This updated episode covers the approach to a common, but icky complaint we will see often in the ED, nausea and vomiting.
[bg_faq_start]Rosen’s in Perspective
In the US, 4% of ED visits are for a chief complaint of nausea and vomiting. In this episode, we cover key aspects of this chief complaint, including the terminology, pathophysiology, associated sequelae, approach to history and physical exam, differential diagnosis, diagnostic workup, and treatment, and classic Rosen’s trivia.
[bg_faq_end]Core Questions:
[bg_faq_start][1] Define the following terms:
- Nausea
- Retching
- Vomiting
- Nausea→ sensation that often precedes vomiting; nausea is associated with increased tone of the duodenum/jejunum with decreased gastric tone. Often, patients are noted to have hypersalivation, repetitive swallowing, and tachycardia.
- Retching→ recurrent rhythmic and synchronized contractions of the diaphragm, intercostal muscles, and abdominal muscles against a closed glottis WITHOUT emptying of gastric contents
- Vomiting→ forceful expulsion of the stomach contents secondary to contraction of the external obliques and abdominal rectus muscles, and the pylorus portion of the stomach. During this process, there is relaxation of the hiatus portion of the diaphragm, gastric fundus/cardia, and the upper esophageal sphincter.
[2] Outline the neural pathway regulating nausea and vomiting.
The neurologic pathways that mediate nausea are not well described, but are postulated to mirror those that regulate vomiting. The neurologic pathways that mediate vomiting are well studied and are outlined below:
Afferents:
- Visceral afferents from the GI tract
- Visceral afferents outside of the GI tract (i.e., biliary system, peritoneum, pharynx, genitalia, and heart)
- Extrameduallary CNS afferents (e.g., vestibular system)
- The chemoreceptor trigger zone (CTZ), located in the area postrema on the floor of the fourth ventricle
Vomiting Centre:
- Located in the lateral reticular formation of the medulla
Efferents:
- Vagus nerve
- Phrenic nerve
- Spinal Nerve
Effectors:
- Diaphragm
- Intercostal muscles
- Abdominal muscles
- Stomach
- Esophagus
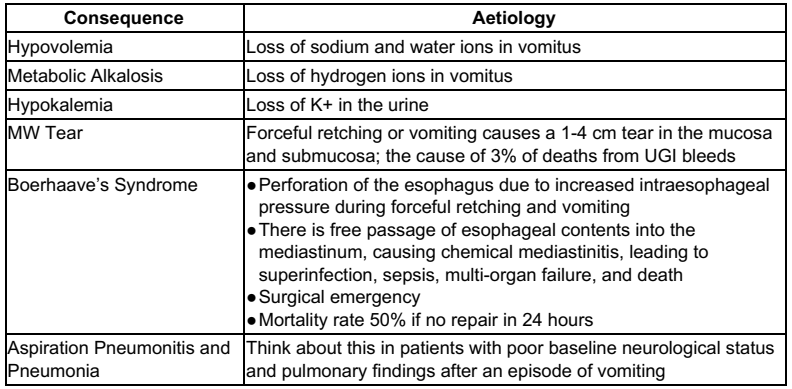
[3] List 6 potential sequelae of vomiting.
Please see Rosen’s 9th Edition Table 26.1 – Potential Sequelae of Vomiting for further detail
[4] Outline an approach to the history in the patient complaining of nausea and vomiting.
A thorough history is required to elucidate the cause of a patient’s nausea and vomiting. Important points to dig into are:
- Timing and duration of symptoms
- Associated CVS/RESP/GI/GU/INFECTIOUS/NEURO complaints
- Previous history of similar events
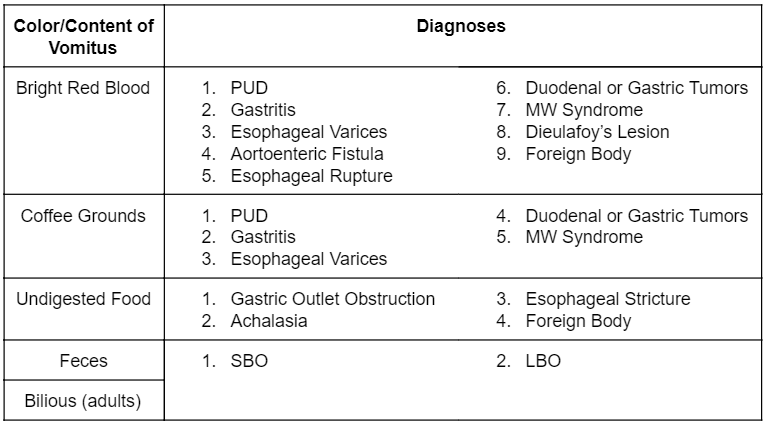
- Characteristics of vomitus
- Exposure to undercooked meats, street foods, well or untreated water
- Medications history
- Social history elucidating use of intoxicants or herbal supplements/natural remedies
Please see Rosen’s 9th Edition Table 26.5 – Differential Diagnosis Based on Contents of Vomitus for further detail
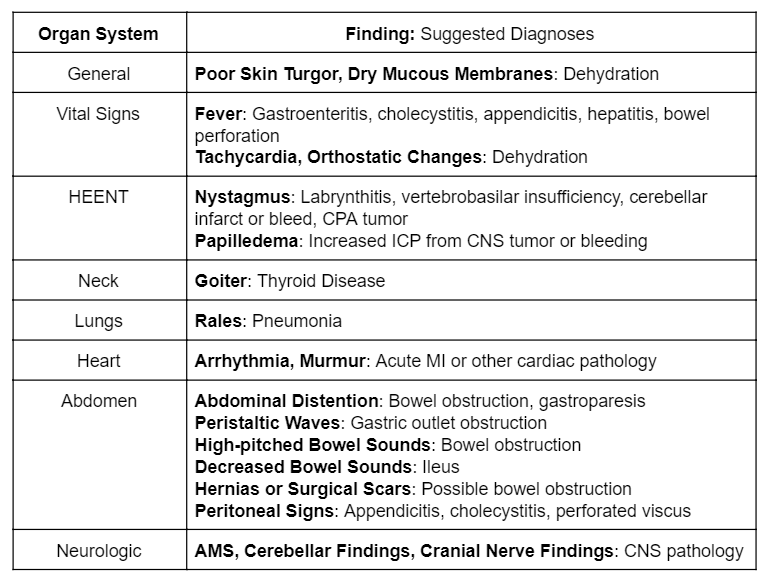
[5] Outline an approach to the physical exam in the nauseated and/or vomiting patient.
Medicine is a clinical science. Remember that a thorough physical examination is essential to determine what is causing this patient’s nausea and vomiting. Consider interrogating the following systems in these patients:
- CNS
- CVS
- RESP
- GI
- GU
Please see Rosen’s 9th Edition Table 26.6 – Physical Examination of the Patient With Nausea and Vomiting for further detail
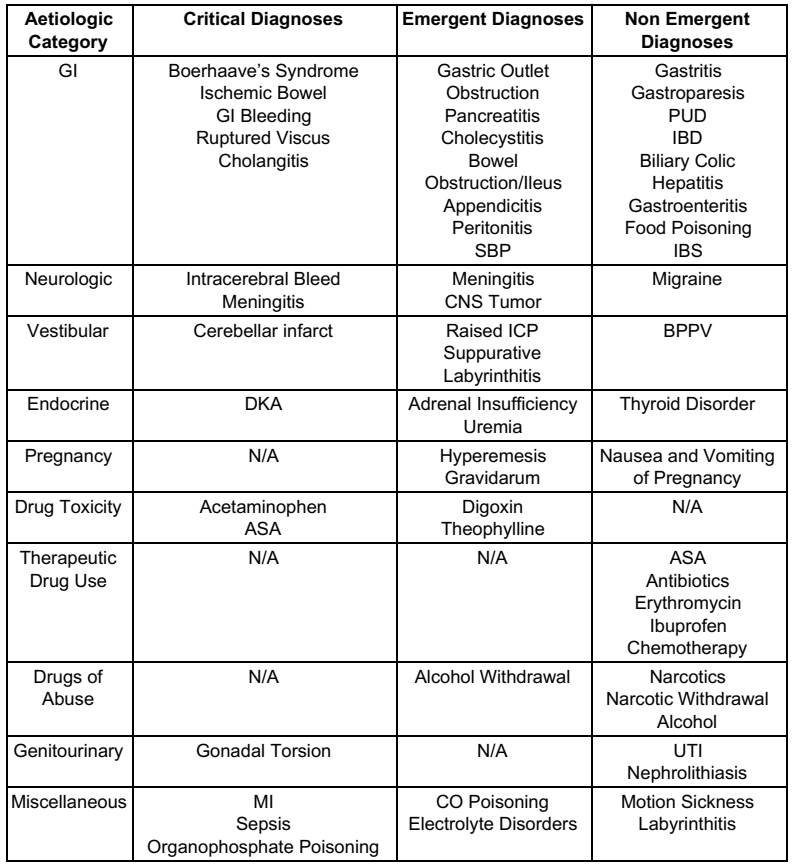
[6] List 10 differential diagnoses for the vomiting patient.
Please see Rosen’s 9th Edition Table 26.4 – Differential Diagnosis of Nausea and Vomiting for further detail
[7] What ancillary tests are indicated in the patient with nausea and/or vomiting?
The ancillary tests you order for the nauseated and vomiting patient are dictated by the history and physical examination. Many patients do not require any ancillary tests. However, consider the following tests in specific clinical scenarios:
- Electrolytes and renal function: protracted or severe vomiting; anticipate hypokalemic hypochloremic metabolic alkalosis or prerenal AKI
- Lipase: nausea, vomiting, and severe epigastric pain
- Urine pregnancy test: all women of childbearing age
- Urinalysis + C/S: sxs consistent with UTI, urolithiasis, or DKA.
- Liver function test +/- ammonia: sxs c/w hepatitis or biliary disease (ammonia may be useful if liver failure is suspected)
- Serum drug levels: if suspected digoxin, ASA, or acetaminophen use/overdose.
- Abdominal US: sxs of cholelithiasis, cholecystitis, renal colic, appendicitis, SBO, or hypovolemia (looking directly at the IVC)
- Abdominal CT: sxs of SBO, appendicitis, or other surgical cause of their nausea and vomiting.
- Head CT or MRI: sxs c/w intracranial etiology
- Chest imaging (CXR or CT): suspicion of perforated viscus or Boerhaave’s Syndrome.
[8] List five antiemetics that can be used to treat the nauseous and vomiting patient.
Please see Rosen’s 9th Edition Table 26.7 – Commonly Used Medications for the Treatment of Nausea and Vomiting for further detail

Wisecracks:
[bg_faq_start][1] What are the three phases of vomiting?
Answer:
- Nausea
- Retching
- Vomiting
[2] What is Hamman’s Sign and what pathology does it point to?
Answer:
- Hamman’s Sign→crunching sound that is synchronized with each heartbeat indicative of air in the mediastinum. May be found in the setting of pathologies, but should trigger concern for Boerhaave’s Syndrome in a patient with nauseated and vomiting.
[3] What medication is indicated in the patient with intractable chemotherapy-induced nausea and vomiting.
Answer:
Dexamethasone 10 mg IV x 1, if refractory to multiple doses of antiemetics (typically ondansetron if chemo-induced emesis)
[bg_faq_end]