This updated episode of CRACKCast covers Rosen’s Chapter 24 (9th Ed.), and while it may not be the most glamorous topic, abdominal pain is both common and potentially life-threatening. In this episode we hope to solidify an approach to your next patient’s gut ache.
Shownotes – PDF Here
[bg_faq_start]Rosen’s in Perspective
Alright, everyone. It is time for yet another cruise down Rosen’s lane. Today, we are covering one of the most important chapters that review core EM content – Chapter 24 – Abdominal Pain. While the chapter itself is not as exciting as others, it no doubt provides you with the information you need to skillfully navigate your next patient encounter with someone complaining of the ol’ angry gut syndrome.
Abdominal pain, as many of you well know, is one of the most common presenting complaints for patients in the ED. And while individuals often come looking for answers, many (approximately 40%) will never have a definitive pathology identified. While it may be easy to falsely conflate this relatively high number of unsolved medical mysteries with notions that abdominal pain is not a serious complaint, do not fall into that trap. Those achy innards often fool ED clinicians, so it is best to approach each case systematically. Today’s episode will review the extensive differential for this complaint, detail the risk factors that increase the likelihood of a patient harbouring a sinister pathology, explain common pitfalls that should be avoided when investigating patients with abdominal pain, and present an approach to the acute stabilization and management for this patient population. It may sound like a lot, but we will make sure your journey with us today is as helpful as possible – so sit back, turn up the volume and enjoy the ride!
[bg_faq_end]Core Questions:
[bg_faq_start][1] What are risk factors for serious underlying causes of abdominal pain? (Box 24.1)
This list was adapted from Box 24.1 in Rosen’s 9th Edition. Please see the textbook for the accompanying images.

[2] Explain key symptoms and signs to look for in the evaluation of the patient with abdominal pain.
Ask about onset, location, radiation, timing, triggers etc. Plus fevers, urinary symptoms, N/V or hematemesis, bowel habit/bloody stools and LMP/pregnancy status/sexual history in females.
Some classic descriptions are as follows:
- Diffuse, severe pain and severe nausea in bowel obstruction
- Pain “out of proportion” in mesenteric ischemia
- Radiation from epigastrium to midback accompanied by severe N/V in pancreatitis
- Radiation to left shoulder with splenic pathology, diaphragmatic irritation, or free fluid
- Onset of pain with syncope in ruptured AAA or ectopic
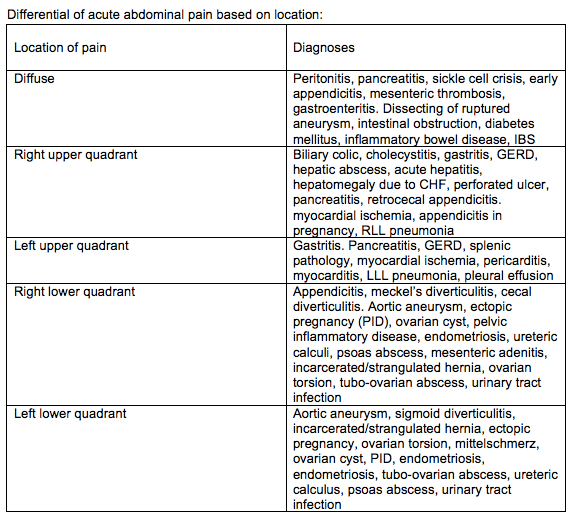
[3] What diagnoses are associated with different regions of abdominal pain? (Fig 24.1)
This table was adapted from figure 24.1 in Rosen’s 9th Edition. Please see the textbook for the accompanying images.
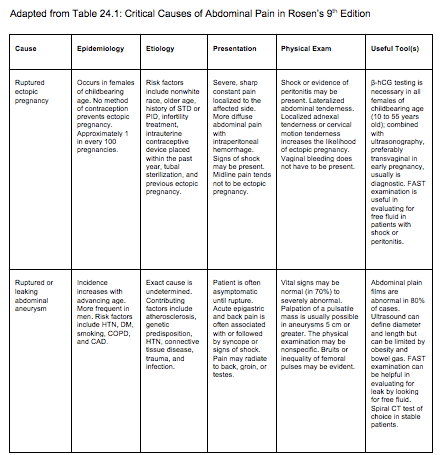
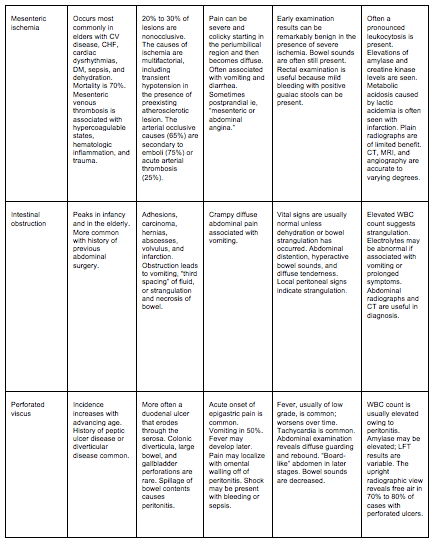
[4] List 5 critical and 5 emergent causes of abdominal pain (Table 24.1, 24.2)



[5] Explain an approach to ancillary testing in abdominal pain.
Labs – UA and BHCG among highest yield tests
CBC – WBC is nonspecific
Lipase, Liver enzymes, and coags – helpful in small proportion
X-ray – free air or obstruction
US – biliary or pelvic pathology
CT – pretty much everything else
Endoscopy – GI bleeds or ?PUD, ?IBD
[6] Outline a diagnostic algorithm for patients with abdominal pain (Fig 24.4)
Adapted from Fig 24.4 in Rosen’s 9th edition please refer to original source for complete figure

[7] Outline a management algorithm for patients with abdominal pain (Fig 24.5)
Adapted from Fig 24.5 in Rosen’s 9th edition please refer to original source for further clarification

Remember to resuscitate and provide analgesia quickly when it is indicated! Don’t spend a bunch of time on your H&P before looking after your patients immediate needs.
[bg_faq_end]Wisecracks:
[bg_faq_start][1] What are the structures included in the foregut, midgut, and hindgut? More importantly, why do you care?
Visceral pain is perceived from the abdominal region that corresponds with the embryonic somatic segment.
- Foregut: stomach, duodenum, liver, GB, pancreas = Epigastric abdominal pain (T7-T9)
- Midgut: small bowel, proximal ⅔ colon, and appendix associated with periumbilical pain (T9-T11)
- Hindgut structures (distal ⅓ colon, descending colon, sigmoid colon, upper anal canal) associated with lower abdominal pain (T11-L1)\
Basically – you need to have a working knowledge of abdominal anatomy to accurately diagnose your patient’s abdominal pain.
[2] List indications for bedside US in the ED patient with abdominal pain. (Table 24.3)

[3] Explain how referred pain works in the setting of abdo pain. (Fig 24.2)
Referred pain = pain felt remotely from its source because peripheral afferent nerve fibers from many organs enter the spinal cord through nerve roots that have somatic afferents from other parts of the body. The short version is that the brain is not very good at interpreting pain signals coming from the viscera and misinterprets them as coming from the associated somatic regions. Thus – upper abdominal structures can refer pain to the chest, and lower structures can refer pain to the hips/retroperitoneum. Some other examples include epigastric pain and inferior MI, shoulder pain with diaphragmatic irritation, and a lower lobe PNA causing referred abdominal pain.
[bg_faq_end]Uploaded and copyedited by Ryan Fyfe-Brown