In this episode the CRACKCast team reviews the approach for patients presenting with “shortness of breath”.
Core Questions
[bg_faq_start]
[1] Define the following terms:

[bg_faq_end]
[bg_faq_start]
[2] What anatomical structures are responsible for controlling respiratory effort?
The exact mechanisms that produce the sensation of breathlessness are not precisely known. However, we do know the structures responsible for controlling respiratory effort. These are detailed below.
Centrally:
- Respiratory centre located in the medulla oblongata and midbrain
- Most sensitive to alterations in the partial pressure of carbon dioxide in the brain
Peripherally:
- Thoracic Neural Receptors
- Slowly reacting receptors in the upper airway, trachea, lungs, chest wall, and pulmonary vessels
- Rapidly responding irritant receptors that respond to changes in lung volumes and the presence of substances such as histamine, prostaglandins, and noxious chemicals in the environment
- Chemoreceptors located in the carotid bodies
- Primarily respond to changes in the partial pressure of oxygen
- Chemoreceptors in the aortic bodies
- Primarily active during infancy and childhood, but largely become inactive during adulthood
- Mechanoreceptors in the diaphragm and skeletal muscles
[3] Outline an approach to the history for the dyspneic patient.
Features of Dyspnea:
- Duration
- Chronic or progressive dyspnea usually denotes primary cardiac or respiratory disease
- Acute episodes of breathlessness may result from asthma exacerbation, infection, intermittent cardiac dysfunction, psychogenic causes, or inhalation of allergens, foreign bodies or irritants
- Onset of Dyspnea
- Sudden onset should lead to consideration of PE or PTX
- Slowly building dyspnea may be the result of an acute exacerbation, COPD, pneumonia, small PE, CHF, or malignancy
- Provoking Factors of Dyspnea
- Position changes should be interrogated (think orthopnea, COPD, or neuromuscular disease)
- Interrogate potential PND by asking “do you wake up in the night acutely SOB and need to sit up for a number of minutes to help it resolve?”
- This occurs in both CHF and COPD
- Exertional dyspnea should be questioned, and if present, can hint toward the presence of COPD, abdominal loading, or poor cardiac reserve
- Feelings of anxiety may point toward psychogenic dyspnea but may also point toward an organic cause of a patient’s dyspnea
Associated Symptoms:
- Interrogate for the presence of chest pain, cough, hemoptysis, palpitations, syncope or presyncope
- Ask about the presence of anginal equivalents
- Inquire as to the presence of symptoms of systemic infection
- Seek clarification as to the presence or absence of nausea, vomiting, abdominal pain, changes in stooling, melena, and hematochezia
- Ask about symptoms of venous thromboembolism
- Inquire as to the presence of neurologic symptoms, looking for weakness, sensory disturbances, and other symptoms of focal neurological deficit
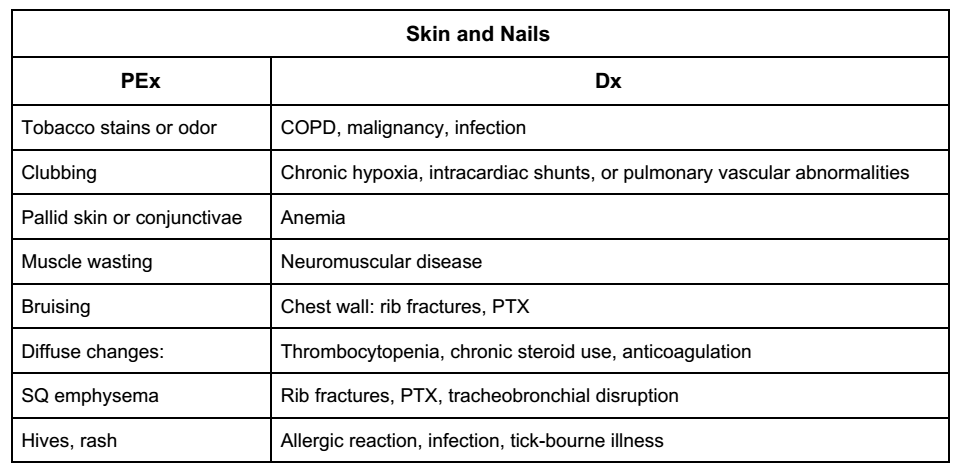
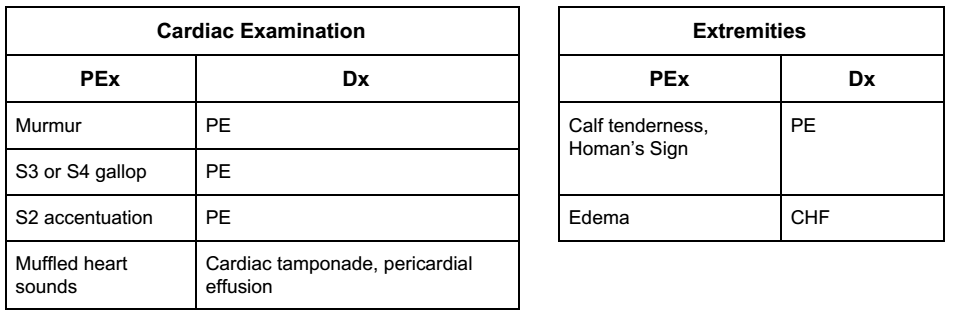
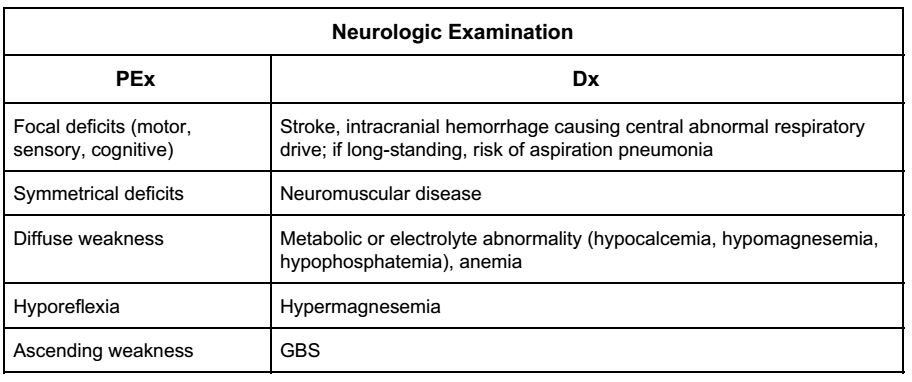
[4] Detail the physical examination for the dyspneic patient and highlight pivotal exam findings that point to specific pathologies.
The following tables have been adapted from Table 22.2 – Pivotal Findings in Physical Examination in Rosen’s Emergency Medicine, 9th Edition. Please see text for further clarification.



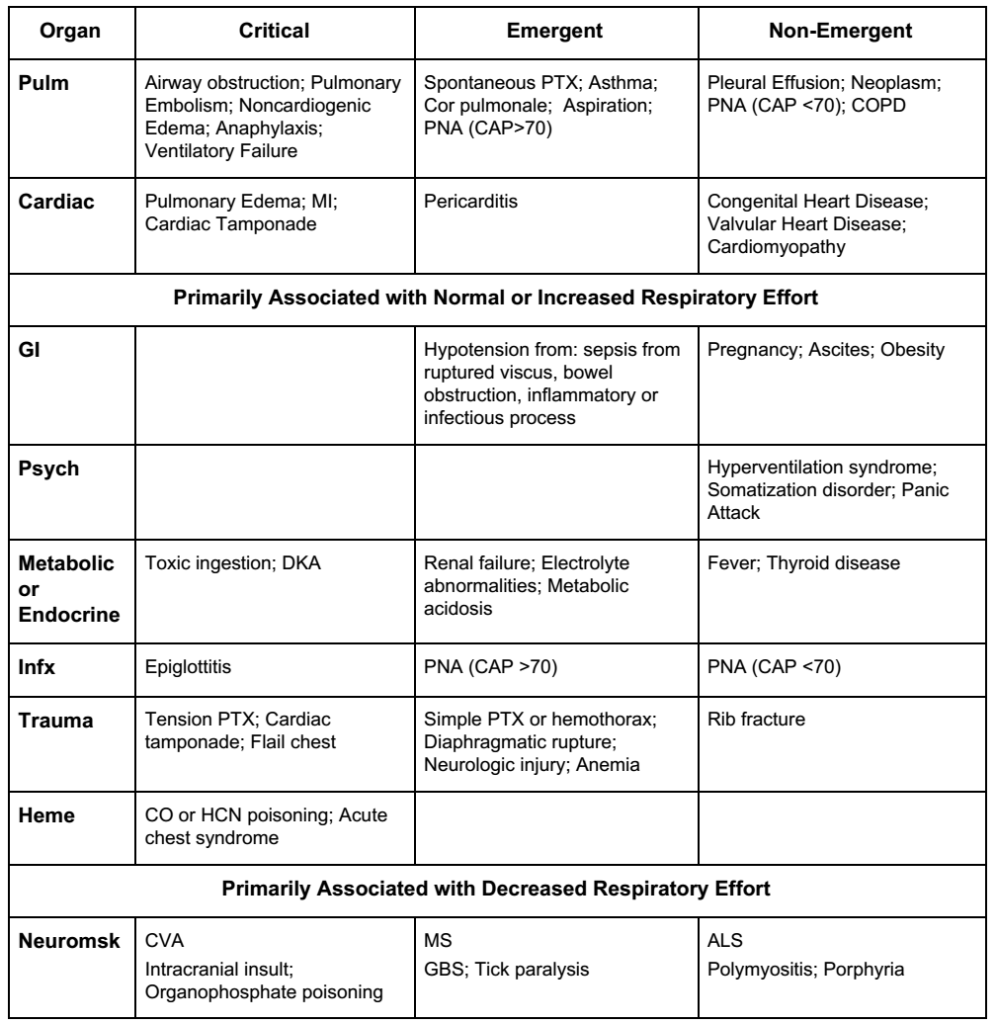
[5] Outline the differential diagnosis for the patient presenting with dyspnea and highlight 5 critical, 5 emergent, and 5 non-emergent causes of shortness of breath.
The following table has been adapted from Table 22.1 – Differential Diagnoses for Acute Dyspnea in Rosen’s Emergency Medicine, 9th Edition. Please see text for further clarification
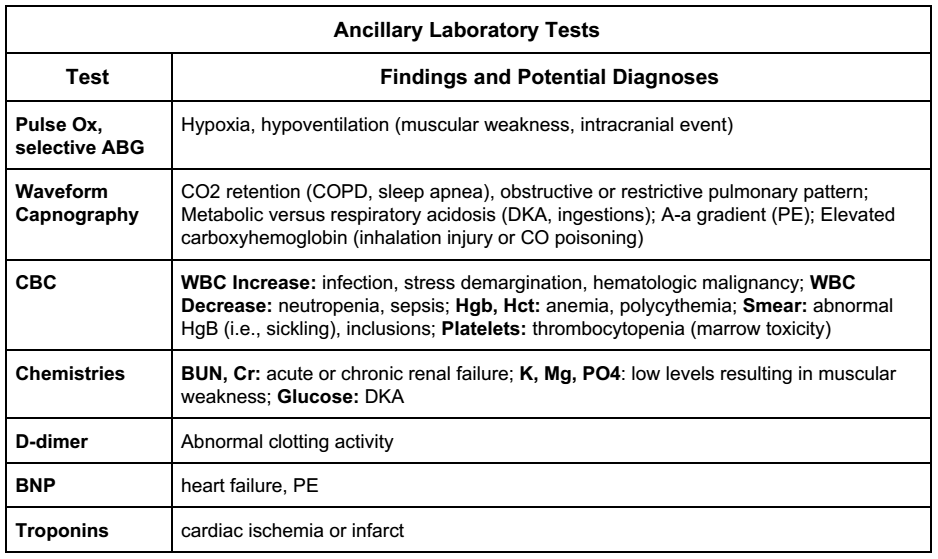
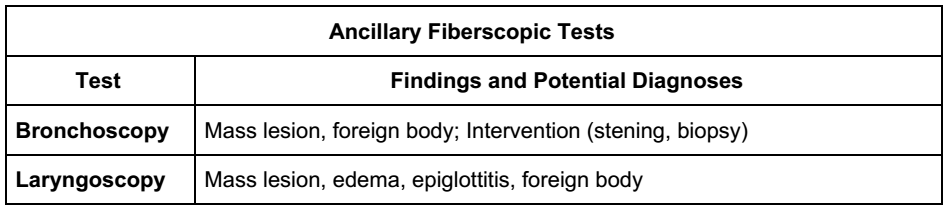
[6] What ancillary tests are indicated for the dyspneic patient?
Rosen’s offers an extensive battery of tests to consider for a dyspneic patient. Below, we present a distilled list of tests that are ordered or considered for most dyspneic patients. Read through Table 22.4 of Rosen’s for a more extensive list of potential evaluations.
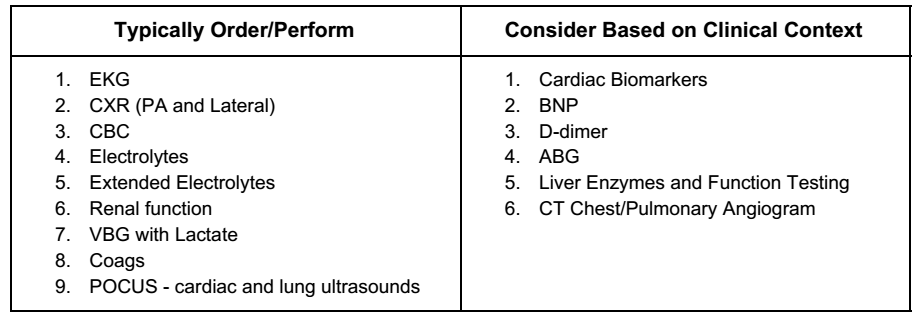
The following tables have been adapted from Table 22.4 – Ancillary Testing in the Dyspneic Patient in Rosen’s Emergency Medicine, 9th Edition. Please see text for further clarification.


[7] Detail the utility of point-of-care ultrasound in the assessment of the dyspneic patient.
POCUS for the dyspneic patient is essential. There is extensive data surrounding this topic in Emergency Medicine, but there is a good summary of the diagnostic utility presented in an excellent emDOCs post.
In summary:
- POCUS in isolation correlates well with diagnosis made by the ED physician in the patient with undifferentiated dyspnea
- POCUS diminishes the time to diagnosis in the ED for the dyspneic patient
- POCUS is highly specific and moderately sensitive for many of the acute causes of dyspnea in the ED

[8] Outline a management algorithm for the acutely dyspneic patient.
This algorithm is adapted from Figure 22.1 titled “Rapid assessment and stabilization of the dyspneic patient” from Rosen’s 9th Edition. Please refer to the text for further clarification.
- Assess for the presence of respiratory distress (defined as RR >24 or <8, presence of tripoding, accessory muscle use, retractions, altered mental status, and/or abnormal chest wall movement)
- If present, apply supplemental oxygen, apply pulse oximetry and continuous waveform capnography, and obtain IV access; proceed to step two after this has been completed
- If not present, obtain pulse oximetry readings, supplement O2 as needed, and perform a directed history and physical examination
- Determine if the patient is able to maintain their own airway or if there is evidence of respiratory failure
- If yes to any of the above, assist ventilation and proceed to step three
- If no, get a CXR and proceed with history and physical examination
- If assisting ventilation, assess breath sounds and prepare for endotracheal intubation or cricothyroidotomy and mechanical ventilation if air entry is equal bilaterally and there are no pathologic movements of the chest or signs of chest wall trauma
- If assisting ventilation and air entry is unequal bilaterally or there is pathologic movements of the chest/ signs of chest wall trauma, rapidly assess for signs of obstructive shock (hypotension, JVD, tracheal deviation, or US confirmation of PTX), immediately decompress the chest
- If no tension PTX suspected, perform beside US for cardiac collapse and PTX
- Once the airway is secured, get a portable CXR, repeat your physical examination, and perform a targeted history and physical examination and draw initial lab investigations
- If there is a + BNP, interstitial pattern on CXR, and clinical signs of CHF, consider getting an EKG and administering diuretics, nitrates, ACEi’s, morphine, and NPPV
- If there is wheeze and a clear CXR,and sharktooth capnography, consider anaphylaxis, bronchospasm, and administer bronchodilators/epinephrine/steroids/antihistamines as appropriate
- If there are rhonchi, diminished breath sounds, and an infiltrate on CXR, consider PNA/pleural effusion and administer ABx after obtaining blood cultures
- If there are no adventitious sounds +/- chest pain, consider PE versus anginal equivalent versus neuromuscular disorder or central neurogenic cause of the patients dyspnea
- Get an EKG, ABG, cardiac biomarkers +/- D-dimer +/- CT PE
- If trops +, consider ischemic causes and treatment for ACS
- If evidence of right heart strain on EKG, consider PE and treat for same
- Get an EKG, ABG, cardiac biomarkers +/- D-dimer +/- CT PE
- If there is unequal chest wall motion, signs of trauma, or evidence of PTX/hemothorax on US, consider thoracostomy
Wisecracks
[bg_faq_start][1] List three findings on chest radiograph suggestive of pulmonary embolism.
Answer: Fleischner sign, Hampton hump, Westermark sign, pleural effusion, Knuckle sign, Palla sign, Chang sign
We have broken these signs down for you below. The information on the diagnostic utility of these tests come from this Radiopedia article.
- Fleischner Sign
- Enlarged pulmonary artery
- Hampton Hump
- Peripheral wedge of airspace opacity that implies lung infarction
- 22% sensitive, 82% specific
- PPV 29%, NPV 76%
- Peripheral wedge of airspace opacity that implies lung infarction
- Westermark Sign
- Focal or regional oligemia in the lung
- 14% sensitive, 92% specific
- PPV 38%, NPV 76%
- Focal or regional oligemia in the lung
- Pleural Effusion
- 36% sensitive, 70% specific
- PPV 28%, NPV 76%
- Knuckle Sign
- Abrupt tapering of the pulmonary artery secondary to embolus
- Palla Sign
- Enlarged right descending pulmonary artery
- Chang Sign
- Dilated right descending pulmonary artery with sudden cut-off
Remember, CXR is not diagnostic for PE. You largely order CXR’s to rule out other pathologies that can cause the patient to become breathless. The vast majority of these signs are difficult to pick up at baseline, so take these findings with a grain of salt.
[bg_faq_end][bg_faq_start][2] What is the utility of venous blood gas testing and how do its values correlate with that of an arterial blood gas?
Answer: VBG is not perfect, but it is useful for the following parameters:
- pH (GOOD CORRELATION)
- Large volume of research that indicates that the pH on a VBG adequately correlates well with the pH on ABG
- There is a pooled mean difference of +0.035 pH units
- PaCO2 (GOOD AT IDENTIFYING NORMOCARBIA)
- Correlates well in patients with normocapnia (ie., if the VBG shows normocapnia, the patient is likely normocapnic on ABG)
- 100% sensitive in identifying hypercarbia (PaO2 > 45 mmHg) in AECOPD – although this conflicts with a recent meta analysis published in 2014
- Once the PaCO2 begins to climb, the VBG begins to become less reliable (ie., higher levels of CO2 on VBG do not correlate well with levels on ABG)
- Poor correlation in severe shock
- HCO3 (GOOD CORRELATION)
- Mean difference – 1.41 mmol/L
- Lactate (POOR CORRELATION AT HIGH LEVELS)
- Dissociates after 2 mmol/L
- Mean difference 0.08 mmol/L
- PaO2 (POOR CORRELATION)
- As stated above, poor correlation with ABG – do not rely on results
- ABG PaO2 often 36.9 mmHg higher on ABG with significant variability
- Base Excess (GOOD CORRELATION)
- Mean difference 0.089 mmol/L
So, when should you order an ABG?
- Assess PaCO2 in severe shock
- To determine PaCO2 when hypercarbic
- To accurately determine arterial lactate levels
For more information, refer to this excellent post from Life in the Fast Lane.
[bg_faq_end]


