This updated episode of CRACKCast covers Rosen Chapter 23 (9th Ed.), one of the quintessential topics of Emergency Medicine, chest pain. Here the crew delivers an organized approach to ensure you’re not missing any important pathology on your next shift.
Shownotes – PDF here
[bg_faq_start]Rosen’s in Perspective
Chest pain is a very common ED complaint, comprising approximately 9% of visits in the US. Chest pain is also a relatively higher risk complaint – the causes can be anything from several life-threatening diagnoses, to completely benign etiologies. We are going to give you a solid approach to chest pain, so that when your next shift that seems to be a conveyor belt of CTAS 2 chest pains registering q15min, you will be well prepared!
[bg_faq_end]Core Questions:
[bg_faq_start][1] Describe an approach to key history and physical exam for chest pain patients presenting to the ED.
This figure is adapted from Table 23.2 in Rosen’s 9th Edition. Please see the text for further details and explanation of information contained within.

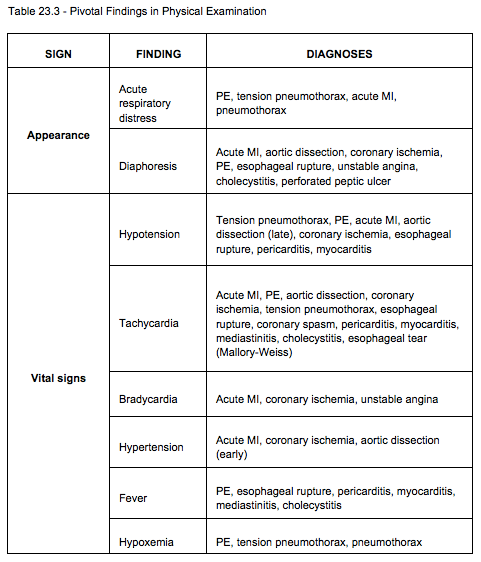
This figure is adapted from Table 23.3 in Rosen’s 9th Edition. Please see the text for further details and explanation of information contained within.


Practically – our general chest pain history screens for:
- Infectious symptoms (Fever/Chills/URTI/Cough/Sputum)
- CHF sx and dyspnea (orthopnea, PND, SOBOE, leg swelling)
- Sx suggestive of ACS and Dissection
- PE risk factors (to calculate a wells score if needed)
- GI sx, N/V, GER (reflux, biliary disease or other abdominal causes)
- Palpitations or syncope
- Don’t forget to ask about cocaine or other stimulants
[2] List 5 critical diagnoses, 5 emergent, and 5 nonemergent diagnoses to consider in the patient presenting with chest pain.
This figure is adapted from Table 23.1 in Rosen’s 9th Edition. Please see the text for further details and explanation of information contained within.


[3] Describe an approach to the critically ill patient with undifferentiated chest pain.

[4] Describe an approach to ancillary testing in chest pain.
Alright, all. Remember, the highest yield diagnostic tests to order in the patient with chest pain are an EKG (should be obtained within 10 minutes of arrival) and a chest radiograph. There are a few others that Owen and I typically order when we encounter these patients in the ED. These are:
- Typically obtain:
- EKG
- CXR
- Bedside lung and cardiac ultrasound
- Bilateral arm BP’s
- CBC + Chem 7
- Cardiac biomarkers (consider risk factors when ordering these)
- Consider obtain:
- Bedside abdominal ultrasound
- Liver enzymes + function tests
- Lipase
- VBG with lactate
- ABG to calculate Aa gradient
- D-dimer
- B-HCG (quantitative)
- Urinalysis +/- culture and sensitivity
- CT Aortogram
- CT PE
As this is a Rosen’s podcast, we would be remiss if we didn’t include the wealth of tables included in the chapter. There are two y’all should know about.
This figure is adapted from Table 23.4 in Rosen’s 9th Edition. Please see the text for further details and explanation of information contained within.

This figure is adapted from Table 23.5 in Rosen’s 9th Edition. Please see the text for further details and explanation of information contained within.

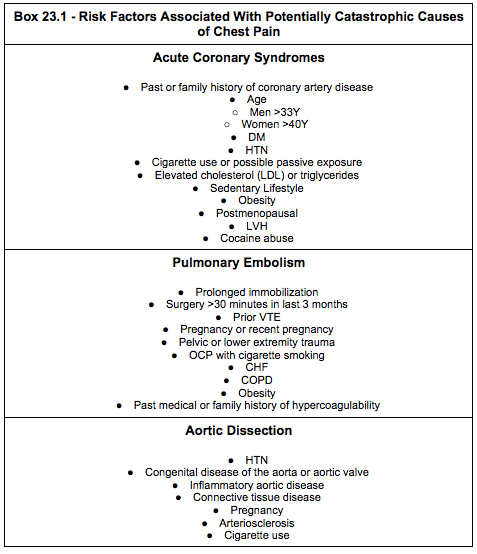
[5] List the risk factors associated with each critical chest pain diagnosis. (Box 23.1)
This figure is adapted from Box 23.1 in Rosen’s 9th Edition. Please see the text for further details and explanation of information contained within.

[6] Explain the approach to risk stratification of ED chest pain patients.
Alright, let’s talk about cardiac risk stratification. There has been quite a bit of literature published in this area over the last several years, so we will present you with the two scores most commonly used. These three scores have been validated externally, so they should help you out in the ED and aid in your conversations with your friendly neighborhood Cardiologist.
So, there are three scores typically spoken of in the literature when risk stratifying patients with query cardiac chest pain. These are:
- GRACE Score
- TIMI Score
- HEART Score
GRACE Score (Global Registry of Acute Coronary Events Score – 6 month admission-mortality):
(Complex method of calculation)
- Age
- HR
- SBP
- Creatinine
- Cardiac arrest at admission
- ST segment deviation on EKG?
- Abnormal cardiac enzymes?
- Killip class (signs/symptoms)
- No CHF
- Rales and/or JVD
- Pulmonary edema
- Cardiogenic shock
Interpretation:

TIMI Score (Thrombolysis in Myocardial Infarction Score – 14 day risk stratification of mortality, MI, or need for revascularization):
- Age >/65 (0 or +1)
- >/3 CAD risk factors (0 or +1)
- HTN
- Hypercholesterolemia
- DM
- FMHx CAD
- Current Smoker
- Known CAD (0 or + 1)
- Stenosis >/50%
- ASA use in past 7 days (0 or +1)
- Severe angina (0 or +1)
- >/2 episodes in 24 hours
- EKG ST changes >/0.5 mm (0 or +1)
- Positive cardiac marker (0 or +1)
Interpretation:
- 0 – 5% mortality, MI, or need for revascularization
- 1- 5% mortality, MI, or need for revascularization
- 2- 8% mortality, MI, or need for revascularization
- 3- 13% mortality, MI, or need for revascularization
- 4- 20% mortality, MI, or need for revascularization
- 5- 26% mortality, MI, or need for revascularization
- 6- 41% mortality, MI, or need for revascularization
HEART Score (History, EKG, Age, Risk Factors, Troponin Score – 6 week risk of MACE):
- History
- 0 – slightly suspicion
- +1 – moderately suspicious
- +2 – highly suspicious
- EKG
- 0 – normal
- +1 – nonspecific repolarization disturbance (no ST deviation but LBBB, LVH, or repolarization changes (e.g., digoxin effect)
- +2 – significant ST deviation (ST deviation not due to LBB, LVH or digoxin effect)
- Age
- 0 – <45 Y
- +1 – 45-64Y
- +2 – >/65
- Risk Factors
- Includes HTN, hypercholesterolemia, DM, obesity (BMI >30), smoking (current or cessation </3 months), positive family history in parent or sibling with CAD before age 65), atherosclerotic disease, prior MI, prior PCI/CABG, Hx CVA/TIA/PAD
- 0 – no known risk factors
- +1 – 1 to 2 risk factors
- +2 – >/3 risk factors or history of atherosclerotic disease
- Troponin
- 0 – </normal limit
- +1 – 1-3x normal limit
- +2 – >3 x normal limit
Interpretation:
- Score of 0-3 – low risk – 0.9-1.7% risk of MACE – discharge home with PRN follow up with family physician; if high-sensitivity troponin used, no need for 3 hour repeat
- Score of 4-6 – moderate risk – 12-16.6% risk of MACE – inpatient or outpatient investigations by Cardiology
- Score of >/7 – high risk – 50-65% risk of MACE – urgent Cardiology consultation for inpatient evaluation
These scores help predict the probability of major adverse cardiac events (MACE) in a predefined period. These three scores have been compared head-to-head in multiple studies, the most recent of which was published in March 2020 in the Journal of the American College of Cardiology (JACC) (https://www.onlinejacc.org/content/75/11_Supplement_1/195).
By-and-large, most of these studies identify the HEART Score as the superior risk stratification system for ED patients. So, use it where appropriate.
[bg_faq_end]WiseCracks:
[bg_faq_start][1] What are the X-ray findings of aortic dissection?
Alright, tight list here for you all:
- Normal in 12%
- Wide mediastinum (61%)
- Double density appearance of the aorta
- Aortic knob obliterated
- Calcium displacement or double calcium sign
- Pleural effusion (L>R)
- Tracheal shift
- Left apical cap (curved density at lung apex)
- Deviated NGT
[2] What are your HR and BP targets in acute aortic dissection?
Use fentanyl and Esmolol/Labetalol as first line
Need to target HR <60 and SBP <120mmHg
If additional agents needed, can add nitroprusside and Nifedipine
Progression of dissection and mortality is proportional to flow velocity and pressure differentials (dP/dT).
- Our aim is to decrease HR, inotropy, and afterload.
Other management considerations:
- Large bore IVs
- If obtaining art line – right radial Art line, left arm NIBP
- Prepare for Rapid CTA
- Notify blood banks and start MTP if indicated
- Early consultation with CVSx indicated for Stanford type A
- If hypotensive – consider tamponade, MI, aortic insufficiency, or aortic rupture
[3] List the components of the HEART score.
HEART Score (History, EKG, Age, Risk Factors, Troponin Score – 6 week risk of MACE):
- History
- 0 – slightly suspicion
- +1 – moderately suspicious
- +2 – highly suspicious
- EKG
- 0 – normal
- +1 – nonspecific repolarization disturbance (no ST deviation but LBBB, LVH, or repolarization changes (e.g., digoxin effect)
- +2 – significant ST deviation (ST deviation not due to LBB, LVH or digoxin effect)
- Age
- 0 – <45 Y
- +1 – 45-64Y
- +2 – >/65
- Risk Factors
- Includes HTN, hypercholesterolemia, DM, obesity (BMI >30), smoking (current or cessation </3 months), positive family history in parent or sibling with CAD before age 65), atherosclerotic disease, prior MI, prior PCI/CABG, Hx CVA/TIA/PAD
- 0 – no known risk factors
- +1 – 1 to 2 risk factors
- +2 – >/3 risk factors or history of atherosclerotic disease
- Troponin
- 0 – </normal limit
- +1 – 1-3x normal limit
- +2 – >3 x normal limit
Interpretation:
- Score of 0-3 – low risk – 0.9-1.7% risk of MACE – discharge home with PRN follow up with family physician; if high-sensitivity troponin used, no need for 3 hour repeat
- Score of 4-6 – moderate risk – 12-16.6% risk of MACE – inpatient or outpatient investigations by Cardiology
- Score of >/7 – high risk – 50-65% risk of MACE – urgent Cardiology consultation for inpatient evaluation
Uploaded and copyedited by Ryan Fyfe-Brown



