You are attending a departmental event when you walk over to a group of your colleagues, and the conversation goes silent. You wonder if you had that effect on the conversation, but the awkward silence is reluctantly broken by the person who was speaking when they quietly continue their story. This veteran physician discusses a recent incident where they placed a wrong-sized lumen chest tube in a patient, only to have to replace it afterwards. In what seems to be a sign of moral support, a veteran nurse shares a story where they gave the wrong patient medication. This opens the door to many more people sharing their own incidents that occured recently.
You walk away thinking about how secretive this conversation was, and wonder why these patient safety incidents aren’t being shared with the entire group so that others learn from them, and that the system and processes that led to these incidents can be improved such that these patient safety incidents can be mitigated in the future.
Welcome back to our third post on patient safety in the ED. In the first two parts of the series, we introduced the systems approach to patient safety. In this post, we discuss the role that ED culture has in supporting (or hindering) patient safety.
What is the patient safety culture?
Patient safety culture is a component of organizational culture that “includes the shared beliefs, attitudes, values, norms and behavioural characteristics of employees, and influences staff member attitudes and behaviours in relation to their organization’s ongoing patient safety performance”.1 While it may be difficult to completely separate ED patient safety culture from the overarching organizational culture, different clinical units may have differences in their subcultures, which provide opportunities for local improvement and leading by example.
Why is it important?
An improved patient safety culture has been associated with reduced patient harm2,3 a perception of better care by patients and family members, and reduced staff burnout. Front line staff in ‘safe’ environment are more likely to report errors.4,5,6,7 Overall, creating this type of culture enhances the work environment and shape staff perceptions about ‘normal’ behaviour related to patient safety in their work area.8 All in all, it is a big deal!
How do you measure your patient safety culture?
A number of surveys have been designed to assess the patient safety culture in healthcare that may be applicable for use in the ED.9,10
One example is the Safety Attitudes Questionnaire:9
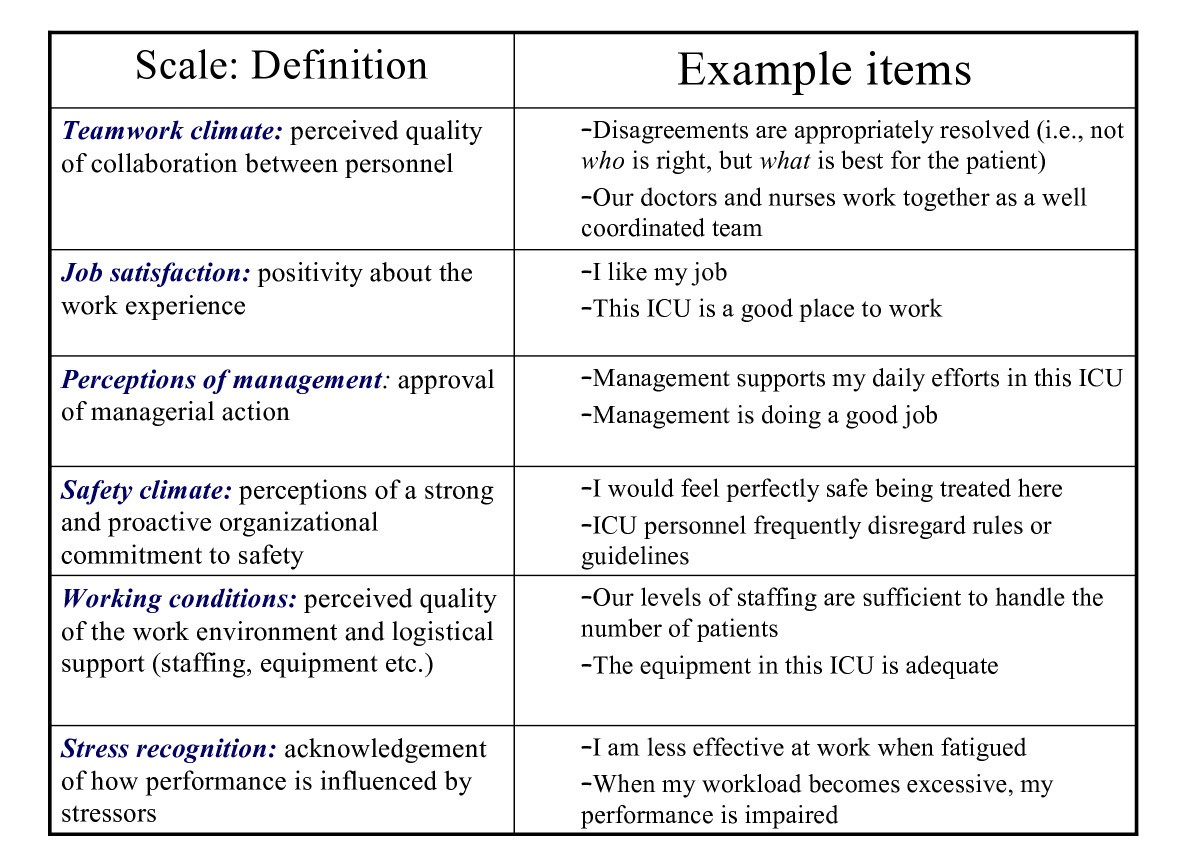
Figure 1. Adapted from The Safety Attitudes Questionnaire. The 6 components of the Safety Attitudes Questionnaire.
The key point in utilizing these questionnaires is that stakeholder engagement, particularly front-line staff, is important in identifying the barriers that exist and key opportunities for improvement in an organization’s safety culture.
How to promote patient safety culture in the ED
Most studies on interventions promoting a patient safety culture were multi-component interventions.8 These included team training activities, executive walk arounds, or the use of evidence based culture change toolkits.11
The Canadian Patient Safety Institute recommends that a comprehensive strategy to promote patient safety culture includes the following:12
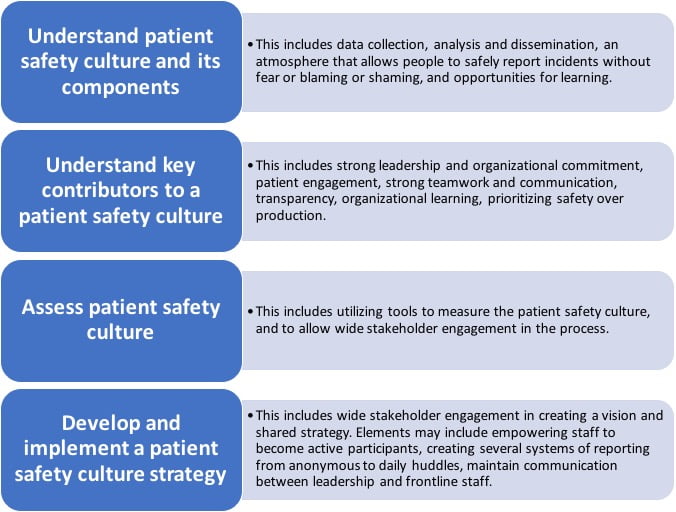
Therefore, an ED culture that promotes patient safety is built on transparency, empowered frontline staff, a non-blaming environment, an organizational learning culture, and invested leadership. Developing this culture requires wide stakeholder engagement and interprofessional collaboration with the patient at the forefront. How is the culture in your institution? Are front line staff empowered to report incidents, and do others learn from them? Is there regular sharing of this information?
In summary, the patient safety programs need to be embedded in health culture that supports them. Patient safety cultures have been shown to have beneficial effects on patients, frontline staff, and the organization. Moreover, there are evidence based strategies to measure and to optimize the patient safety culture.
Now that you have been empowered with this information, you are able to discuss this at your next ED business meeting and slowly start to create a safer environment where staff are reporting, learning, and improving patient safety. Stay tuned to our next post where we dive deeper into one aspect of patient safety and discuss the risky business of patient handovers.
This post was copyedited by Jung-In Choi.
**UPDATE (November 2020): The HiQuiPs Team is looking for your feedback! Please take 1 minute to answer these three questions – we appreciate the support!**