This episode of CRACKCast covers Rosen’s Chapter 91 for the 8th Edition (Chapter 81 9th Edition), Pancreas. This chapter covers the various pathologies, diagnoses and treatments of the Pancreas.
Shownotes – PDF Here
[bg_faq_start]Rosen’s in Perspective
Pancreatitis is when the pancreas starts to auto-digest itself, usually because some spark (e.g. toxin) sets off an early activation of digestive enzymes. This causes a cascade of inflammation which leads to SIRS and possible intestinal bacterial translocation. This disease can have a mortality that ranges from 4% to 30% in severe cases!!!
The pancreas – divided into head, body and tail – lives in the retroperitoneum. The head abuts the duodenum, where is the tail crosses midline and abuts the spleen.
- Exocrine functions: secretion of digestive enzymes (eg. lipase, amylase, trypsinogen, and other proteases)
- Endocrine functions: secretion of insulin, glucagon, and somatostatin

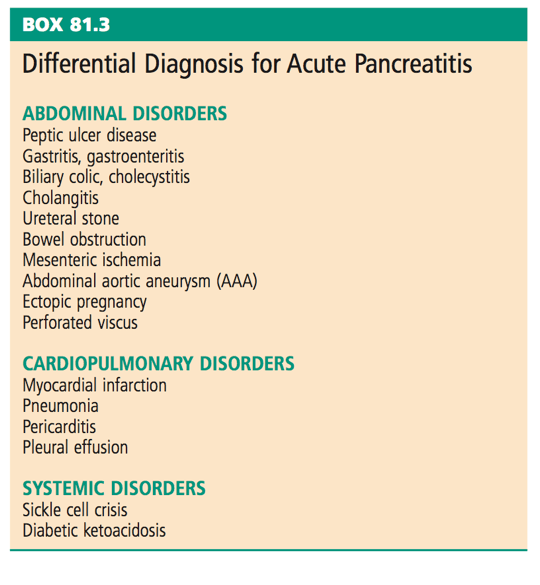
Question 1) List 10 differential diagnoses for acute pancreatitis
Question 2) List 10 causes of pancreatitis. Which are most common in adults? Which one is most common in pediatrics?
See table 81.1 – but in general these are the common adult causes:
- Gallstones (40%–70%)
- Chronic alcohol consumption (25%– 35%).
- Endoscopic retrograde cholangiopancreatography (ERCP)
- Drugs
- Trauma
- Idiopathic (up to 10-30% of the time; may be due to microlithiasis?)
- PEARLS:
- The risk of biliary pancreatitis is actually correlated with the decreasing size of gallstones (inverse relationship! I.e. small tiny gallstones increase the risk!))
- Smoking and diabetes are independent risk factors for the development of pancreatitis
- Females = think stones
- Men = think ETOH
Pediatric causes:
- Trauma (#1)
- Infection (viral: Mumps and other viruses (EBV, CMV)
- Congenital (aberrant ductal structure, stone forming diseases – sickle cell disease, hereditary spherocytosis)
- Genetic lipid disorders
Its mnemonic time: IGETSMASHED
- Idiopathic
- Gallstones
- Ethanol
- Trauma
- Steroids
- Mumps and other viruses (EBV, CMV, HIV)
- Autoimmune diseases (SLE, polyarteritis nodosa, pregnancy)
- Scorpion stings
- Hypercalcaemia, hyperlipidaemia, hypothermia, hypotension (ischemia)
- ERCP, emboli
- Drugs (SAND + MR VET)
- Sulphasalazine, azathioprine, NSAIDS, diuretics + metronidazole, ranitidine, valproate, erythromycin, tetracyclines

Question 3) Describe 6 management priorities in acute pancreatitis.
Again, this is mostly supportive!
- Volume resuscitation – ideally with Ringer’s Lactate
- Major third spacing, decreased PO intake, V/D, diaphoresis, ketosis
- Early fluid resuscitation reduces SIRS and organ failure at 72 hrs.
- Resuscitate to correct hypotension, improve urine output, and correct hemoconcentration.
- Pain control
- Narcotics are safe!
- Correct any absolute electrolyte deficits:
- Low ionized calcium
- Hypomagnesemia
- Hypokalemia
- Correction of hyperglycemia (insulin deficiency)
- Treat nausea
- Initiate oral or enteral feeding ASAP
- This is in contrast to the old dogma of “no feeding”.
- Now we know that early enteral feeding decreases mucosal atrophy, prevents bacterial translocation, and may shorten hospital stay.
- Begin with a low-fat solid diet as tolerated
- Consider early U/S post-diagnosis and then → ERCP for anyone with cholangitis or biliary obstruction (jaundice, elevated bilirubin, sepsis)
- Consider antibiotics only if:
- Septic (tachycardia and tachypnea don’t count)
- Evidence of infected necrotizing pancreatitis
- Usually surgical, endoscopic or radiologic intervention only considered until ~4 weeks when the collection becomes walled off.
- Extrapancreatic infections
Things that don’t help:
- Histamine H2 blockers
- Prophylactic antibiotics
Consider delayed surgical cholecystectomy
Discharge criteria:
- Mild pancreatitis:
- With controlled pain, tolerating PO intake, no signs of complications
Question 4) What are the early, late and chronic complications of pancreatitis?
Pancreatitis is usually classified as either: interstitial edematous (I.E.) VS. necrotizing. The interstitial type develops few local complications, and usually resolves in a week or so. The complications we’ll discuss now. This is revised from Box 81.2 (9th Ed.)
- Acute complications (< 4 weeks onset):
- Local:
- Acute hemorrhage (intraluminal GI bleeding or intraabdominal)
- Ileus → bowel obstruction
- Peripancreatic fluid collection (homogenous) – adjacent to pancreas – seen in I.E. pancreatitis
- Acute necrotic collection (heterogeneous) – intra/extrapancreatic. – seen in necrotic pancreatitis.
- Systemic:
- SIRS – bacteremia – sepsis
- Atelectasis → pleural effusions → ARDS
- Renal failure
- Multi-system organ failure / shock / DIC
- Hyperglycemia, hypocalcemia (low albumin / magnesium levels)
- Local:
- Late (>4 weeks):
- Local:
- Pancreatic pseudocyst – homogeneous fluid collection with well defined wall (seen in Interstitial edematous pancreatitis).
- Walled-off necrosis (heterogenous) with fluid in a well-defined wall. Intra/extrapancreatic.
- Bowel necrosis
- Splenic / portal vein thrombosis
- Systemic:
- Pleural effusions
- Glucose intolerance
- Local:
- Chronic:
- Chronic pancreatitis (pancreatic tissue replaced by fibrous tissue).
- With associated opiate dependence / addiction
- Malnutrition / malabsorption / steatorrhea
- Diabetes
- Renal failure
- Cirrhosis
- Pancreatic cancer
- Chronic pancreatitis (pancreatic tissue replaced by fibrous tissue).
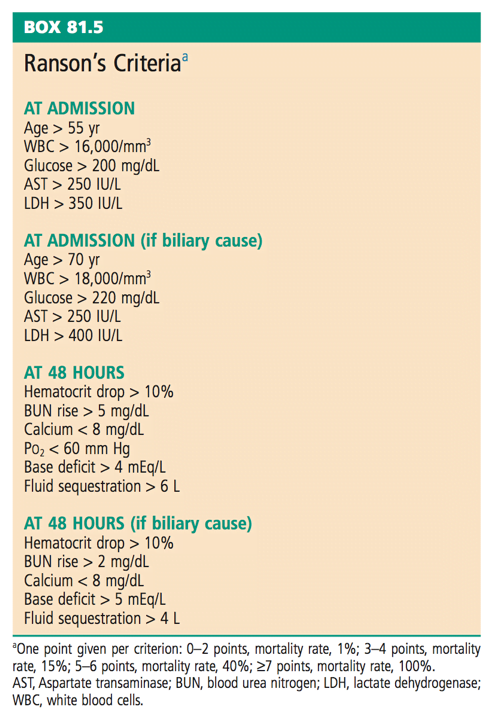
Question 5) Describe Ranson’s criteria and the Atlanta criteria
The clinical picture of pancreatitis is variable! And the level of pain doesn’t correlate with disease severity. To make the diagnosis of pancreatitis you need ⅔ of these:
- Clinical features (see textbook for a description)
- Laboratory results (lipase or amylase > 3x ULN)
- Imaging tests (not a requirement!)
These are a couple of scoring tools that exist, more for testing/research purposes than actual clinical application in the ER.
The Ranson’s criteria: see https://www.mdcalc.com/ransons-criteria-pancreatitis-mortality This is the most well known scoring tool. Unfortunately it uses 5 yes/no criteria at the admission mark, and 6 criteria evaluated at the 48 hr mark. Again, this makes it less useful in the ER! Let’s quickly run through it because your consultants may ask you about it…
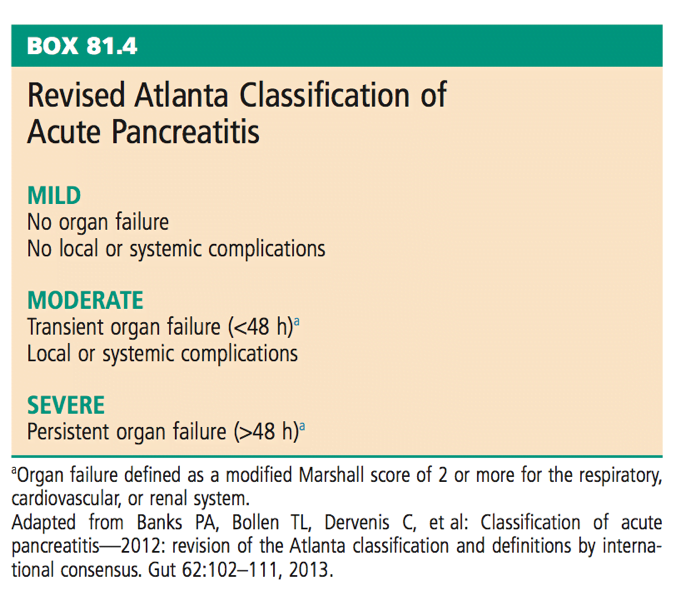
The revised Atlanta classification of acute pancreatitis is quite simple, because it breaks people down into (mild-moderate-severe). Unfortunately, you can’t really put anyone into a category until the 48 hr mark. Let’s quickly go through it now so you know what it includes….
There are many other scoring tools that exist – APACHE II, CTSI, BISAP, HAPS, all of which don’t seem to be the silver bullet for acute pancreatitis. So as a result, in the ER we can’t really predict which patients with pancreatitis are going to need ICU and which aren’t…
At the end of the day we’ll have to use our best judgement based on the patient in front of us:
- Their hemodynamics
- Their list of comorbidities
- Their laboratory findings (e.g. elevated ALT, creatinine)
- Their imaging findings (massive complex necrotic pseudocyst)
Question 6) List causes of chronic pancreatitis. What is the best diagnostic tool? What 4 findings can be seen in chronic pancreatitis?
- Causes
- Toxic-metabolic
- ETOH abuse
- Smoking
- Obstructive
- Genetic
- Autoimmune
- Post-necrotic acute pancreatitis
- Idiopathic
- Toxic-metabolic
- Diagnosis:
- Clinical features, laboratory analysis, imaging tests – still the best rule of thumb
- However, lab tests are less helpful:
- Amylase and lipase may not rise to the same degree or may be normal
- Liver function tests may be elevated due to concurrent ETOH abuse / biliary obstruction due to cirrhosis
- Likely have chronic hypoalbuminemia, hypocalcemia, hyperglycemia
- X-rays may show pancreatic calcifications
Best tests of choice:
- CT
- Dilated pancreatic ducts
- Atrophy
- Microcalcifications
- Pseudocysts
- MRCP
- Endoscopic ultrasound = most sensitive tool
Question 7) Describe the management of chronic pancreatitis (6 priorities)?
- Supportive
- Pain relief
- Start with NSAIDS / acetaminophen
- Octreotide
- Celiac plexus block
- Correction of fluid imbalance
- Correction of electrolyte deficits
- Glucose control
- Correction of malnutrition
- Oral enzyme replacement
- Antioxidants
- Healthy diet
- Smoking / ETOH cessation
- Endoscopy:
- Drainage of symptomatic pseudocysts / ductal leaks (refractory ascites)
- Stenting obstructed bile ducts
- Pain relief
Question 8) What is the 5 year survival rate for pancreatic cancer? Describe typical clinical findings. How is it diagnosed? What is the management?
This is a terrible disease, because it often goes undetected until later stages and has very poor survival. 5% at 5 years from the time of diagnosis – with high risk of metastasis to the liver and lungs
- Clinical findings
- Gastric outlet obstruction
- Hypoglycemia (insulinoma)
- Diarrhea
- Glucose intolerance (glucagonomas)
- Jaundice (obstruction)
- Weight loss
- Dermatitis
- Diagnosis
- CT with IV contrast (many subtle findings!)
- Endoscopic ultrasound (most sensitive test in the early disease)
- Management
- Some ampullary masses can be successfully resected, but the majority of cases have metastatic disease by the time they present
- Chemo and radiation may be helpful – in a small subset
- Palliative therapy
- Pain control
- Treatment of GI bleeding
- Bowel obstruction correction
- Treatment of acute cholangitis / venous thrombosis
Wisecracks
[bg_faq_start]Question 1) Specifically list 10 drug causes of pancreatitis.
- Cannabis
- Codeine
- Dapsone
- Enalapril
- Furosemide
- Isoniazid
- Metronidazole
- Pravastatin
- Procainamide
- Simvastatin
- Sulfamethoxazole
- Tetracycline
- Valproic acid
These are some of the class Ia drugs – from Uptodate – where people have developed pancreatitis on a re-challenge of the drug and other causes of pancreatitis have been ruled out (e.g. ETOH, gallstones, etc.).
[bg_faq_end] [bg_faq_start]Question 2) List 5 causes of false-positive amylase elevation.
Amylase is an enzyme that functions in carbohydrate digestion. The levels do go up in pancreatitis, but also can rise from a myriad of other pathologies:
- Parotitis
- Malignancy
- Trauma
- Burns
- Liver disease
- Cholecystitis
- Renal failure
- HIV
- Pregnancy
- …and many others!
That’s why we use lipase more often – because its predominantly produced by the pancreas. And more sensitive.
Should we then use both? NOPE! Testing both enzymes doesn’t improve our sens/specificity. So just get the lipase (plus bilirubin, calcium, serum triglycerides, glucose, and ALT).
And on a final note – the degree of elevation DOES NOT correlate with disease severity or prognosis.
[bg_faq_end] [bg_faq_start]Question 3) List 4 peripancreatic/local complications of pancreatitis that may be visualized on CT
CT is only recommended in the setting of confirmed pancreatitis (labs + clinical exam) when:
- Diagnostic uncertainty (i.e. only ⅓ criteria)
- To rule out other pathology (e.g. duodenal perforation)
- Assess for complications in people who aren’t responding to traditional therapy in 48 hrs
In fact, to evaluate for complications of pancreatitis, it’s best to order a CT with IV contrast in (minimum) 3-7 days to look for:
- Necrosis
- Pseudocyst formation
- Abscess
- Arterio-venous thrombosis
Although an initial ultrasound may be unable to visualize the pancreas due to bowel gas, it can be very helpful to look for any subtle biliary tract dilatation / disease.
[bg_faq_end]This post was uploaded and copyedited by Andrew Guy (@andrew_s_guy)


