You are a Nurse Practitioner who has educated yourself about Canada’s digital divide through personal research and interactions with your own patients. Now that you have a grasp on the source of the problem, you begin to search for solutions. You scour the internet for various services that will provide your patients with access to devices, internet services, and provide technology teachings.
Welcome to Part 2 of our Virtual Care and Equity series of HiQuiPs! In our last post, we discussed the digital divide, the patient populations most affected, and the main challenges contributing to the digital divide. In this post, we delve deeper into the available community supports and possible solutions that we must advocate for to help our patients close the gap.
What can be done?
Firstly, healthcare providers should evaluate each patient’s situation, particularly when conducting visits with patients who are frail and/or elderly, patients for whom there is a language barrier, and those with mental health concerns. For patients where there may be discomfort with telemedicine, an initial phone consult should be performed to determine if a virtual visit is necessary or suitable. During this consult, patients can be asked about devices they have, internet availability and efficacy, comfort with technology use, availability of a caregiver to assist, availability of a private environment, and the patient’s preference of visit modality.1 Patients can also be counselled on the purpose, safety, and efficacy of virtual visits.1 St. Joseph’s Hospital in London, ON released guidelines from their South West Frail Senior Strategy which provides comprehensive questions to ask patients regarding technology and sample scripts to use when explaining telemedicine.
For patients who are onboarded for virtual visits, paper instructions surrounding use of a device, applications, and the correct environment for the visit in the patient’s language of choice can be provided.1 Patients should also be provided with a list of telephone numbers to call for technical support.1 If possible and with the patient’s consent, healthcare providers should also reach out to the patient’s caregivers to inquire whether they can assist with the virtual visit. For patients without caregiver support, particularly the frail elderly, inquiries within the hospital system should be made to refer the patient to a specific health team or health consultant who engages in setting up technology. For example, at Mount Sinai Hospital in Toronto, there is a Telemedicine Program for Homebound Elders. This program is facilitated by a Geriatrics Clinical Nurse Specialist (GCNS). During a typical appointment, the GCNS arrives at the patient’s home to perform a history and physical exam, and to go through medication changes14. The GCNS the connects the patient with the physician using Ontario Telemedicine Network videoconferencing software to conduct the virtual visit14. In the US, some health consultants such as Oak Street Health run a program where they send drivers to deliver cellular-enabled tablets to patients15. The drivers log patients onto the video visit and afterwards, pick up the tablets, clean them, and deliver them to other patients15. Oak Street Health and other US health consultant firms such as Iora Health and Landmark also offer to set up clients with their video app and perform practice visits, where admin staff conduct mock video visits with patients a few days prior to their first virtual appointment15.
For patients who cannot be onboarded, a phone call and/or in-person visit should be offered.
With regards to problems accessing devices and internet due to cost, there are multiple programs offered by non-profits, hospitals, and the Canadian government that we can refer our patients to. There are also many organizations which provide teaching for those struggling with digital literacy. For example, reBOOT Canada provides computer equipment, training, and technical support to people with limited access to technology. There is also the PHONE-CONNECT program, an initiative started by emergency physicians at University Health Network (UHN), which provides used, donated phones to patients who are homeless, struggling with mental health or substance use, and socially isolated. This program has expanded to include Unity Health Toronto in collaboration with UHN. Rogers and Telus also have programs to provide internet service for $10/ month for certain eligible Canadians. There are many organizations funded by the Canadian government which provide teaching to improve digital literacy. Please see Table 1 for an extensive list.
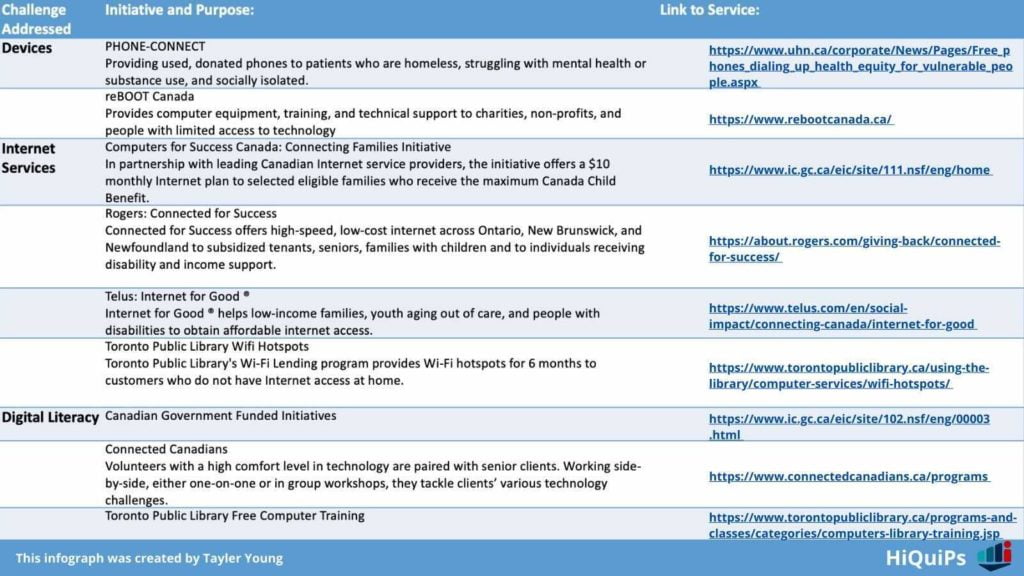
Another avenue to explore is to connect with certain organizations at a hospital level. For example, Toronto Public Library offers free internet in public libraries and have a Wi-Fi hotspot lending program. By partnering with them and supplementing their resources, healthcare providers can provide better access points to the low-income and homeless populations. Similar partnerships formed with outpatient services/ shelters could help their populations find an easier pathway to virtual care and connectivity. In terms of advocacy, we must advocate locally within our own hospital systems to offer programs such as Mount Sinai’s Telemedicine Program for Elders, Oak Street Health’s tablet delivery system, or Oak Street Health and Iora Health’s practice visit system. On a provincial and national level, we must push the government to improve internet infrastructure for sufficient broadband access in rural, remote, and First Nations communities.
With respect to virtual care, we cannot just have a level playing field for access. We need to provide easier, more meaningful access, if we truly want success in our vulnerable populations.
You create handouts in multiple languages for your patients being onboarded for virtual visits. You also produce a list of organizations that offer access to devices, internet services, and technology teachings. You share these resources with your local hospitals. Your colleagues in the Emergency Department are inspired and look to pair with UHN’s PHONE-CONNECT team to start the initiative in their own hospital. That’s it for our 2-part series on digital inequity in healthcare. We hope this series has given you a toolkit to help support your patients. Let us know what you think on Twitter at @Hi_Qui_Ps. If there is anything specific you would like to learn about, e-mail us at [email protected]. There is more content to come on #HI and Digital health!
Senior editor: Ahmed Taher (@ak_taher)
This post was copyedited by Tayler Young (@Tay1erYoung)
- Providing Geriatric Virtual Care across the South West: Guidance Document for Health Care and Community Support Services Providers. London https://www.sjhc.london.on.ca/media/8411/download.
- Telemedicine Program for Homebound Elders. https://sinaigeriatrics.ca/services/mount-sinai-2/telemedicine-program-for-homebound-elders/. Published 2020. Accessed July 8, 2021.
- Ikram U, Gallani S, Figueroa JF, Feeley TW. 4 Strategies to Make Telehealth Work for Elderly Patients. Harv Bus Rev. November 2020. https://hbr.org/2020/11/4-strategies-to-make-telehealth-work-for-elderly-patients.



