This episode of CRACKCast covers Rosen’s 9th Edition Chapter 146, Antidepressants. Continuing the section on toxicology, antidepressants make up one of the most commonly prescribed medications in the general population. The use and misuse of antidepressants can have serious consequences and having a high suspicion of overdose in suicidal patients can lead to timely antidote therapy.
Shownotes – PDF Here
[bg_faq_start]Key Points
- Although rarely used for depression, MAOIs are used in the treatment of Parkinson’s disease
- Because serious symptoms can occur after a lengthy latent period, patients with reported MAOI overdose should be admitted for 24 hours, regardless of symptoms. Symptoms are characterized by tachycardia, hypertension, and CNS changes, and later cardiovascular collapse.
- The primary manifestations of TCA toxicity are seizures, tachycardia, and intraventricular conduction delay. IV sodium bicarbonate should be administered for QRS prolongation.
- DO NOT USE PHYSOSTIGMINE IN TCA OVERDOSE
- SSRIs are comparatively benign in overdose.
- SNRI ingestions can result in seizures, tachycardia, and occasionally intraventricular conduction delay.
- The hallmark feature of serotonin syndrome is lower extremity rigidity (spasticity) with spontaneous or inducible clonus, especially at the ankles.
- Serotonin syndrome is primarily treated with supportive care, including discontinuation of the offending agent, and benzodiazepines.
Rosens in Perspective
I like the little trip down memory lane here! Fun medical history tidbit – the class of antidepressants we know as monoamine oxidase inhibitors (MAOI) came from the anecdotal findings that patients treated for TB with isoniazid and iproniazid (which inhibit MAO) had improved mood symptoms. Therefore, there was the formation of the >60 year old theory that depression stems from an imbalance of monoamine neurotransmitters (eg dopamine, noradrenaline and serotonin).
We NEED TO KNOW THESE DRUGS.
- ⅕ people have a lifetime bout of depression, and are very likely these days to end up on one of this class of medications.
- Although antidepressants account for only 4% of poison control center calls, they make up approximately 10% of fatalities.
- These drugs range from the Bad -ish (SSRIs) do the dang near dirty/ugly (TCAs & MAOIs)
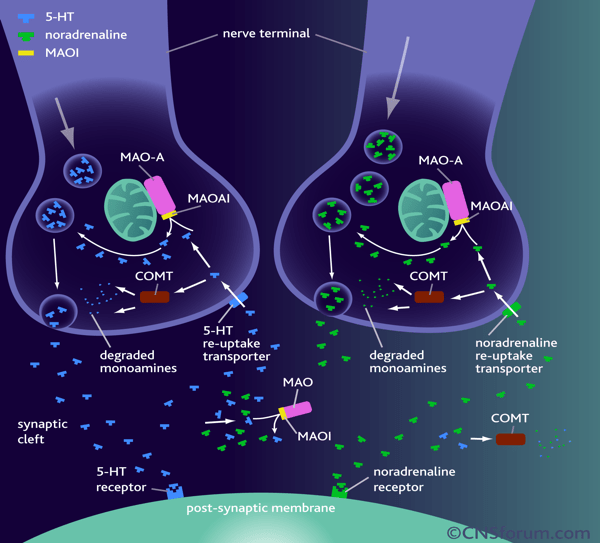
Another key fundamental understanding is how and where these drugs work:
Source here
MAOIs were the first!
- MAO is located on the outer mitochondrial membrane
- Responsible for breakdown of cytoplasmic catecholamines and other neurotransmitters (epinephrine, norepinephrine, dopamine, serotonin and tyramine)
- Monoamine oxidase type A (MAO-A) breaks down serotonin and norepinephrine
- Monoamine oxidase type B (MAO-B) breaks down phenylethylamine.
- Tyramine and dopamine are metabolized equally by both MAO A & B
- Most tissues contain both isozymes
- MAO-A = primarily placenta / sympathetic nerve terminals / intestinal mucosa
- MAO-B = primarily in platelets / basal ganglia.
The old school first generation MAOIs are non-selective and IRREVERSIBLE
- Major problems with food and other drugs (phenelzine, isocarboxazid, and tranylcypromine)
- The second-generation MAOIs can preferentially inhibit either MAO-A or MAO-B.
- Third-generation are reversible inhibitors (Ex. Moclobemide reversible A inhibitor)
“Drugs that selectively inhibit MAO-B disproportionately increase dopamine concentrations in the striatum. Selegiline is an irreversible MAO-B inhibitor used in the treatment of Parkinson’s disease. Importantly, the selectivity for MAO-B is only present at low doses. Rasagiline is also an irreversible inhibitor of MAO-B and has similar clinical efficacy with selegiline. Furthermore, unlike selegiline, which is metabolized to l-methamphetamine, rasagiline is not metabolized to an amphetamine derivative.”
- In addition to its antibiotic properties, linezolid, an oxazolidinone class antibiotic, is a reversible inhibitor of MAO, producing significant inhibition of MAO-A ***
- Also, herbals and OTC < remember to ask! For example, St John’s Wort is also a MAOI!!!
[1] List 7 pharmacodynamic effects of cyclic antidepressants and describe the physiologic result
CLASSIC PIMP QUESTION
- Sodium Channel Blockade
- QRS >100 (phase 0 of the action potential)
- Dysrhythmias
- Potassium Channel Blockade
- QTc prolongation
- Antihistamine
- Hypotension and sedation
- Anticholinergic = Usual toxidrome
- Red as a beet
- Dry as a bone
- Blind as a bat
- Mad as a hatter
- Hot as hell
- The bladder keeps its tone and the heart runs alone
- 5HT & NE reuptake inhibition (ie extra serotonin and norepinephrine)
- They look like sympathomimetic
- Tachycardia / hyperthermia, agitation, ALOC & Seizures
- GABA Blockade
- Seizures
- Alpha – 1 blockade
- Hypotension
[2] What are the ECG findings associated with TCA toxicity and what are their implications
As per LITFL
- Interventricular conduction delay — QRS > 100 ms in lead II
- Right axis deviation of the terminal QRS:
- Terminal R wave > 3 mm in aVR
- R/S ratio > 0.7 in aVR
- Patients with tricyclic overdose will also usually demonstrate sinus tachycardia secondary to muscarinic (M1) receptor blockade.
- Fast sodium channel blockade
- Dominant secondary R wave (R’) in aVR > 3mm
*** NOTE*** QRS > 100 = 30% risk of seizure & >160 50% dysrhythmia!!!
[3] Describe the management of TCA toxicity
*** Note: symptoms usually within 1-2 hours, severely poisoned= by 6 hrs***
ABCs
Decontamination
Elimination
Personal Protection
Antidote
Or
- R – Resuscitation
- R – Risk Assessment
- S – Supportive Care
- I – Investigations
- D – Decontamination
- E – Enhanced Elimination
- A – Antidotes
- D – Disposition
Management
If less than 2 hrs from known ingestion
- Activated Charcoal
- Avoid in unstable patients or if you’re heading to RSI
Cardiac instability (QRS > 100, hypotension, dysrhythmias)
- Bicarb (9%)
- 2meq/kg bolus until QRS narrows
- Consider infusion (3 amps (150 meq) bicarb in D5W as looking for the extra sodium!)
- STRONGLY Consider potassium replacement
- 3% hypertonic
- Lidocaine (sodium channel blocker) – listen to the podcast to understand how this works!
- Intralipid
Seizures
- Bicarb
- Benzos
- Phenobarb
- Propofol
- NO DILANTIN : can’t be given quickly enough to be effective, worsens hypotension, similar mechanism as Na channel blocking of lidocaine
Hyperthermia
- Go big if Ultra hot (possibility with co-ingestions and SS) – evaporative & ice immersion
- Intubate, deeply sedated and paralysed if not responding to above
- Watch for rhabdo, treat accordingly
Metabolic derangements:
- Metabolic acidosis with hyperkalemia
- Treat as indicated
- Avoid Sux! And DON’T GIVE PHYSOSTIGMINE
[4] What are the diagnostic criteria for Serotonin Syndrome?
Hunter criteria
- Exposure to a known serotonergic agent; AND
- Any of the following:
- Spontaneous clonus
- Inducible clonus and agitation or Diaphoresis
- Ocular clonus and agitation or Diaphoresis
- Tremor and hyperreflexia
- Hypertonic w/ Temp > 38oC and ocular clonus or inducible clonus
“The descending ladder of hyper-reflexia”
- As the hyper-reflexia gets less and less impressive, the additional criteria become more pronounced
[5] How can you discern between NMS and Serotonin Syndrome?
Both look the same = FARM
- Fever
- Autonomic instability
- Rigidity / rhabdo
- Mental status changes
However, the major differentiating features:
- NMS = parkinsonian type lead pipe rigidity; slower onset; similar presentation to the unwell septic patient
- SS = spastic rigidity – agitation / tremor / CLONUS / increased motor activity; rapid onset
- Onset: SS relatively rapid within hours NMS over days potentially
- Course: NMS may wax and wane. SS peaks then declines
- Obviously hyper-reflexia is the most important differentiator along with drug history
[6] What are the common meds causing Serotonin Syndrome?
See Box 146.1 in Rosens
- Cocaine
- Amphetamines
- SSRIs
- SNRIs
- TCAs
- MAOIs
- Dextromethorphan
- Tramadol
- Fentanyl & derivatives
- Methadone
- St John’s Wort
- Ondansetron
Rare: Linezolid & Methylene Blue!!! When mixed with SSRI use
[7] Describe the management of Serotonin Syndrome
ABCs
Consider narcan or glucose if needed
Decontamination w/ Activated Charcoal if <2hrs
ECG to r/o cardiotoxicity
R/O TCA / Tylenol / ASA
Supportive care:
- Fluids
- Cardiac monitor
- Observation for standard 6 hrs (longer if citalopram, escitalopram or bupropion)
- Consider cyproheptadine (in consultation w/ toxicologist)
- Treat hyperthermia
- Sedate
- Paralyse
- Intubate
- Cool
- Watch for rhabdo and hyperkalemia
[8] What is the primary risk of toxicity in Bupropion?
- Drug class = norepinephrine/dopamine reuptake inhibitor
- used for depression, ADHD, and smoking cessation
- Seizures are the major toxicity
- However, known myocardial depressant can lead to hypotension and cardiogenic shock
- Treat seizures aggressively with benzos and other GABA agents
- Always observe for 24 hrs for extended release formulations or congestions
- Note: Immediate release no longer available
[9] What are the 3 mechanisms by which MAOI toxicity can occur? And what is the clinical syndrome?
- See table 146.1 of current MOI agents currently available
Three mechanisms:
- Tyramine syndrome
- Drug interactions
- Overdose
Tyramine syndrome (food based)
- Usually broken down by MAOI A
- No MAO = release of serotonin
- Features : headache / flushing / Hypertension / diaphoresis
Drug Interactions
- SSRIs/SNRIs/Sympathomimetics and grab bag of fentanyl, tramadol etc (aka SS)
Overdose
Show notes: What is a Tyramine Reaction
According to LITFL
Tyramine reaction:
This occurs after an ingestion of tyramine containing foods such as cheese and beer. It precipitates am hypertensive crisis. Patients may complain of headache, sweating, agitation and chest pain. Complications include an intracranial bleed, rhabdomyolysis, acute renal failure and DIC. It should be managed as per the resuscitation section to lower BP and alleviate anxiety and tachycardia.
[10] List 5 foods and 5 classes of meds that can interact to cause MAOI toxicity
Med Classes: anything with serotonergic effects (see question 6)
For example:
- Cocaine
- Amphetamines
- SSRIs
- SNRIs
- TCAs
- MAOIs
- Dextromethorphan
- Tramadol
FOOD:
- Tyramine is an indirectly acting sympathomimetic amine that is present in aged cheeses, red wine, smoked or pickled and aged meats, and other foods
Full list as per wikipedia:
- Meats that are potentially spoiled or pickled, aged, smoked, fermented, or marinated (some fish, poultry, and beef); most pork (except cured ham)
- Chocolate
- Alcoholic beverages
- Fermented foods
- most cheeses (except ricotta, cottage, cream and Neufchâtel cheeses)
- sour cream
- Yogurt
- shrimp paste
- soy sauce
- soybean condiments: teriyaki sauce, tempeh, miso soup
- Sauerkraut
- Kimchi
- broad (fava) beans, green bean pods, Italian flat (Romano) beans, snow peas, edamame
- Avocados
- Bananas
- Pineapple
- eggplants, figs, red plums, raspberries
- peanuts, Brazil nuts, coconuts
- an array of cacti and the holiday plant mistletoe.
[11] Describe the management of MAOI toxicity.
According to LITFL
Note: Juicy Dr. JG Pearl: Generally, treatment is supportive/the same as for sympathomimetic overdose/ serotonin syndrome, only thing to be aware of is that catecholamine burnout is very common… so may actually require pressor support later on.
Seizures:
- IV benzodiazepines incrementally dosed every 5 minutes to effect.
- Check the patient is not in a dysrhythmia
- Can be managed with benzodiazepines
- (varying doses in the textbooks, easy method is 0.1mg/kg IV for lorazepam (max 4mg) / midazolam (max 10mg) / diazepam (max 10mg). Or…
- Lorazepam 0.1mg/kg max 4mg
- Diazepam 0.15mg/kg max 10mg
- Midazolam 0.2mg/kg max 10mg
- Consider pyridoxine – check out the podcast !
Hyperthermia (>39.5 degrees centigrade):
- This is a feature of severe toxicity and needs immediate control to prevent multi organ failure.
- Treatment is with paralysis, intubation, ventilation and cooling.
Hypertension and Tachycardia:
- Usually controlled with titrated doses of benzodiazepines as listed above, aiming for gentle sedation and a heart rate falling towards 100 beats per minute.
- Severe hypertension including tyramine reaction may require the following:
- Titrate vasodilator infusion of sodium nitroprusside and glyceryl trinitrate (need something that can be reduced rapidly in the event of autonomic instability)
- alpha-antagonism: Phentolamine 2 – 3 mg increments every 10 – 15 minutes until BP close to 140 systolic
- Beta-adrenergic blockers are contraindicated due to the risk of unopposed alpha-agonist stimulation.
- Life threatening serotonin toxicity: Requires paralysis, intubation and ventilation to prevent multi organ failure
Supportive Care
- Agitation and tachycardia: Increasing anxiety, sweating, tremor, tachycardia and mydriasis may herald the onset of seizures.
- Titrated doses of benzodiazepines are effective e.g. diazepam 2.5 – 5 mg every 5 minutes IV until gentle sedation is achieved and a heart rate falls towards 100 beats per minute is considered safe.
Investigations
- Screening: 12 lead ECG, BSL, Paracetamol level
- Specific:
- Serial ECGs with moclobemide due to QT prolongation.
- Labs: the usual plus CK, troponin, ABG, Chest X-ray, CT brain and EEG (as indicated)
Decontamination:
- 50 grams of activated charcoal can be given to cooperative patients within 2 hours post ingestion of tranylcypromine or phenelzine.
- Activated charcoal is contraindicated in the awake patient with a more delayed presentation or one with symptoms due to the risk of seizures and rapidly declining GCS
- Moclobemide does not require activated charcoal and can be managed with supportive care alone
Enhanced Elimination
- Not clinically useful.
Antidote
- None available for MAOIs per se.
- Serotonin toxicity: There may be a role for serotonin antagonists for mild to moderate serotonin toxicity refractory to benzodiazepines. If the patient has severe toxicity aggressive supportive care including cooling, intubation, ventilation and neuromuscular paralysis will be necessary – do not use the specific serotonin antagonists below in this situation.
- Cyproheptadine: Antihistamine with anti-serotinergic effects, can be given orally or via a nasogastric tube. 8mg TDS if there is a positive response after the first dose. Stop after 24 hours.
- Olanzapine: 5 – 10 mg sublingual (avoid if worried about NMS and D2 blockade)
Disposition
- Patients who are clinically well at 12 hours with no signs of serotonin toxicity or ECG changes are medically cleared. Do not discharge at night.
- Symptomatic patients following moclobemide overdose require 6 hours of close observation and then can be medically cleared if asymptomatic and they have a normal ECG.
Patients with severe symptoms or who have ingested phenelzine or tranylcypromine usually require ICU level care
[12] What is discontinuation syndrome and how is it managed?
- This is a withdrawal / med discontinuation syndrome
- does not always develop, but when it does, it typically starts within 3 days after meds stopped
- Looks just like recurrence of the underlying depression (which has overlap of some symptoms)
- Symptoms include:
- SSRIs = most commonly nausea, lethargy, headache, and dizziness.
- More common after discontinuation of drugs with shorter half- lives (eg, paroxetine) than of drugs with longer half-lives (eg, fluoxetine).
- Six general categories:
- disequilibrium (eg, dizziness, ataxia)
- sleep disturbances
- gastrointestinal symptoms
- affective symptoms (eg, irritability, anxiety)
- sensory symptoms (eg, electric shock–like sensation, paresthesias)
- general somatic symptoms (eg, headache, tremor, anorexia, diaphoresis).
- SNRIs typically WILL GET discontinuation syndrome
- Not as life-threatening compared to GABA withdrawal (ethanol or benzodiazepines)
- EXCEPT neonates born to mothers using TCAs = serious, potentially life- threatening withdrawal
- TCA withdrawal is similar to SSRI withdrawal, although sensory abnormalities and equilibrium disturbances are rare with TCA discontinuation.
- Non–life-threatening arrhythmias are rare after discontinuation of the TCAs
From uptodate
“Factors that appear to be associated with more frequent and severe discontinuation symptoms include
- Shorter antidepressant elimination half-life (eg, <24 hours)
- Nonlinear antidepressant pharmacokinetics
- Anxiety symptoms at the onset of antidepressant treatment
- Higher antidepressant doses
- Longer duration of treatment at therapeutic doses (eg, ≥5 to 8 weeks)
- Prior history of discontinuation symptoms
Discontinuation symptoms can occur with any SSRI, but the frequency and severity of symptoms appear to vary according to the drug’s elimination half-life. Randomized trials indicate that the likelihood of discontinuation symptoms is as follows:
- Least risk of symptoms – Fluoxetine
- Intermediate risk – Citalopram, escitalopram, and sertraline
- Greatest risk – Paroxetine
A study of clinician-initiated reports of adverse effects found that discontinuation symptoms occurred 10 times more often with paroxetine than sertraline, and 100 times more often with paroxetine than fluoxetine***”
Management
- Patients with mild withdrawal symptoms do not require specific therapy
- For severe symptoms = treatment involves restarting of the antidepressant
- Continue by gradual tapering dose
- If D/C SNRI, consider switch to long acting SSRI (fluoxetine) and then D/C (fluoxetine has SUPER LONG HALF LIFE 1-3 days and metabolite 6-14 days)
[13] List 8 drug causes of wide QRS / Sodium channel blockade
***Basically, all of the ANTI- anything drugs***
Rosen’s list / As per LITFL / WikiEM:
- Tricyclic antidepressants (= most common)
- class IA antidysrhythmics (eg, procainamide, disopyramide, quinidine)
- class II antiarrhythmics (eg sotalol or metoprolol) & propranolol
- class IC antidysrhythmics (eg, flecainide, encainide, and propafenone)
- local anaesthetics (bupivacaine, ropivacaine)
- Antimalarials (chloroquine, hydroxychloroquine)
- Antispasmodics (eg cyclobenzaprine)
- Antipsychotics (1st and second generation eg chlorpromazine, )
- Anticonvulsants (eg dilantin, Carbamazepine)
- Anti-Parkinson’s agent (eg Amantadine ie dopamine agonist)
- Cocaine
- Antihistamine agents (eg Diphenhydramine)
- Dextropropoxyphene (opioid brand name Darvon-N in Canada, now recalled)
Wisecracks
[bg_faq_start][1] What are the indications for Bicarb in TCA toxicity?
- QRS > 100 (if different from baseline)
- Hypotension
- Dysrhythmia
- Seizures
- Acidosis
When do you switch to Hypertonic?
- pH > 7.55
- Failure of QRS to respond to NaHCO3
[2] List 3 meds to avoid in TCA overdoses
Avoid anything with Na+ channel blocking effects!
- Physostigmine
- Class IA IC drugs
- Ia – Quinidine, procainamide, disopyramide (depress phase 0, prolonging repolarization)
- Ic – Flecainide, propafenone, moricizine (markedly depress phase 0, minimal effect on repolarization)
- Dilantin (phenytoin)
[3] List the 2 common situations for NMS
- High Potency antipsychotics
- Abrupt cessation of Parkinson’s meds
[4] Expand on the hot & bothered ddx
- MAOI toxicity
- sympathomimetic drugs of abuse (cocaine and amphetamine derivatives)
- anticholinergic (or antimuscarinic) toxicity (diphenhydramine, cyclic antidepressants, anti-Parkinson drugs, and jimson weed)
- methylxanthine toxicity (eg, theophylline and caffeine)
- acute withdrawal states (eg, ethanol and benzodiazepines)
- neuroleptic malignant syndrome (NMS)
- serotonin syndrome
- environmental hyperthermia or heat stroke
- meningitis and encephalitis
- Pheochromocytoma
- carcinoid syndrome
- thyroid storm
- hypertensive emergency
This episode was uploaded and copyedited by Riley Golby (@RileyJGolby)