Your next patient is a 29-year old G1P0 currently at 24+5 weeks’ gestational age. She has a history of migraines that were previously treated with NSAIDs to good effect. Now, she presents with an ‘unbearable’ headache and nausea, and when you examine her she is clearly uncomfortable. You want to provide her with adequate analgesia, but you remember that certain medications may be contraindicated in pregnancy because of their ability to affect the developing fetus. How do you proceed in managing headaches in pregnancy?
Working up headaches in pregnancy
Primary headache disorders are common both within and outside of pregnancy. However, certain dangerous causes of headache are heightened in or are exclusive to the pregnant state. When assessing the pregnant patient with headache, consider the following diagnoses:
1. Pre-eclampsia: New onset hypertension at or after 20 weeks’ gestation, measuring 140 systolic and/or 90 diastolic over two separate occasions at least four hours apart. Must be accompanied by evidence of end-organ dysfunction (commonly proteinuria >0.3g in a 24-hour urine collection).1 Headache associated with pre-eclampsia fulfills two of the three following criteria:
- Bilateral
- Pulsating
- Aggravated by physical activity
AND is not better accounted for by another diagnosis.2
2. Cerebral venous thrombosis (CVT): Thrombus formation in the cerebral venous sinuses. Most common in the third trimester and potentiated by pregnancy’s prothrombotic state. The majority of affected patients present with headache (70-90%), focal neurologic deficits such as hemiparesis, visual disturbances, impaired level of consciousness and papilledema.3
3. Idiopathic intracranial hypertension: Defined as an increased intracranial pressure with no organic cause. More common in overweight or obese women. Patients present with headache worse with Valsalva (90%), visual changes (transient vision loss, diplopia) and papilledema. Opening pressure with lumbar puncture is >25 mmH2O with normal CSF.2,4,5
4. Pituitary apoplexy: Increased pituitary size during pregnancy (due in part to lactotroph hyperplasia/hypertrophy) predisposes the pituitary to ischemia and thrombosis. The disorder manifests as headache (90%), nausea (80%) and loss of visual fields (71%). Pituitary hormone deficiency may result.6
Primary headache treatment options
By history, you determine that the patient has no red flags for the above disorders. You conclude that the patient has a primary headache disorder and the next step is determining your plan to treat both the headache and associated symptoms including nausea and vomiting. You read that some medications normally used to treat these conditions are contraindicated in pregnancy, including neuroleptics such as Haldol (risk of limb defects) and ergotamine (risk of increased uterine contractility and miscarriage).
Consequently, you follow the below treatment ladder:4,5,7–10
Table 1. A proposed medication ladder for treatment of headache and migraine in pregnancy.
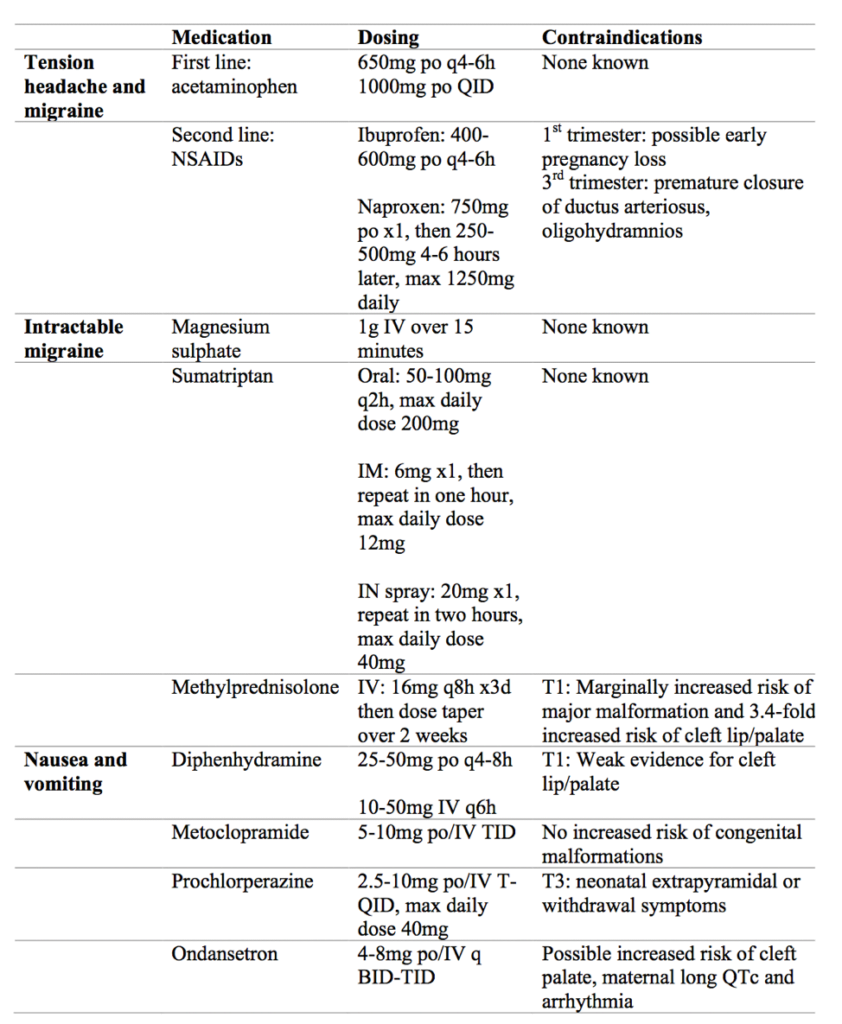
You try two sequential doses of acetaminophen with diphenhydramine. While the patient’s nausea improves, she complains of ongoing pain at your next reassessment so you initiate a dose of metoclopramide and IV magnesium sulphate. After her IV finishes, your patient reports significantly improved pain and nausea. You send her home with follow up to her primary care physician, and advise her to return if she develops red flag symptoms including thunderclap headache or neurologic deficits including blurry vision, focal weakness, dysarthria, dysphagia, or intractable nausea and vomiting.
This post was copyedited and uploaded by Kimberly Vella.
References:
- 1.Magee L, Helewa M, Rey E, HYPERTENSION G, STRATEGIC T. Diagnosis, evaluation, and management of the hypertensive disorders of pregnancy. J Obstet Gynaecol Can. 2008;30(3 Suppl):S1-S2. https://www.ncbi.nlm.nih.gov/pubmed/18817592.
- 2.Revell K, Morrish P. Headaches in pregnancy. Obstet Gynecol. May 2014:179-184. doi:10.1111/tog.12101
- 3.Allroggen H, Abbott R. Cerebral venous sinus thrombosis. Postgrad Med J. 2000;76(891):12-15. https://www.ncbi.nlm.nih.gov/pubmed/10622773.
- 4.Schoen J, Campbell R, Sadosty A. Headache in Pregnancy: An Approach to Emergency Department Evaluation and Management. WestJEM. March 2015:291-301. doi:10.5811/westjem.2015.1.23688
- 5.Negro A, Delaruelle Z, et al. Headache and pregnancy: a systematic review. J Headache Pain. October 2017. doi:10.1186/s10194-017-0816-0
- 6.Grand’Maison S, Weber F, Bédard M-J, Mahone M, Godbout A. Pituitary apoplexy in pregnancy: A case series and literature review. Obstet Med. September 2015:177-183. doi:10.1177/1753495×15598917
- 7.UK Medicines Information (UKMi). How Can Nausea and Vomiting Be Treated during Pregnancy? NHS; 2017:10. https://www.sps.nhs.uk/articles/how-can-nausea-and-vomiting-be-treated-during-pregnancy-2/.
- 8.Quinla J, Hill D. Nausea and vomiting of pregnancy. Am Fam Physician. 2003;68(1):121-128. https://www.ncbi.nlm.nih.gov/pubmed/12887118.
- 9.Duong S, Bozzo P, Nordeng H, Einarson A. Safety of triptans for migraine headaches during pregnancy and breastfeeding. Can Fam Physician. 2010;56(6):537-539. https://www.ncbi.nlm.nih.gov/pubmed/20547518.
- 10.Bigal M, Bordini C, Tepper S, Speciali J. Intravenous magnesium sulphate in the acute treatment of migraine without aura and migraine with aura. A randomized, double-blind, placebo-controlled study. Cephalalgia. 2002;22(5):345-353. https://www.ncbi.nlm.nih.gov/pubmed/12110110.
Reviewing with the Staff
The evaluation of a headaches is common bread and butter emergency medicine. We carefully consider dangerous diagnoses while at the same time try to provide proper analgesia to the suffering patient. Pregnant patients are also commonly encountered in the ED, which often leads to clinician discomfort and unease. When a woman presents to the ED with a headache during pregnancy, the clinician is tasked with considering a handful of other important headache causes that more commonly affect this special population. While most ED physicians are comfortable with headache management, the usual “cocktail” of medications must be reconsidered in a pregnant patient, keeping in mind the potential for harm to the developing fetus. This review by Dr Tam highlights the reds flags to look out for in headaches during pregnancy as well as options for analgesia and antiemetics with risk profiles for the first, second and third trimester.