosta J, Bridgeman A, Wang D, Jordan M, Rich N. Survival after emergency department thoracotomy: review of published data from the past 25 years. J Am Coll Surg. 2000;190(3):288-298. doi:10.1016/s1072-7515(99)00233-1
- 8.Bulger EM, Perina DG, Qasim Z, et al. Clinical use of resuscitative endovascular balloon occlusion of the aorta (REBOA) in civilian trauma systems in the USA, 2019: a joint statement from the American College of Surgeons Committee on Trauma, the American College of Emergency Physicians, the National Association of Emergency Medical Services Physicians and the National Association of Emergency Medical Technicians. Trauma Surg Acute Care Open. Published online September 2019:e000376. doi:10.1136/tsaco-2019-000376
- 9.Long B, Hafen L, Koyfman A, Gottlieb M. Resuscitative Endovascular Balloon Occlusion of the Aorta: A Review for Emergency Clinicians. The Journal of Emergency Medicine. Published online June 2019:687-697. doi:10.1016/j.jemermed.2019.03.030
- 10.Cannon J, Morrison J, Lauer C, et al. Resuscitative Endovascular Balloon Occlusion of the Aorta (REBOA) for Hemorrhagic Shock. Military Medicine. Published online September 1, 2018:55-59. doi:10.1093/milmed/usy143
- 11.Khalid S, Khatri M, Siddiqui MS, Ahmed J. Resuscitative Endovascular Balloon Occlusion of Aorta Versus Aortic Cross-Clamping by Thoracotomy for Noncompressible Torso Hemorrhage: A Meta-Analysis. Journal of Surgical Research. Published online February 2022:252-260. doi:10.1016/j.jss.2021.09.016
- 12.Castellini G, Gianola S, Biffi A, et al. Resuscitative endovascular balloon occlusion of the aorta (REBOA) in patients with major trauma and uncontrolled haemorrhagic shock: a systematic review with meta-analysis. World J Emerg Surg. Published online August 12, 2021. doi:10.1186/s13017-021-00386-9
- 13.Kinslow K, Shepherd A, McKenney M, Elkbuli A. Resuscitative Endovascular Balloon Occlusion of Aorta: A Systematic Review. Am Surg. 2022;88(2):289-296. doi:10.1177/0003134820972985
- 14.Hurley S, Erdogan M, Lampron J, Green RS. A survey of resuscitative endovascular balloon occlusion of the aorta (REBOA) program implementation in Canadian trauma centres. Can J Emerg Med. Published online September 18, 2021:797-801. doi:10.1007/s43678-021-00193-w



