Emergency Medicine is known for being a relatively procedure-heavy specialty. Whether it be suturing up a forehead laceration, performing an incision and drainage of a forearm abscess, reducing and casting a Colles fracture, or performing a diagnostic lumbar puncture on a patient with altered mental status, it’s highly likely that you’ll have the chance to perform multiple procedures throughout your EM rotation. However, this also means that you’ll be responsible for documenting the procedure on the patient’s chart. Writing a concise yet thorough procedure note is a skill that is rarely taught in traditional pre-clerkship curriculums, but is important for achieving success throughout your EM rotation.
This blog post will walk you through the general principles of how to write a comprehensive procedure note, with specific examples for some of the more common procedures performed in the Emergency Department: suturing, incision and drainage (I&D), and casting.
General Principles:
Some principles are universal to all forms of medical documentation including procedure notes: your note should be clear, accurate, and contain the date and time the note was written. Beyond that, procedure notes have some unique requirements. Here is a list of elements commonly included in a procedure note:
Type of procedure: For example, a simple laceration repair, diagnostic lumbar puncture, I&D of abscess.
Who performed the procedure: Include both name and designation (e.g. MS3, CC4, PGY2).
Name of the attending physician overseeing the procedure (if relevant)
Indications for the procedure: This can be a simple one-liner (e.g. suturing = for laceration repair). This component is particularly important in situations where you perform a procedure that could potentially have major adverse events (e.g. intubation, conscious sedation).
Patient consent: In this section, note whether the patient provided verbal and/or written informed consent. You should document in this part of the note that the specific indications, risks, and alternatives of the procedure were discussed with the patient. Importantly, did the patient understand the risks of the procedure? If the patient does not have capacity, document that a substitute decision maker (including the name and role in that patient’s life) was contacted and the results of the discussion.
Safety first! Document any key lab values that prove the procedure was done in a safe manner: Some procedures performed in the ED require you to first consider certain lab values, most notably INR, platelets, and hemoglobin level. Procedures that require you to consider these values include but are not limited to: I&D, lumbar puncture, paracentesis, thoracentesis, arterial line placement, and central line placement.
Description of the procedure: This section can be broken down into several parts:
- Procedure prep: what materials were prepared? Was a clean or sterile technique used? How was the patient positioned?
- Anesthesia: document which medications were used as anesthesia, including the route, total dose, and the times that the medications were administered. Note that in procedural sedation there is often a separate nursing chart which documents the various medications that were administered (including dose and time) — this can be referenced.
- Equipment used: for example, suture type or scalpel type.
- Procedural technique: here, walk the reader through the procedure in a step-by-step fashion, including all key steps.
Any complications from the procedure: This includes both major complications (e.g. apnea during conscious sedation requiring intubation) and more minor complications (e.g. apnea that responded to a jaw thrust). In this section you can also include estimated blood loss from the procedure, if relevant. This will often purely be an estimate based on any suctioning that was required and/or the amount of gauze that was soaked. Hopefully, there were no immediate complications that you will need to document; if that is the case, you can simply document that there were no such complications.
Post-procedural vitals (if relevant)
Patient disposition: Most commonly: the patient tolerated the procedure well. However, if they didn’t tolerate the procedure well, what happened? This is also the place where you can document if the patient is coming into hospital or going home post-procedure.
Follow-up plan: What are the next steps that the patient needs to know? For example: family doctor to remove sutures in 5-7 days.
Also note that if a procedure is attempted unsuccessfully, this still needs to be documented! This should follow a similar format, but should also include a description of how or why the procedure was unsuccessful.
Now that we’ve discussed how to write a general procedure note, we’ll walk you through how to successfully write notes for three of the most commonly performed procedures in the ED: suturing, I&D, and casting. We will cater the above template to each of these procedures, as they all have unique requirements.
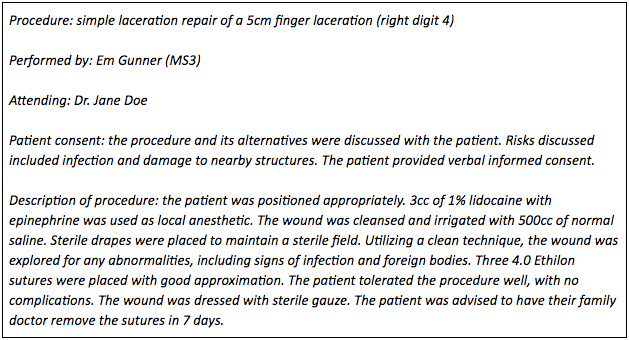
Suturing:
Suturing is likely the most common procedure performed by learners in the ED. As such, prior to your EM rotation, it’s important to not only have your simple interrupted suturing technique down pat, but to also know how to chart the procedure in your note. Using the principles described above, here is an example of how you might chart this note:
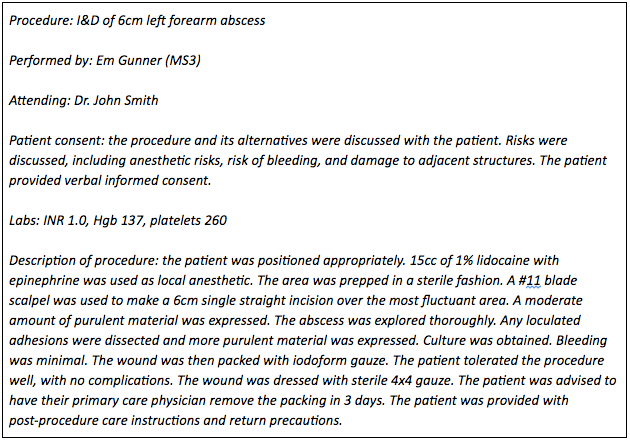
Incision and Drainage (I&D):
I&D is another common procedure performed in the ED, but is one that is less frequently covered in procedural skills training for medical students. As such, it’s a good idea to review the principles of I&D prior to your EM rotation. Here is an example of how you might chart an I&D procedure note:
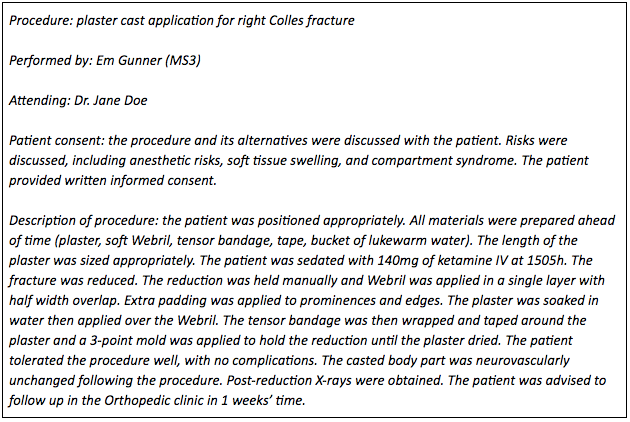
Casting:
Orthopedic injuries are exceedingly common presentations to the Emergency Department, and as a result, fracture reduction and casting are very commonly performed procedures. At some sites, casting is performed by ortho techs or orthopedic residents. However, to ensure that you are prepared for all possibilities, we’ll walk you through how to accurately document a casting procedure note. Here is an example:
Final Thoughts:
Good documentation is a vital part of clinical work, but is rarely emphasized in traditional pre-clerkship curriculums. As a result, it can often serve as a source of stress for many junior learners. No matter what kind of note you are writing, it’s important to remember the basic principles: be accurate, be thorough, and in the ED especially, be concise. Beyond that, when writing a procedure note, remember to incorporate the elements highlighted throughout this blog post; this will allow you to cover the most important points, and will prepare you to chart a procedure note for any kind of procedure you might encounter in the ED. As long as you keep these principles in mind, you’ll be well on your way to achieving success on your EM rotation. Good luck!
Additional Resources:
- https://ucalgary.ca/codeblue/files/codeblue/writing-clinical-notes.pdf
- https://www.schulich.uwo.ca/medicine/undergraduate/docs/clerkship-london/Dictation_Templates.pdf
- http://www.nyjsm.com/myEMresidency/procedure_templates.htm
- http://allanapostol.tripod.com/dci/procedure-note.html
- https://www.venturafamilymed.org/cerner-ehr-tips/autotexts/incision-and-drainage-procedure-note
Reviewing with the Staff
For those of you who are doing procedures in the ED, it is very important to write down the key aspects that have been reviewed by our team in this post.
Consent can be a tough subject to wrap you head around, and so I would suggest diving into the resources set forth by the Canadian Medical Protective Agency (CMPA):
https://www.cmpa-acpm.ca/en/advice-publications/handbooks/consent-a-guide-for-canadian-physicians
There is also a module by the CMPA on phases of surgical care, which reviews what the CMPA thinks would be good content for a surgical note - many of the principles can be generalized into any procedure note. They state that “The operative note should include details of: the technique, anatomical findings and variants, difficulties encountered in the procedure, confirmation that sponge and instrument counts were correct.” All of these have similarities to the types of content you might put into your procedure note - maybe except the sponge and instrument counts, since you won’t be doing any deep cavity surgery and risk leaving equipment behind.
Importantly the CMPA also remind us that the procedure note should be completed as soon as possible, since it can be more difficult to defend care if reports are only available after a post-procedural complication arises or is recognized. They also note that you should consider document the progress of the patient after the procedure, and note whether there were any complications that you immediately noted (e.g. post-procedural bleeding).
Read this module for more hints:
https://www.cmpa-acpm.ca/serve/docs/ela/goodpracticesguide/pages/manage_risk/Reducing_risk_in_surgery/phases_of_surgical_care-e.html
Remember, as a clinical clerk or junior learner you are certainly going to be documenting or dictating almost right away, but remember this post when you are more senior. It is always tempting to think that you would do something later and push it off till you have more time - but this is an illusion. Contemporaneous charting is something that you should always strive for, and it is also highly recommended by the CMPA.



