This updated episode of CRACKCast covers Rosen’s Chapter 28 (9th Ed.) on diarrhea. With this review, we hope to provide you a systematic approach to this explosive clinical presentation!
Shownotes – PDF Here
[bg_faq_start]Rosen’s in Perspective
Alright, everyone. It is the episode you have all been waiting for. Today’s episode covers Chapter 28 in Rosen’s 9th Edition – Diarrhea. And while some of you may be wanting to learn about anything else at this moment, don’t hit pause just yet. Along with being one of the leading causes of childhood death in developing countries, diarrheal illnesses comprise a significant cause of morbidity and mortality here at home. In the United States alone, there are approximately 179 million cases of acute diarrhea every year, accounting for 900,000 hospitalizations. C.difficile infection accounts for a growing number of these cases (largely because of increasing exposure to antibiotics), and is one of the most common causes of fatal diarrhea. Alone, this pesky pathogen directly costs the US healthcare system $3.4 million USD per year and ultimately leads to the death of many of our most vulnerable persons. Thus, while learning about this foul topic may be uncomfortable, knowing how to appropriately evaluate, diagnose, and treat patients with diarrhea in the ED is of the utmost importance.
Along with a heavy helping of humour, we will be giving you the essential information you need to treat your next patient with a case of the loosies. We will first jump in by defining diarrhea and the manner in which cases are typically defined. We will review the relevant pathophysiology you will need to understand to inform further investigation and treatment strategies for the patient on the commode in bed 4. As per usual, we will review an extensive differential, approach to investigation, and management strategy for the patient with a case of the Wet Taco Bell Tuesdays, giving you all of the exam ammunition you need to increase your chances of getting your golden ticket to staffhood. Last, we will hit you with the high yield on-shift wisecrack trivia that you have come to know and love. So, sit back, push that coffee to the side, and enjoy!
[bg_faq_end]Core Questions:
[bg_faq_start][1] Define diarrhea
As per Rosen’s 9th Edition, diarrhea is defined as “a change in normal bowel movements with passage of three or more stools per day or at least 200g of stool per day”
Typically, diarrhea is further classified based on the time course.
- Acute Diarrhea
- Occurs over a span of 1-14 days
- Persistent Diarrhea
- Occurs for a total duration of 14-30 days
- Chronic Diarrhea
- Occurs over a span of 30 days or longer
[2] Outline the pathophysiologic processes that result in diarrhea
There are four pathophysiologic mechanisms that can cause diarrhea. These are:
- Secretory Diarrhea
- This is the most common type of diarrhea seen in the ED, as most cases of infectious diarrhea is secretory in nature
- In cases of infectious secretory diarrhea, pathogens produce toxins that increase GI cellular permeability leading to secretion of water and electrolytes into the bowel lumen
- Other causes of secretory diarrhea that are not infectious in nature include:
- Medication-induced diarrhea
- Endocrinopathy-induced diarrhea
- Neoplastic diarrhea
- Osmotic Diarrhea
- Osmotic diarrhea occurs because the patient has ingested osmotically active solutes or has a malabsorption disorder that allows osmotically active molecules to draw water and electrolytes into the GI tract
- Inflammatory Diarrhea
- Cellular damage of the intestinal mucosa results in hypersecretion of water, blood, mucous, proteins, and electrolytes into the GI tract
- This type of diarrhea is caused by invasive bacteria or parasites OR by chemotherapy, radiation therapy, IBD, and other autoimmune disorders
- Dysmotility Diarrhea
- Usually a component of chronic diarrhea, but can contribute to acute cases
- Increased motility decreases the time over which GI luminal contents can be absorbed. This results in limited water and electrolyte reabsorption
[3] List 10 infectious causes of diarrhea – Box 28.1
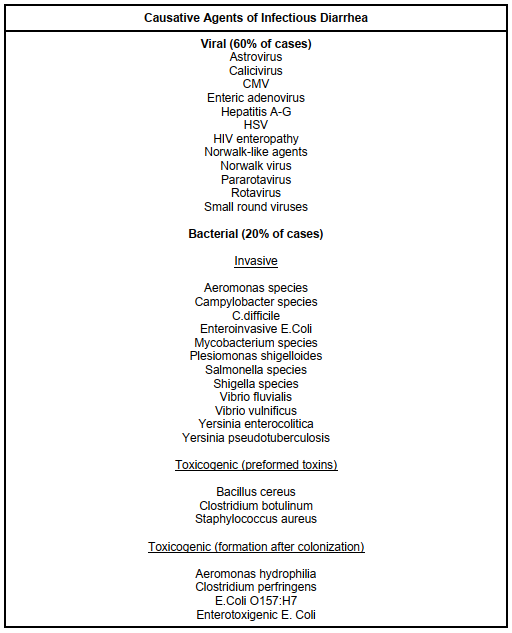
This figure was informed by Box 28.1 – Causative Agents of Infectious Diarrhea in Rosen’s 9th Edition. Refer to the text for further information.

[4] List 10 non-infectious causes of diarrhea – Box 28.2
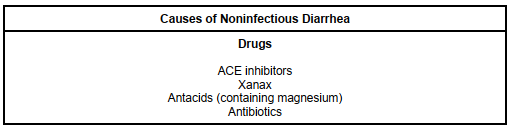
This figure was informed by Box 28.2 – Causes of Noninfectious Diarrhea in Rosen’s 9th Edition. Refer to the text for further information.


[5] Outline 5 important aspects of a patient’s history to elucidate in cases of diarrhea.
As you could probably predict given the laundry list of diagnoses aforementioned, you need to be systematic when taking the history of a patient with diarrhea. You must ask about the duration of symptoms, volume/frequency/consistency of stools, presence of bloody stools, inability to tolerate PO intake, and accompanying symptoms. Additionally, taking a detailed social history and sexual history is important. There are several aspects that are essential to elucidate that you may not think to ask every day. These are:
- Travel history
- Immunization history
- Recent antibiotic use
- Recent hospitalizations
- Sick contacts
[6] Detail an approach to laboratory testing in the patient with diarrhea
Major key point alert: MOST CASES OF ACUTE DIARRHEA require minimal laboratory and diagnostic testing. That being said, some cases of the trots do require you to know a thing or two about the diagnostic evaluation of diarrhea.
First, when do we test? Well, the degree to which you test largely depends on the following factors:
- Clinical severity of illness
- Presence of vital sign derangements
- Presence of comorbidities
- Presence of physical exam findings suggesting serious intraabdominal pathology
- Diarrhea occurring in the presence of serious systemic illness
Now that we know when to test, what tests should you order? This is in no way a complete list, but consider the following investigations when your pen meets the page:
- CBC
- Remember that leukemoid reactions are not sensitive or specific for identifying serious pathologies
- Eosinophilia may hint at parasitic infections with an extra-intestinal migration phase
- HgB/platelet levels can screen for anemia either secondary to blood loss or hemolysis
- Coagulation Profile
- May identify a coagulopathy that is leading to GI bleeding and subsequent diarrhea
- Electrolyte/Renal Panel
- Identify pre-renal AKI and electrolyte abnormalities that need to be corrected
- Liver Enzymes/Function Testing
- May elucidate patients with diarrhea secondary to hepatic dysfunction
- VBG with lactate
- Can identify acid/base disturbances associated with diarrheal illnesses and elucidate the degree of perfusion deficit in patients with severe illness
- Lipase
- Rarely indicated, but can be ordered in cases of diarrhea with severe epigastric pain/tenderness accompanied by vomiting
There are some special tests to consider in patients with diarrheal illnesses. We have provided some information on them below:
- Hemoccult and Fecal Cell Count
- Not useful, as they are not sensitive or specific for certain diseases and do not identify those in need of antimicrobial therapy
- Fecal Calprotectin and Lactoferrin
- Not indicated in the context of the ED; not sensitive or specific for identifying acute bacterial diarrhea
- C.difficile Toxin Assays
- Indicated if patients are immunocompromised, have a history of recent antibiotic use, reside in a nursing home, are employed in a healthcare setting, or if they have significant diarrhea (>/6 stools per day) for several days
- E.coli O157:H7 Toxin Assay
- Indicated when there is a known outbreak or if the patient presents in an endemic area
- Can also consider if the patient has suspected HUS
- Stool Culture for Bacteria
- Rarely useful in the ED setting as they are insensitive and take too long to process
- Indicated in patients who are admitted to hospital with a toxic appearance, in those who are immunocompromised, or those patients with advanced age
- Also indicated in patients with persistent or chronic diarrhea that has not been previously tested for these pathogens
- Stool Ova & Parasite Examination
- Generally not indicated in the ED
- May be useful in patients with chronic diarrhea, as they can demonstrate infection with E.hystolytica, Giardia, and Cryptosporidium
- Consider ordering in patients with a history of:
- Travel two or immigration from endemic countries
- Patients with exposure to infants in daycare settings
- Patients with HIV infection
- Giardia Antigen Assay and Serologic Testing for Amebiasis
- Indicated in patients who:
- Are exposed to poor sanitation
- Are immunocompromised
- Have a history of travel to developing countries
- Have a history of recent camping with ingestion of stream or spring water
- Have a history of those with daycare exposure
- Indicated in patients who:
[7] When are empiric antibiotics indicated for the treatment of diarrheal illnesses?
- Severe disease (fever, >6 stools per day, volume depletion warranting hospitalization)
- Features suggestive of invasive bacterial diarrhea (e.g., bloody or mucoid stools) except if features of non-severe disease and either afebrile or minimally febrile
- Host factors that increase the risk for complications, including age >70, comorbidities such as immunocompromised states and cardiac disease
Wisecracks:
[bg_faq_start][1] What antibiotics are most commonly implicated with precipitating C.difficile diarrhea
Answer:
While all antibiotics can precipitate C.difficile diarrhea, the three most commonly-implicated antibiotics are:
- Cephalosporins
- Penicillins
- Clindamycin
[2] What factors on history increase the probability of non-benign diarrheal illness
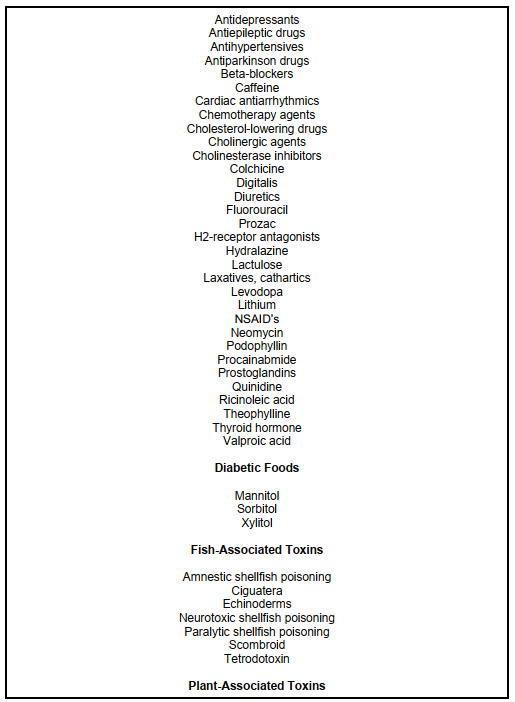
This figure was informed by Table 28.1 – Factors Increasing Probability of Non-Benign Diarrhea in Rosen’s 9th Edition. Refer to the text for further information.


[3] Outline the constituent ingredients contained within the World Health Organization’s rehydration formula.
Answer:
- 3.5 grams of sodium chloride
- 2.9 grams of trisodium citrate or 2.5 grams of sodium bicarbonate
- 1.5 grams of potassium chloride
- 20 grams or glucose or 40 grams of sucrose
[4] What is the BRAT diet and why is it recommended in patients with acute diarrheal illnesses?
Answer:
The BRAT diet (bananas, rice, apples, toast) is a diet recommended for patients who have resumed oral intake after an episode of diarrhea. It is beneficial as it is constipating (bananas, apple peels) and non-stimulating.
[bg_faq_end]Uploaded and copyedited by Osama Rehman



