You have just finished a busy ED shift on a warm summer evening and feel that you have been able to help a lot of people today. You plan to visit a patio and relax as you have earned it! On your way out you overhear a patient and their family members saying that they came to this ED because they heard it was “the best”, and they would never go back to the other ED as the care isn’t as good. You think about this on your scenic drive to the patio and wonder why the patient thinks your ED is “the best”? How is “the best” being measured? Who makes that determination? And how can EDs in general have good quality? You think about elements like the ED size, how many patients are being seen, the rate at which they are seen, and how satisfied they are. Your mind wanders about many different elements, but how do you reconcile them? And where is a good starting point?
Welcome to our new HiQuiPs series, where we will cover a wide array of topics within the intertwined fields of Health Informatics, Quality Improvement, and Patient Safety as they relate to emergency medicine. Quality of care is an integral starting point to our discussions. A previous two-part CanadiEM Quality Improvement series sought to define quality in healthcare, quality improvement and introduce some basic approaches.12 They discussed the classical definition from the landmark Institute of Medicine report which includes six domains that define quality of care which are safe, effective, patient-centered, timely, efficient, and equitable.3
These are broad categories, but how do they translate to a practical assessment of the current quality of care in your ED and apply them to improvement initiatives? When you are driving your car you need to know how it’s performing – what the gas level is, how fast you’re going, indicators for your temperature, and oil, etc. But there are so many different elements pertaining to the ED that you can think of on your drive. So the first step is how to organize them.
Frameworks to Think About Healthcare Quality
When reading about quality measures, many terms often appear like benchmarking, indicators, and targets. Figure 1 provides a helpful framework that helps organizes some commonly used terms:

Figure 1. Commonly Used Terms for Healthcare Quality. Reproduced from Cameron et al.4
One of the most widely used frameworks to organize quality measures is the Donabedian model, which classifies measures into the three categories: structural, process, and outcome measures.5
Why is it important to know about this model? Well, it will frame how you think about quality and help communicate with others. Structural measures are the easiest to measure and reflect the capacity of the system. Process measures are reflections of different elements of the continuum of care, and may coincide with guidelines or recommendations of care.6 Outcome measures reflect the impact of care on patients. These are more difficult to measure at times, but reflect what is ultimately intended by the provision of care. Another category of measures that is often included in quality frameworks are balancing measures, which reflect the unintended consequences of changing the system.7 A summary with examples is presented below:
| Framework for Quality Improvement Measures | ||
| Measures | Definition | Examples |
| Structural Measures | The capacity of the system | Number of ED beds; number of nurses, porters, or physicians on shift. |
| Process Measures | What is done along the continuum of care | Time to be seen by ED physician; percentage of patients receiving meal trays; length of time until consultant calls back. |
| Outcome Measures | The impact of the care or intervention | Patient reported outcomes; number of unscheduled return visits. |
| Balancing Measures | Unintended consequences | Cost changes with intervention; impact on other patients; impact on other services. |
On the next shift after meeting your friends on that patio, you see a patient that is critically ill with acute respiratory distress. After you intubate and stabilize them, the transfer to the ICU team takes much longer than expected. You return often to re-assess and continue to manage the care of this patient. You believe that this takes away from your ability to care for other patients effectively during your shift. You wonder about the quality of care this patient experienced as well as the other patients during your shift. You wonder what quality measures are being collected by your department.
There are numerous methods to collect data on quality. They vary in terms of scope and labour intensiveness as they pertain to different needs. Figure 2 is a summary of a variety of methods that can be used to collect quality data. Having a routine and standard way of quality data collection is essential to understanding the quality of care in your ED.
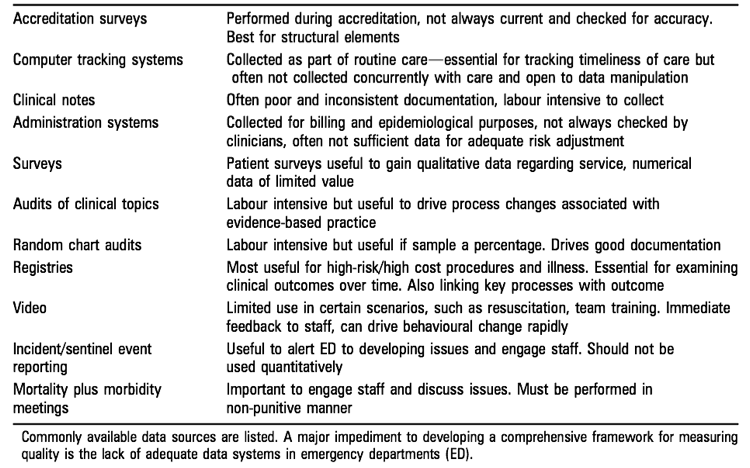
Figure 2. Methods of Data Collection for Healthcare Quality. Reproduced from Cameron et al.4
Emergency Department Quality Measures
Over the past decade, there has been an increasing role of ED quality data collection and public reporting across North America. Given the numerous options in quality measures, efforts have been made to standardize them. This would enable increased adoption, use, benchmarking, comparisons, and public reporting. Currently, there are two consensus-driven approaches for ED quality measures.
The first was published in a Canadian consensus paper, with a set of 48 indicators across nine categories: patient satisfaction, ED operations, patient safety, pain management, pediatrics, cardiac conditions, respiratory conditions, stroke, and sepsis or infection.8 The highest ranked measures in each category are shown in Figure 3:

Figure 3. Top Priority Indicators as ranked by a Canadian Consensus Panel. Reproduced by Schull et al.8
The second approach arose from the proceedings of the 2014 Emergency Department Benchmarking Alliance Consensus Summit with indicators across several categories: ED operational characteristics, hospital operational characteristics, timestamps and time intervals, proportion metrics and readmission measures, as well as ED utilization and staffing units.9 There are also many notable healthcare organizations which focus on healthcare quality which can be helpful if you are going more in depth.4
Regardless of the approach, there are evidence-based consensus driven measures that can be utilized. Maybe now you wonder about which ones are being used in your ED and how they are being used? Or how many are used locally and how many are reported to the Ministry of Health?
Now you are equipped with a basic approach to understanding healthcare quality measures and how they apply to the ED. With this new lens, you are eager to get started on a local quality improvement project in your ED. Now you just have to choose a project!
As you prepare for your QI project, you wonder where to get more information. Stay tuned for our next HiQuiPs monthly post, as we start a three-part series called: QI in the ED – Preparation, where we will cover general considerations, stakeholder engagement, elements of behaviour change, root cause analyses and much more!
This post was copyedited by Paula Sneath