This episode of CRACKCast covers Rosen’s Chapter 041, Head Injury. This episode covers a spectrum of head injuries seen in the emergency department along with appropriate management.
Shownotes – PDF link
[bg_faq_start]Rosen’s in Perspective
- Most common causes of head injury: falls, MVC’s
- Leading cause of death for people < 25 yrs old
- There may be no external indicators on someone with a serious TBI
Principles of disease
ANATOMY AND PHYSIOLOGY
- Scalp and cranium : “SCALP MAP”
- Scalp components:
- Dermis: thick layer of skin (skin)
- Subcutaneous tissue: hair follicles, and BLOOD supply (cutaneous)
- Galea: tough fascia (aponeurosis)
- Loose areolar tissue: loose tissue, where subgaleal hematomas form
- Pericranium: firmly attached to the skull
- Skull:
- Frontal, ethmoid, sphenoid, occipital, and TWO parietal + temporal bones
- Temporal bones are the thinnest
- Must consider contrecoup injuries
- Cranial vault can take up to 1900 ml of space
- Brain takes up 80% of the cranial vault
- And is covered by (outside to inside):
- Meningeal dura
- Arachnoid layer
- Pia
- ….then brain
- Frontal, ethmoid, sphenoid, occipital, and TWO parietal + temporal bones
- Brain Divisions
- Cerebrum, cerebellum, brainstem
- CSF surrounds and protects the brain with buffering and cushioning.
- Produced by the choroid plexus (in the lateral ventricles)
- Pathway: ventricles → subarachnoid space → brain and spinal cord
- CSF functions
- Delivers brain substances, eliminates wastes, transports hormones,
- Normal pressure of CSF is 6-20 cm H20
- Blood in the ventricles can cause traumatic hydrocephalus
- Blood brain barrier
- When intact it serves to balance ion and neurotransmitters.
- Post-traumatic cerebral edema affects the permeability of the BBB which can last for hours.
- This can lead to vasogenic edema
- Scalp components:
Brain cellular damage and death – Primary and Secondary Brain Injuries
- Primary:
- Mechanical damage occurring at the time of head injury
- Brain lacerations, hemorrhages, contusions, tissue avulsions.
- Permanent microvascular injury and cellular disruption lasting for hours and days
- Only interventions: able to evacuate traumatic hematomas and reverse these injuries
- Goal should be to promote primary prevention
- Avoid crashes, stop violence, prevent falls)
- Goal should be to promote primary prevention
- Mechanical damage occurring at the time of head injury
- Secondary
- Intracellular and extracellular derangements due to massive depolarization of brain cells and ionic shifts
- See Fig 41-3 in Rosens
- All current therapies aim to prevent secondary neurologic injury
- All injuries lead to metabolic failure, cell membrane disruption, cellular edema, and cerebral edema
- No therapies to date show promise in consistently preventing secondary neurologic injury
What are the secondary systemic insults?
The final neurologic outcome is heavily affected by subsequent secondary brain injuries
[1] Hypotension
Systolic BP < 90 mmHg
- Potentiates ischemia and infarction
- Doubles the mortality from head injury and worsens outcomes!
[2] Hypoxia
- PaO2 < 60 mmHg
- Due to:
- Transient or prolonged APNEA (brainstem compression or traumatic apnea)
- Partial airway obstruction due to blood/vomit/debris
- Chest wall injuries leading to interference in respiratory excursion.
- Pulmonary injury reducing effective oxygenation
- Ineffective airway management (poor BVM, poor intubation, etc.)
- Often occurs in the pre-hospital setting
[3] Anemia
- Reductions in the oxygen carrying capacity of the blood → increased mortality due to limited oxygen delivery to the brain
[4] Hyperpyrexia
- >38.5 degrees.
- Thought to worsen injury by stimulating injured brain tissue metabolism
[5] Hypercarbia
- Leads to more blood flow to the brain and will increase ICP
[6] Coagulopathy
- Leads to more bleeding inside the brain (subdural, etc.)
[7] Seizures
- Brain activity increases, depletes glucose stores and creates more toxic byproducts
Pathophysiology
–> Increased ICP
- Three methods to decrease ICP:
- 1) Hyperventilation
- 2) Osmotic and diuretic agents
- 3) CSF drainage
- Has no prospective data to support its use, but is done to avoid brainstem compression and arrest
Brain Swelling and Cerebral Edema
- Congestive brain swelling
- Increased intracranial blood volume due to hyperemia caused by vasodilation needed to maintain increased metabolic needs of damaged brain tissue after head injury
- Cerebral edema
- Absolute increase in cerebral water content
- Diffuse cerebral edema may occur with a head injury, but does NOT correlate with the severity of head injury
- 3 findings: loss of sulci, loss of grey-white interface and collapsed ventricles
- Vasogenic edema
- Failure of the BBB endothelial junctions → leading to transvascular leakage
- Cytotoxic edema
- An intracellular process due to membrane pump failure
- Usually due to post-traumatic ischemia and tissue hypoxia caused by a decrease in cerebral blood flow (due to dying cells)
- This is often worsened by increasing ICP
- Absolute increase in cerebral water content
1) List 7 causes of altered LOC in the trauma patient
Altered LOC
- Consciousness is the awareness of self and the environment
- Requires a functioning RAS and cerebral cortices
- Etiologic factors for altered LOC:
- Hypoxia
- Hypoglycemia
- Post-seizure
- Post-intoxicating drugs
- Brain or brainstem compression due to swelling or a mass
- Bleed
- Hypotension
2) List four herniation syndromes.
- Uncal herniation
- Most common type: due to traumatic extra-axial hematomas in the lateral middle fossa or temporal lobe.
- Central transtentorial herniation
- Due to an expanding lesion at the vertex, frontal, or occipital brain
- Upward transtentorial herniation
- Expanding posterior fossa tumour
- Signs:
- Rapid decline of LOC, downward conjugate gaze, pinpoint pupils
- Cerebellar-Tonsillar herniation
- Due to cerebellar tonsils herniating through the foramen magnum
- Cerebellar mass or large central vertex mass
- Signs:
- Sudden resp / cardio collapse, pinpoint pupils, flaccid quadriplegia (corticospinal tracts are compressed)
- Due to cerebellar tonsils herniating through the foramen magnum
Describe the pathophysiology of uncal herniation and the typical presentation.
See Rosen’s Figure 41-5 in Head Injury Chapter
Signs: Anisocoria, ptosis, impaired EOMs, sluggish pupil on the IPsilateral side
- A dilated, non-reactive pupil = compressed oculomotor nerve
- CONTRALATERAL: (+) Babinski’s sign (upward going big toe and outward fanning of the other toes)
- Contra-lateral hemiparesis, then may progress to bilateral decerebrate posturing
- As the brainstem becomes compressed: agitation > restlessness > confusion > coma > cushing’s reflex > cardiac collapse
Describe the presentation of central herniation.
Signs: May be subtle LOC changes → bilateral motor weakness → pinpoint pupils → increased muscle tone and bilateral babinski’s → Posturing, respiratory pattern changes (sighs, yawns, shallow-irregular breaths, then respiratory arrest)
3) Describe how cerebral blood flow in relationship to the following parameters: PO2 , PCO2 , MAP and ICP. What are the indications for ICP monitoring?
- Brain consumes 20% of the body’s oxygen content and optimal cerebral blood flow is maintained by the cerebral vessels adapting to physiologic conditions: between MAP 60-150 mmHg
Cerebral vasoCONstriction:
- Hypertension, alkalosis, hypocarbia
- This is why we hyperventilate coning or severe head injury patients showing signs of brain herniation — to vasoconstrict (pg. 341) — 1 mmHg of CO2 change can decrease cerebral diameter by 2-3%
- If the PCO2 becomes too low, the brain can become ischemic.
- The Goal is 30-35mmHg of CO2
- This loses its effectiveness after 12 hrs and the brain can become DAMAGED due to vasodilation and reperfusion injury
- Therefore hyperventilation only for TBI patients showing ACUTE signs of increased ICP
Cerebral vasoDILation:
- Hypotension, acidosis, hypercarbia
- In a TBI – the brain is not able to respond normally to changes in oxygen levels
- Normal functioning BBB: declines in P02 lead to cerebral vessel dilation, however injured brain is unable to properly DILATE to improve cerebral oxygenation (and also remove metabolic end products that are toxic to the brain)
- In a TBI – the brain is not able to respond normally to changes in oxygen levels
Cerebral perfusion pressure: CPP = MAP – ICP (resistance to CBF by mean systemic pressure and ICP)
- CPP is the pressure gradient across the brain
- CBF = is constant from 50-160 mmHg
- ICP effects are greater than mean systemic venous pressures
- Goals: to maintain MAP and reduce ICP so that CPP can sustain metabolic needs.
So in summary:
- PCo2 = direct relationship with CBF. So, high pco2 higher ICP.
- PO2 = inverse relationship with CBF
- MAP = direct
- ICP = inverse
What are the indications for ICP monitoring?
From Trauma.org:
- Severe head injury (GCS <9)
- Moderate head injury (GCS 9-12) who cannot be monitored with serial neurological exams
4) What is the Canadian CT head rule? What are the inclusion criteria. What is the New Orleans CT head rule? What are the inclusion criteria? Which test is more sensitive? More specific?
- (adapted from: http://thesgem.com/2015/02/sgem106-o-canada-canadian-ct-head-rule-for-patients-with-minor-head-injury/)
What is the Canadian CT head rule?
From CJEM:
Primary Outcome:
Need for neurological intervention, defined as need for neurologic intervention as death within 7 days due to the head injury or need with 7 days for craniotomy, elevation of skull fracture, intracranial pressure monitoring, or intubation for head injury. ~ from thesgem.com
What are the inclusion criteria?
- “Adult patients presenting to the emergency departments at 10 large Canadian hospitals with Glasgow Coma Scale 13 or greater within 24 hours after blunt head trauma resulting in witnessed loss of consciousness, amnesia, or witnessed disorientation.”
- Age < 16 excluded
- Minimal trauma with no LOC/amnesia/disorientation
- Anticoagulation
- PTSs
- Unclear hx, focal deficits, penetrating injury, depressed skull #
What is the New Orleans CT head rule?
Head CT is required if one or more of the following are present:
- Headache
- Vomiting
- Age >60yr (!)
- Drug or Alcohol Intoxication
- Persistent anterograde amnesia (deficits in short-term memory)
- Visible trauma above the clavicles
- Seizure
What are the inclusion criteria?
- Inclusion Criteria: Age >18, GCS 15 and Blunt head trauma occurring within previous 24hr causing LOC, amnesia, or disorientation
Which test is more sensitive?
- Both 100% sensitive for pt’s needing neurosx intervention
More specific?
- Canadian CT head rule!
- “Both the New Orleans and the Canadian rules had 100% sensitivity, but the Canadian Rule had a higher specificity for all three outcome measures (36.3 versus 10.2 to identify traumatic intracranial lesions on CT, 35 versus 9.9 for clinically important brain injuries, and 80.7 versus 9.6 to identify need for neurosurgical intervention).” ~ from thesgem.com
5) What is a concussion? How is a concussion managed? What are potential complications? Define second impact syndrome & return to play
Concussion:
- Is a complicated minor TBI
- Commonly occurring from head injury in collision sports
- Leads to short-lived distortion of axons and neuroanatomy
- Levels of neurotransmitters remain elevated and a hypermetabolic state persists up to weeks — which can cause secondary injury
- Functional PET scanning is the only imaging that shows signs of damage after head injury
- Post-concussive syndrome
- Affects cognitive, psychomotor, behavioural performance
- Headache, sensory sensitivity, memory/concentration problems, sleep changes, mood changes, etc.
- People with dizziness, headache, and nausea early after head injury may have a 50% chance of having symptoms at 6 months
- Affects cognitive, psychomotor, behavioural performance
- RE-injury risk is highest within the first 10 days
- Due to deficits in balance, reflexes, speed, information processing
- Second impact syndrome:
- When an athlete sustains a second concussion before recovering completely from the previous concussion
- Causes a rapid, at times fatal decline, due to cerebral edema
- THIS IS a debated entity – some question its validity and existence
- A careful field side assessment is important for determining who can play and who can’t.
- Return to play protocols are important – in a stepwise approach
- Only move on to the next step if the athlete is asymptomatic
- Generally athletes should return to play one week AFTER they are totally asymptomatic (during training and exercise)
- Link to CDC Return to Activity Guidelines
6) Outline the ED management goals of TBI.
| SEVERE GCS<8 or intra-cranial contusion/hematoma by CT
| Out of hospital care:
| Notes:
Depends on:
|
| Emergency department care: Airway
Hypotension
Hyperventilation
Osmotic agents
Barbiturates
Steroids
Hypothermia
Cranial decompression
Seizure prophylaxis
Antibiotic prophylaxis Risk in:
Not for mere otorrhea/rhinorrhea Miscellaneous:
| Ancillary evaluation: Lab tests
Neuroimaging
Disposition Consultation
Priority management
| |
| Moderate GCS 9-13 | Clinical features:
Management:
Disposition:
Complications:
|
Damage:
When no neurosurgeon is available and a patient develops an acute herniation syndrome which does not respond to hyperventilation and mannitol, ED trephination and hematoma evacuation should be considered Some may need followup MRI to look for lesions not seen on CT |
| Mild* TBI
Brief and temporary Interruption of neurologic function | Neurobiological damage, with no damage to microstructures
This is a CLINICAL diagnosis
Clinical and historical features:
High risk Features:
Low risk – factors: – see box 41-3
Delayed complications likely to occur in:
| Due to “heightened ionic flux, surges in levels of glutamate, enzyme pathway disruptions, accumulation of lactate, and nitric oxide”; axonal stretching and twisting
Imaging
Best approach: selective CT scanning vs. Observation based on risk stratification
Ancillary studies:
Disposition:
|
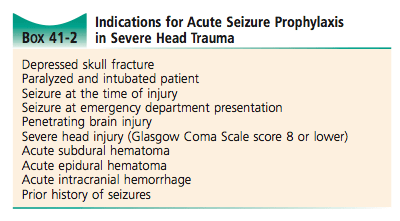
What are the indications for seizure prophylaxis following TBI?
What are the indications for antibiotics in TBI?
- Penetrating TBI
- Depressed skull #
- Complex, contaminated, deep scalp lacerations
- Fever in someone with a basilar skull #
- ***prophylactic abx in the acute setting of CSF leaks and basilar skull fractures are NOT recommended*** – but they do decrease the incidence of meningitis (no clear consensus)
What are the complications after TBI?
Neurologic complications
- Seizures
- Acute PTSs
- Brief
- Self-limited
- Very frequent in children
- Subacute PTSs – 24-48 hrs post
- Due to worsening cerebral edema, small hemorrhages, penetrating injuries
- Prophylaxis reasons: – see box above
- Med Hx of seizures Or any seizure
- intracranial blood
- Penetrating wounds
- Unable to assess seizure activity because of: low GCS, paralysis,
- Meds:
- Phenytoin or fosphenytoin
- No recommendations to suggest long term prophylaxis – this depends on their clinical course
- TBI is thought to account for 20% of adults with epilepsy – and late seizures may present up to 12 yrs post injury
- Acute PTSs
- CNS infections
- Meningitis after basilar skull fractures
- Fever, AMS, focal findings,
- Common in people with CSF leaks
- Fever occurs within 3 days of injury
- Caused by pneumococcus
- Trxt: ceftriaxone and vancomycin
- Fever > 3 days – usually due to gram -ve
- Txt: ceftriaxone with vancomycin
- ***prophylactic abx in the acute setting of CSF leaks and basilar skull fractures are NOT recommended*** – but they do decrease the incidence of meningitis (no clear consensus)
- Caused by pneumococcus
- Brain abscess
- Rare
- May be part of a fragment of bone left in the cranium or post-op complication
- Post-traumatic fistulae with tracts into sinuses are a risk factor
- S+s:
- Headaches, vomiting, fevers, declining mental status, increased ICP, focal findings, nuchal rigidity, seizures
- NEED contrast enhanced CT head
- LP is dangerous and should not be done in someone with signs of increased ICP
- Trxt: is surgery, unless there is isolated cerebritis.
- Common bugs: gram -ve anerobes and staph aureus .
- Cranial-osteomyelitis
- Pain, tenderness, erythema at the site
- MAy need bone scans to make the dx,
- Abx, surgery are the treatment
- Pain, tenderness, erythema at the site
- Fever occurs within 3 days of injury
- Meningitis after basilar skull fractures
Medical complications
- Disseminated intravascular coagulation
- Injured brain releases tissue thromboplastin. — which activates the extrinsic clotting system → can lead to DIC
- Increased risk of intra-cranial hemorrhage
- Dx:
- INR, PTT, platelets, fibrinogen levels, fibrin degradation products.
- Tx:
- To correct these abnormalities
- Patients should receive prophylactic LMWH to prevent VTE
- They do not worsen ICH hematoma expansion
- Cardiac dysfunction
- A clear relationship between intracranial bleeding and cardiac dysrhythmias:
- In 50% of ICH, and 70% of cases of SAH
- Etiology may be from concurrent blunt chest injury and/or underlying cardiac disease
- Pathophysiology thought to be from autonomic nervous system dysfunction (changing ventricular depolarization); high levels of catecholamines,
- Lead to:
- SVT
- Diffuse large upright or inverted T waves
- Prolonged QT interval
- ST segment elevation or depression
- U waves
- Key priority: to ensure adequate brain perfusion and oxygenation ; some may need cardiac monitoring!
- Lead to:
- Neuro-cardiogenic pulmonary edema
- May develop in minutes to days post injury
- Pathophysiology hypothesis:
- Catecholamine surges
- Blasts of elevated hydrostatic forces and and increased capillary permeability due to the primary brain injury
- A systemic inflammatory reaction
- Key goal is to lower ICP
- CLOSE ventilator management is essential
- A clear relationship between intracranial bleeding and cardiac dysrhythmias:
7) What are 7 clinical features of basal skull fracture?
- Basilar skull fracture findings: see box 41-1:
- Blood in ear canal
- Hemotympanum
- Rhinorrhea
- Otorrhea
- Battle’s sign (retro auricular hematoma)
- Raccoon’s sign (periorbital ecchymosis)
- Cranial nerve deficits:
- Facial paralysis
- Decreased auditory acuity
- Dizziness
- Tinnitus
- Nystagmus
- Carotid bruit (carotid artery injury) – hyperflexion and extension injury
Wisecracks
[1] CT tips: Three signs of cerebral edema on CT, Five differences on CT between SDH And ED, List 3 CT findings in DAI
Three signs of cerebral edema on CT
- Sulcal effacement
- Loss of grey white differentiation
- Compression of ventricles (ventricular effacement)
Five differences on CT between SDH and EDH
- SDH
- Crescentic (crescent moon shaped)
- Crossing suture lines – more extensive
- Layers
- Damage to the bridging veins
- EDH
- Lens shaped
- One cranial bone space
- Middle meningeal artery damage
List 3 CT findings in DAI
- Trick question!
- “CT is particularly insensitive to non-haemorrhagic lesions (as defined by CT) only able to detect 19% of such lesions, compared to 92% using T2 weighted imaging. When lesions are haemorrhagic, and especially when they are large, then CT is quite sensitive. As such, it is usually a safe assumption that if a couple of small haemorrhagic lesions are visible on CT, the degree of damage is much greater.”~ from radiopaedia.org
[2] What are: the Monroe-Kellie doctrine, the Cushing’s reflex, Kernihan’s notch and how does this syndrome present?
Monro-kellie doctrine
- Sum of brain volume, CSF, and blood must remain constant, so increases in any one leads to decreasing volumes of the others
- The CSF is the first to move out of the cranial vault. Once the 50-100 ml of space is filled ICP increases and CPP is compromised
- Vasoparalysis occurs and the autoregulation mechanics fail. → cerebral vasodilation → vasogenic edema → increases in ICP → cerebral blood flow cases and brain death occurs
Cushing’s reflex
- Hypertension, bradycardia, fluctuating respiratory effort – specific to increased ICP, but only occurs 30% of the time
- When a herniation syndrome presents, mortality is nearly 100% unless urgent reversal is undertaken
What is kernihan’s notch syndrome, and how does this syndrome present
*Kernohan’s notch syndrome* false localizing of motor findings due to contralateral cerebral peduncle compression (midbrain) by the tentorium cerebelli.
- It is a FALSE localizing sign: ie. the patient has a left SDH causing an uncal herniation to the right, producing decreased LOC and LEFT (rather than right) sided hemiparesis.[bg_faq_end]
This post was copyedited and uploaded by Riley Golby (@RileyJGolby).