FRCPC or CCFP-EM?
This is a question that EM physicians spend a lot of time discussing with their mentees. Why are there two EM designations in Canada? What do the letters even mean? What’s the difference? Which route is right for you?
These are great questions. Unfortunately, as with many important decisions, you’ll probably get as many answers to them as people you ask. Everyone in the Canadian EM world seems to have an opinion on this topic, and today I am going to share mine. “Why would you want to get into this potentially thorny topic?” you may ask?
Two reasons: First, I think it is important for medical students to make an educated decision. The only way to do that is by hearing a lot of opinions and deciding what is best for their personal situation and career goals. And second, because I feel like I have a pretty good idea of the range of responses.
There are a lot of things in my background that has coloured my thoughts on this issue. The most obvious of these is that I chose the FRCPC (Fellow of the Royal College of Physicians of Canada) route. My opinion has also been shaped by training in Saskatchewan, where a significant portion of my training came from CCFP-EM (Canadian College of Family Physicians – Emergency Medicine) physicians (there were no FRCPC EM physicians in the province when I started medical school and only two when I started residency). Finally, I have been quite involved in Canadian EM over the past decade. As a resident, I was the president of the CAEP resident section and sat on the CAEP board through the tail end of its discussions about the Montreal Task Force (aka Dual College/Dual Certification (DC/DC)) on Canadian EM credentials. As faculty, I have spent a year as a program director and helped to design the FRCPC Competence By Design assessment program. I learned a lot about the historical context of this issue in these roles.
Why are there two EM designations in Canada?
While it was certainly discussed earlier, the first mentions I found in the literature of EM training paths came in 1997. Drs. James Ducharme and Grant Innes started some controversy that year with an editorial in a CAEP Communique published in the Fall of 1997 titled “The FRCPC vs the CCFP(EM): Is there a difference 10 years after residency?” This article and a history of publications and letters to the editor that address this issue were compiled by CAEP in a suite containing multiple documents relevant to the history of Canadian emergency medicine. In this particular article, Drs. Ducharme and Innes provide their take on how the two streams of training came to be. As I was -4 years old back in 1980 when the two programs were conceived, I take their word for it. Here it is:
Almost 20 years ago [now >40 years ago], two groups perceived the importance of emergency medicine (EM) and saw the need for advanced EM training. The Royal College of Physicians and Surgeons viewed emergency medicine as a new specialty with a distinct body of expertise, while the College of Family Physicians viewed it as a critical aspect of primary care. As a result of disparate philosophies and divergent political agendas, 2 distinctly different training programs for EM arose and flourished in Canada.
Their editorial went on to speculate about the differences (or lack of differences) between the graduates of the two training streams. If the letters to the editor published in response were representative, it raised quite a furor. Some CCFP-EM physicians took offense from their conclusion that the FRCPC program was intended to provide “proper academic training” that would allow its residents to provide “academic leadership” to EM and that a CCFP-EM program “could not possibly teach” that in one year.
Over the subsequent decades, the situation has not changed significantly. There are still two training programs, every once in a while someone proposes modifying/unifying them in some way, and every time their efforts are rebuffed. Most recently, CAEP reviewed emergency physician credentialing in Canada through a Working Group in 2013 – their conclusions were published in 2016 and can be read here. No substantive changes were forthcoming.
What’s the Difference?
The first thing to compare about the programs is their goals so that their purpose can be understood.
The goals of Certification in Family Medicine with added competency in Emergency Medicine program that leads to the CCFP-EM credential as described in a historical version of the CFPC’s Red Book (the current version is much less explicit) are:
1. To improve the standards and availability of emergency care from practicing family physicians
2. To establish guidelines for the development and administration of training programs in emergency medicine for family physicians
3. To ensure the availability of teachers for training programs in family medicine/emergency medicine
They describe CCFP(EM) graduates as follows:
The family physician/emergency physician is a family physician who acquires additional skills in emergency medicine to augment family medicine training. The goal of this training is to prepare family physicians to integrate the principles of family medicine into their emergency practice.
Conversely, from the Royal College’s Royal College Objectives of Training:
Upon completion of training, a resident is expected to be a competent specialist in Emergency Medicine, capable of assuming a consultant’s role in the specialty. The resident must acquire a working knowledge of the theoretical basis of the specialty, including its foundations in the basic medical sciences and research.
The specialist Emergency physician employs pertinent methods of prioritization, assessment, intervention, resuscitation, and further management of patients to the point of transfer. Appropriate procedural and pharmacotherapeutic interventions are central to these abilities.
The specialist Emergency physician possesses organizational skills in emergency department management and disaster management, and the ability to interface with and play a leadership role in the development and organization of emergency medical services and prehospital care.
Residents must demonstrate the requisite knowledge, skills and attitudes for effective patient-centered care and service to a diverse population. In all aspects of specialist practice, the graduate must be able to address ethical issues and issues of age, gender, sexual orientation, culture, and ethnicity in a professional manner. The specialist Emergency physician has the ability to incorporate these perspectives in research methodology, data presentation, and analysis.
I think it is important for a medical student considering which route to EM practice they would like to take to compare their career goals to the goals of the program that will train them. Which description sounds like it is more for you?
In terms of what is included in the training, we have outlined the requirements of the CCFP-EM program and the historical requirements of the Royal College program below (note that with the transition to Competence By Design the rotation requirements for the Royal College program are much less explicit as the focus is on ensuring that each trainee receives the experience they need to demonstrate competence in the entrustable professional activities of EM – regardless of the rotations required for a program to get them those experiences).
CCFP training:
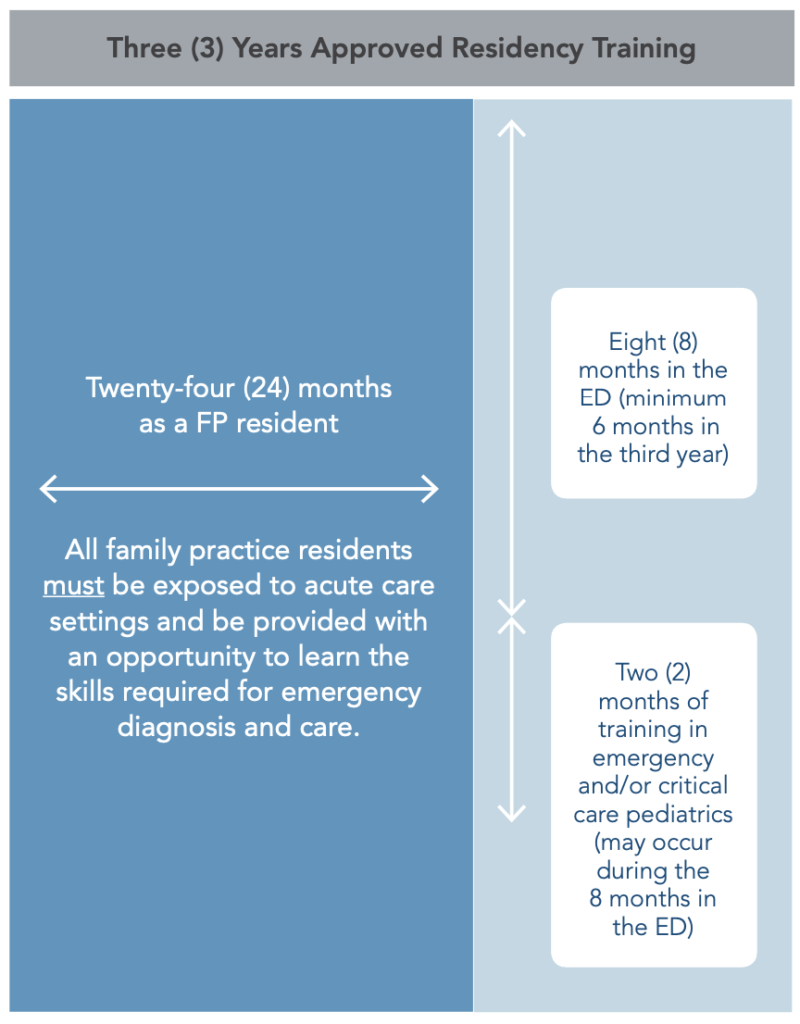
FRCPC training:
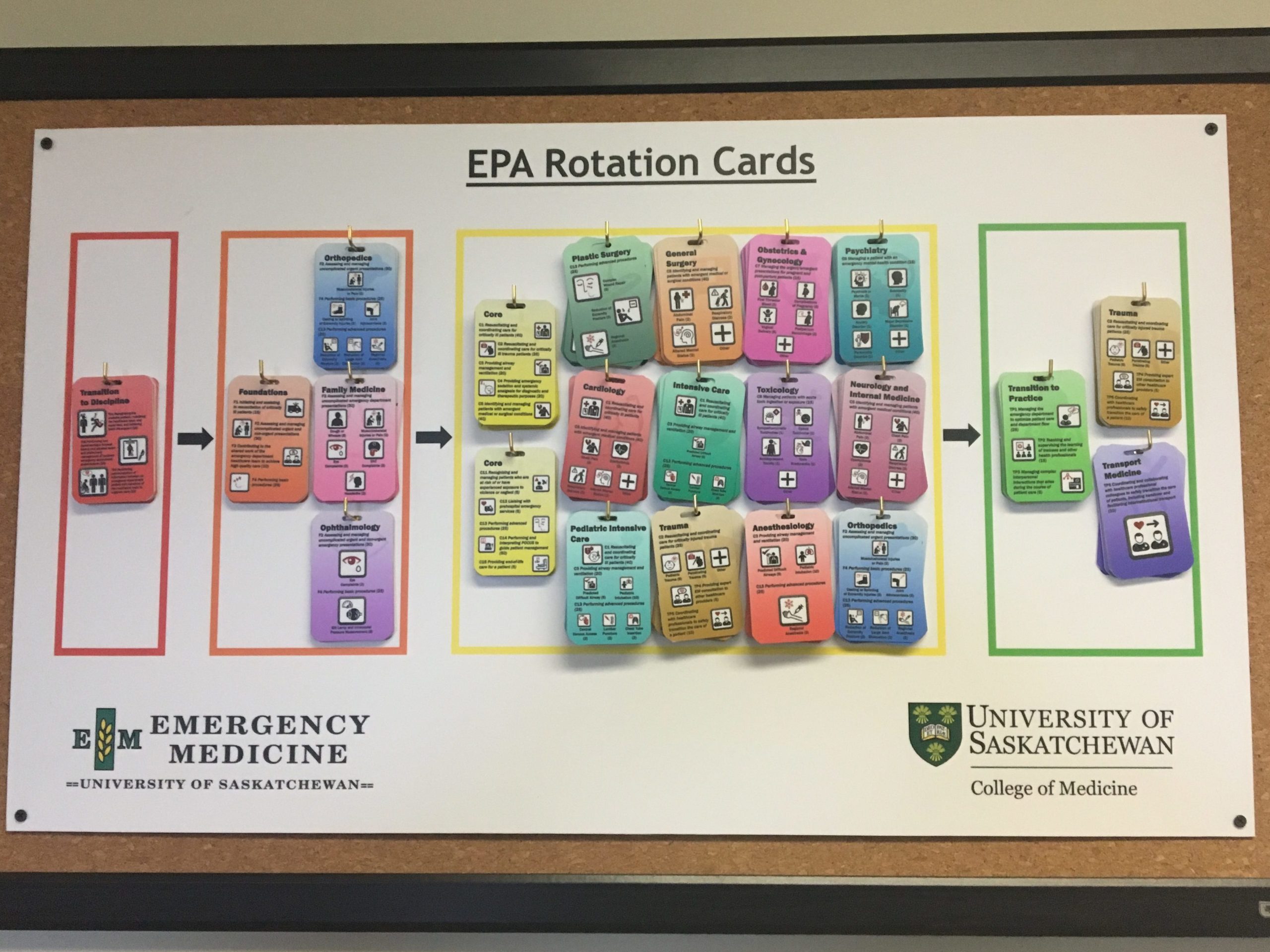
FRCPC programs implemented Competence by Design in 2017. Above is a visual curriculum map for residents showing the rotations they will complete during training at the University of Saskatchewan. As per the Royal College minimum training requirements for EM, programs follow this structure. Broadly, the curriculum consists of Transition to Discipline (~3 months), Foundations (~9 months), Core (~3 years), and Transition to Practice (~1 year, with 6 months devoted to developing niche expertise in an area of EM). The exam has been moved from the end of training to the end of Core / 4th year.
To give a bit more insight into the differences between the programs, this table outlines some of the differences between the two routes with elaboration when needed:
| FRCPC | CCFP-EM | |
| Years of residency | 5 | 3 |
| Years of EM residency | 5 | 1 |
| Payscale | Equivalent | Equivalent |
| One exception to this is that FRCPC’s get paid more than CCFP-EM’s in Quebec. However, the number of specialist (FRCPC) positions in each region is limited by work permits. In all provinces, CCFP-EM’s would begin earning attending wages 2 years prior to their FRCPC colleagues. | ||
| Family Medicine License | No | Yes |
| Fellowships | Yes | Some |
| CCFP-EM’s are eligible for informal fellowships (e.g. simulation, ultrasound) but they are unable to enter Royal College subspecialty residency programs such as Pediatric EM, Toxicology, and Intensive Care. | ||
| Integrated subspecialty time | Variable | No |
| Historically, FRCPC programs allowed up to 12 full months of funded electives to develop a subspecialty interest in EM. This time is often used to complete the first year of a fellowship, complete a Master’s degree, etc. However, within the CBD training program, this period is now a minimum of 6 months during the Transition to Practice stage. The amount of time any individual resident will receive may vary depending upon the program and resident progress. | ||
| Internationally Recognized EM Credential | Yes | No |
| It is possible that EM experience may be considered to allow a CCFP-EM to work internationally as an emergency physician, but the CCFP-EM credential is not considered equivalent to an emergency medicine specialty credential internationally. | ||
| Job prospects | Good | Good |
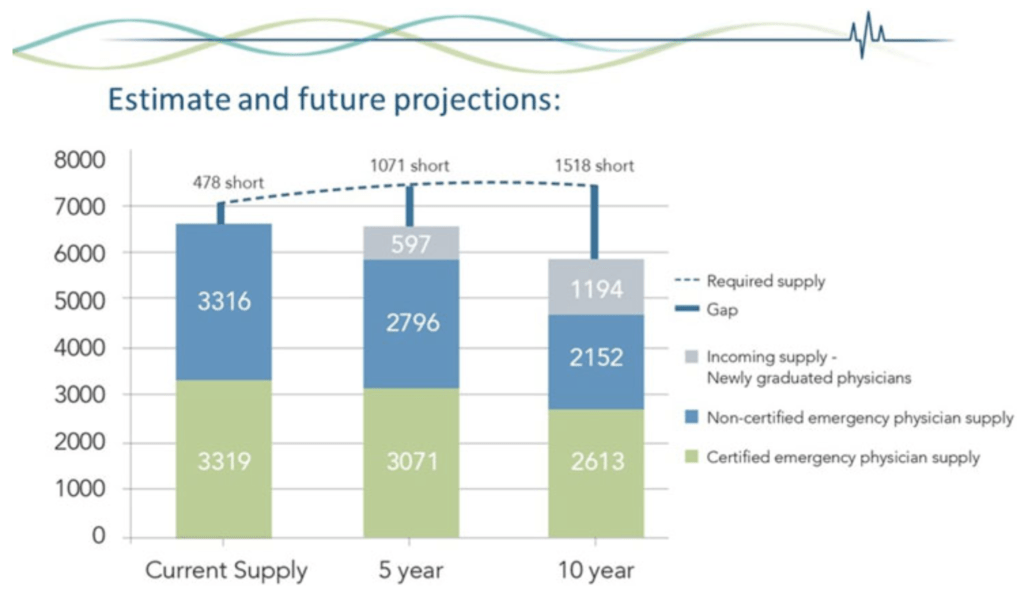
| If you are a credentialed emergency physician (through either stream) it is easy to find work in Canada. I have not spoken to a graduate of either program that has had difficulty finding a job, physicians with both credentials work in large departments across the country, and a recent CAEP workforce study anticipates this being true well into the future. However, there are academic tertiary care hospitals in the country where no CCFP-EM physicians have been hired out of residency in some time. |
Which route is right for you?
I hope this information has helped you consider some of the important aspects of that decision.
The question that tipped me from being unsure to 100% certain that the FRCPC route for me was “Do I want to train for family medicine for two years?” As I had no interest in working as a family physician, I decided that I was not interested in pursuing the CCFP-EM route. I also found the possibility of fellowship training appealing and ended up doing a Fellowship in Medical Simulation at Massachusetts General Hospital before finishing residency and starting work at an academic center.
A note on the numbers game…
Much has been said regarding the increasing competitiveness of Emergency Medicine as a specialty. Here’s some rough data regarding the CaRMS match between 2013 – 2021:
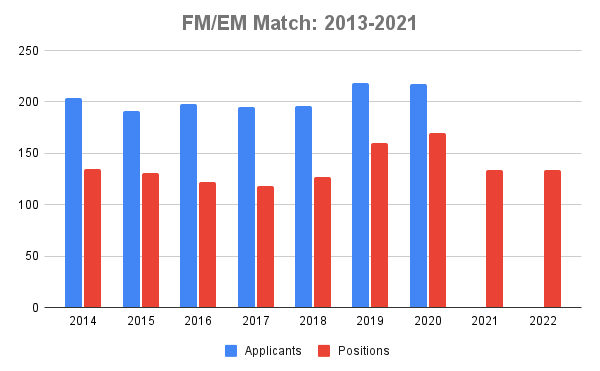
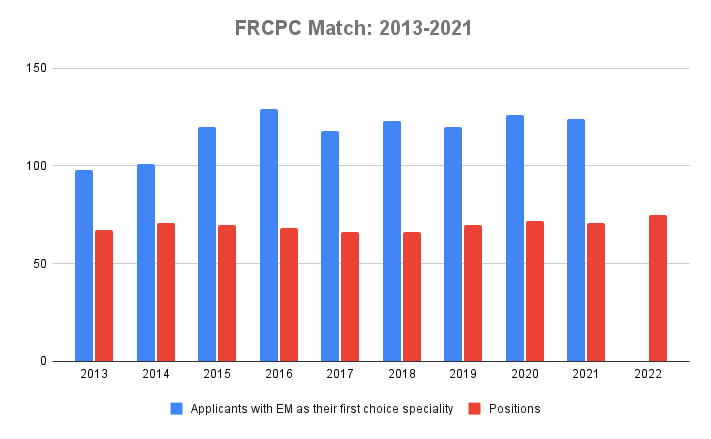
As you can see, the number of applicants applying to the FRCPC program as their first-choice specialty has increased by approximately 20% from 2014-2017 but has remained fairly constant since. The CCFP-EM applicant data was a bit more difficult to get because CaRMS began reporting the number of enhanced skills applicants and positions in aggregate in 2021 whereas they had reported the CCFP-EM numbers specifically before.
| 2020 | 2021* | 2022* | |
| Memorial | 5 | 5 (0) | 5 (0) |
| Dalhousie | 5 | 4 (-1) | 4 (0) |
| Laval | 16 | 8 (-8) | 7 (-1) |
| Sherbrooke | 17 | 8 (-9) | 10 (+2) |
| Montreal | 23 | 11 (-12) | 10 (-1) |
| McGill | 18 | 10 (-8) | 10 (0) |
| Ottawa | 5 | 6 (+1) | 5 (-1) |
| Queen’s | 9 | 8 (-1) | 8 (0) |
| Toronto | 7 | 7 (0) | 7 (0) |
| McMaster | 6 | 6 (0) | 6 (0) |
| Western | 12 | 10 (-2) | 11 (+1) |
| NOSM | 6 | 7 (+1) | 6 (-1) |
| Manitoba | 6 | 6 (0) | 6 (0) |
| Saskatchewan | 10 | 10 (0) | 11 (+1) |
| Alberta | 6 | 7 (+1) | 7 (0) |
| Calgary | 8 | 8 (0) | 8 (0) |
| UBC | 11 | 13 (+2) | 13 (0) |
| Total | 170 | 134 (-36) | 134 (0) |
As of 2022, the FRCPC has 75 available positions, up from 66 in 2017. The CCFP-EM stream offered 134 spots in 2021, down from 170 in 2020 due largely to a decrease in the number of positions in Quebec. This leads to an overall theoretical match percentage of 58% for the FRCPC and 62% for the CCFP-EM matches (assuming that the number of applicants to the CCFP-EM programs in 2021 was similar to 2019 and 2020)
This post was peer reviewed by Eve Purdy, Paul Olszynski (CCFP-EM) and Nadim Lalani (FRCPC) prior to its initial publication on May 27th, 2013. It was revised and reposted by Casey Jones and Remi Kandal on January 17, 2021 and previously by Kelly Lien on August 16, 2017. For more CaRMS advice, check out the complete CaRMS Guide. The next post in the CaRMS Guide series is Finding a Mentor.