Editor’s note: This post marks the second in a series of posts outlining the evidence surrounding various aspects of CPR by Dr. Stu Netherton. Follow along as he covers Rate of Compression, Depth of Compression, Chest Wall Recoil, Minimizing Interruptions, and Avoiding Excessive Ventilation.

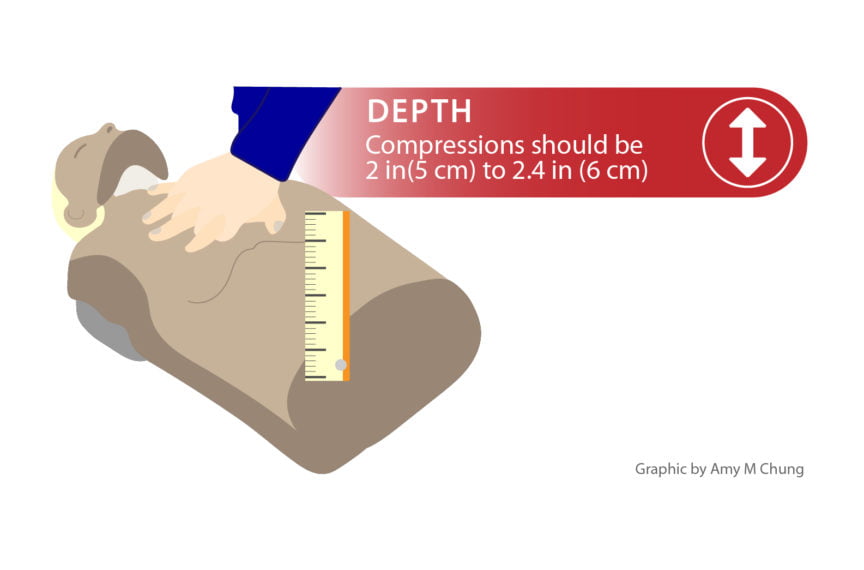
To guide the depth of our compressions during CPR, the 2015 AHA guidelines state:
“During manual CPR, rescuers should perform chest compressions at a depth of at least 2 inches or 5 cm for an average adult, while avoiding excessive chest compression depths (greater than 2.4 inches [6 cm])”
This was a change from the 2010 guidelines in which there was no upper limit to guide compression depth: The 2010 AHA Guidelines for CPR recommend a single minimum depth for compressions of ≥2 inches (50 mm) in adults.
Before worrying about how deep to go, can we go too shallow? The answer is yes. Compression depth of < 38mm has been shown to be associated with decreased ROSC and decreased survival.1,2 The other question to ask is, can we go too deep? And again, the answer is yes. The upper limit was added in the 2015 guidelines as a compression depth of greater than 6 centimeters (or 2.4 inches) was found to be associated with an increased risk of non-life-threatening harm (mainly rib and sternal fractures).3
So we know we shouldn’t go too shallow, and we shouldn’t go too deep, so what is our optimal depth of compression? The answer is somewhere between those two extremes. While the research in this area is rather heterogeneous, it does suggest that achieving a target depth close to 5cm leads to more favourable outcomes compared to shallower depths of compression. 1,2,4–6 The largest study to date showed improved outcomes with compression depth between 40.3 to 55.3 mm, with a peak of positive outcomes at depth of 45.6 mm. 2
It is relatively easy to count your compression rate, someone can watch you to ensure you’re not leaning on the chest during your compressions, but how do we accurately assess our depth? Someone can’t be at the bedside with a ruler. How often do you assess whether or not you’re compressing 1/3 of the anterior-posterior AP chest diameter? How do we know we’re achieving a depth of 45.6mm and not 37mm? Can a CPR provider really know the difference between a few millimetres of compression depth? It has been shown that trained providers of CPR tend to be too shallow, i.e. less than 40mm, and rarely reach a depth over 55mm2, but the use of CPR feedback and debriefing can help. The use of a standalone CPR feedback device, or one integrated into the defibrilator – which provides real-time rate and depth of compressions – during a resuscitation has been shown to help guide the providers efforts, improving the quality of CPR. 7,8Including data from feedback devices when debriefing the resuscitation teams has also shown to improve ROSC on subsequent resuscitation attempts.9 Embracing emerging technologies and constructive team debriefings are easy ways to build high functioning resuscitation teams.
As with all things CPR, each component is closely related to one another. Depth of compressions is no exception. Studies have shown that at compression rates greater than 120 per minute, there is a dose-dependent decrease in depth of compressions 10, and that shallower compression depths have been associated with defibrillation failure.4
Adequate depth can be a difficult part of CPR delivery to achieve, but with feedback devices, feedback simulation sessions, knowing our target depth and practice, we can continue to improve.
Uploaded by Amy Chung.
References
Reviewing with the staff
Adequate depth is critical to create any significant blood flow during CPR. During cardiac arrest the only way to ensure adequate depth is through CPR feedback in real-time. This is absolutely critical. Many device manufacturers do not provide CPR feedback on depth nor the ability to assess depth post-resuscitation but to increase survival, depth is critical and CPR feedback is a must. The AHA is now recommending that as of 2018 all CPR training programs must incorporate real-time CPR feedback to ensure adequate performance of high quality CPR.