As a senior resident, I am continually humbled by the practical questions of junior residents that I cannot answer. While practicing ultrasound-guided knee aspiration last week, a resident asked for clarification about a conversation she had had with an Orthopedic surgeon about the suprapatellar bursa.
A patient was seen in the Emergency Department with a red, hot, swollen knee, so the usual “rule-out septic joint” workup was initiated. Whether by difficult landmarking or initial dry tap, the resident ended up sending a sample from what she believed was the suprapatellar bursa. When the orthopedics resident saw that the tap was labeled as being from the bursa, they said it would have to be repeated. The junior resident asked me:
Isn’t the suprapatellar bursa continuous with the knee joint? If it’s an easy target, shouldn’t we just tap that?
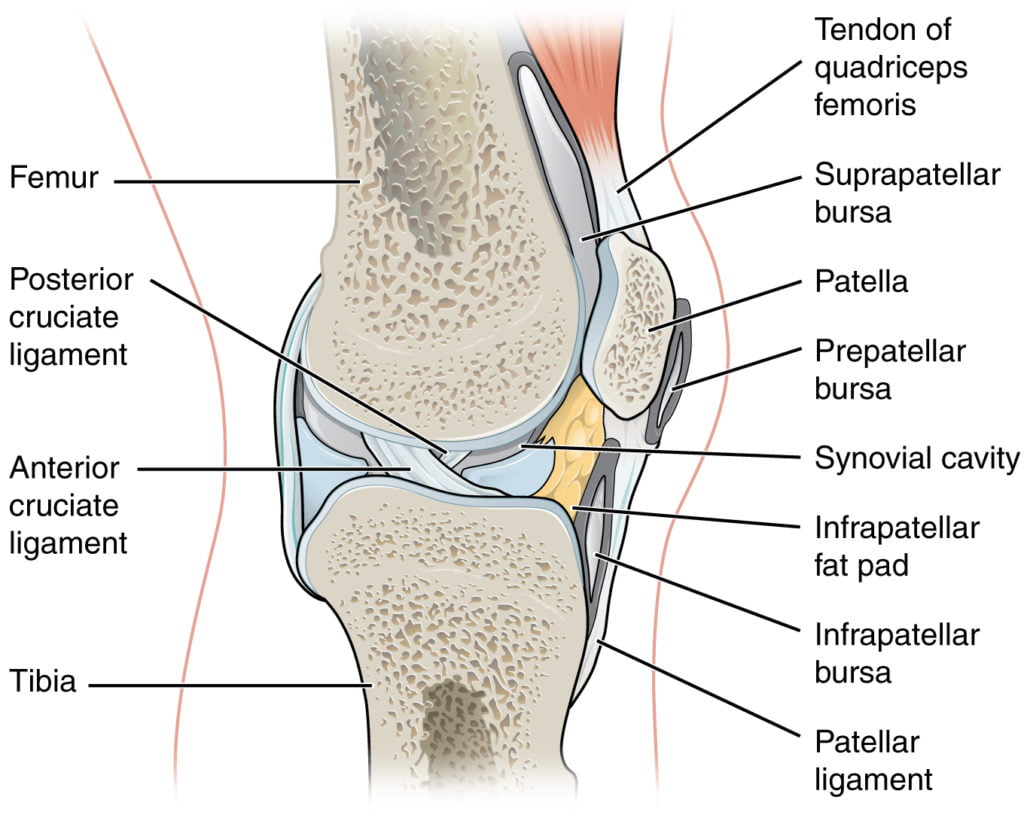
Looking at anatomy renderings, tapping the bursa seems pretty easy, especially when clinical knee effusions make the bursa seem so big and juicy:
Reluctant to answer incorrectly, I collected opinions from Emergency Medicine attendings, Orthopedic surgeons, and PhD Anatomists. Though there was consensus that we should not be purposefully tapping the bursa as opposed to the knee joint, there seemed to be different opinions on whether or not the bursa was truly continuous with the joint, and if the suprapatellar approach to aspiration samples joint or bursa (or both!). The slim pickings of anatomical studies on the bursa actually reflect this ambiguity: 16% of suprapatellar bursae are not continuous with the knee joint.1
Embryologically, we all have an imperforate suprapatellar septum, but from around the 5th month of gestation on, most knees develop a perforation or complete loss of the septum, yielding a continuous joint space.2

This figure1 helps understand spatially that the joint tracks proximal to the patella (p) in an effusion, even if the bursa (b) has a full septum (arrows).
In Summary
In most patients, the suprapatellar bursa is continuous with the joint space. According to the expert opinions I solicited, it is unlikely that a knee with a discrete isolated bursa will look any different than a continuous bursa. Because the knee joint extends proximally beyond the patella regardless of bursa anatomy, there will likely always be the familiar “fullness” above the patella in a large knee effusion. I am speculating, but it seems unlikely that a suprapatellar diagonal approach to knee aspiration would sample a septated bursa and not the joint space, since a septated bursa would likely remain small and be displaced superiorly/proximally.
Similarly, do not confuse “the suprapatellar approach” with “tapping the suprapatellar bursa”. The angle of one’s needle is intended to track beneath the patella (or at least the ‘j’ area on the previous image), understanding that in 84% of people, you may hit an effusion that is indeed continuous with the bursa.
This still leaves a number of unanswered questions. For example, emergency physicians are becoming slick with ultrasound. If ultrasound was used to find a pocket of fluid (perhaps a blind lateral approach seemed difficult due to osteophytes!), how frequently would we find the suprapatellar bursa and sample that? In fact, some ultrasound organizations and protocols specifically say to find the bursa and sample it! In 14% of people, this might be an isolated septated bursa that should not be used to rule out a septic knee. Conversely, how many cases of discrete suprapatellar bursitis have been sampled and erroneously assumed to be septic arthritis?
Further conversations about this might be “knee-ded”.
This post was uploaded by Patrick Boreskie (@PBoreskie)
References
- 1.Zidorn T, Schäfer H. Morphologic variants of the proximal knee-joint cavity. An anatomical and radiological study. Surg Radiol Anat. 1992;14(2):141-146. doi:10.1007/bf01794891
- 2.Zidorn T. Classification of the suprapatellar septum considering ontogenetic development. Arthroscopy. 1992;8(4):459-464. doi:10.1016/0749-8063(92)90008-y
Reviewing with the Staff
This is a very important topic, as the ability to access synovial fluid for analysis is the only way to definitively rule out, or rule in septic arthritis, and can drastically alter the treatment and disposition of a patient presenting with a swollen, painful joint. Most ED practitioners are proficient at arthrocentesis of knee joints with a blind approach, but ultrasound has become an invaluable asset in assisting access to other joints, such as the ankle, hip, wrist, elbow, and shoulder. Many of these joints are infrequently tapped, have smaller volumes of fluid, or do not have a straightforward landmark approach to them.
But what do we do when our standard landmarking approach to the knee fails? Is it because there is no significant joint effusion, or is our needle not going where it needs to go? Many practitioners will advocate for a suprapatellar approach, regardless of whether we know we are sampling the joint or the suprapatellar bursa, as the majority of patients have continuity of fluid. If there is a significant enough joint effusion it will rise above the patella, regardless of whether or not the joint and bursa are continuous. A convincing case can be made that a suprapatellar aspiration indicative of infection should be treated as a septic joint until proven otherwise, regardless of the origin of the fluid. This could lead to a small subset of patients who have both an incongruous bursa and an isolated suprapatellar bursitis being treated more aggressively than needed, but this would be a preferable outcome to the opposite situation. Ultimately, it is imperative to have this discussion with the consultant Orthopod at your centre, as they will be the physician responsible for definitive management of a large septic joint in the operating room.