This episode of CRACKCast covers Rosen’s Chapter 73, Asthma. Not just for kids! This disease process is satisfying to treat when patients respond well to therapy, but recognition of critically-ill patients is an important first step in management.
Shownotes – PDF Here
[bg_faq_start]Rosens in Perspective
Basic Principles:
- Reverse Obstruction
- Treat Hypoxia
- Treat Inflammation
Basic definition:
- A chronic airway inflammatory disorder
- Recurrent episodes of wheezing, breathlessness, chest tightness, and coughing
- Variable airflow obstruction (with varying degrees of reversibility) either spontaneously or with treatment.
According to UpToDate: The basic steps of care:
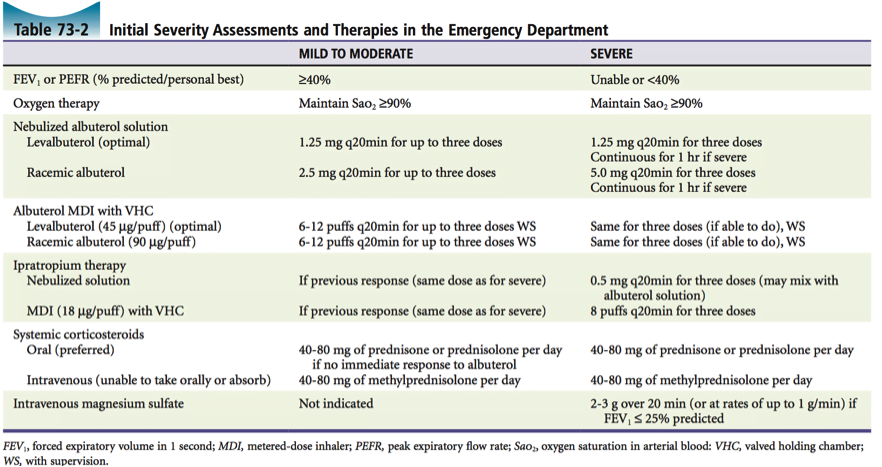
- Assess the severity of the attack
- Assess potential triggers (eg. animal dander, pollen, mold, respiratory infection, beta blockers, NSAIDs, cigarette smoking, non-adherence)
- Use inhaled short-acting beta agonists early and frequently, and consider concomitant use of ipratropium for severe exacerbations
- Start systemic glucocorticoids if there is not an immediate and marked response to the inhaled short-acting beta agonists
- Make frequent (every one to two hours) objective assessments of the response to therapy until definite, sustained improvement is documented
- Admit patients who do not respond well after four to six hours to a setting of high surveillance and care
- Educate patients about the principles of self-management for early recognition and treatment of a recurrent attack and develop an “asthma action plan” for recurrent symptoms
Know how to interpret how bad your patient’s asthma is at baseline!!!
Looking for more info: check out
https://lifeinthefastlane.com/ccc/acute-severe-asthma/
https://emergencymedicinecases.com/pediatric-asthma/
http://rebelem.com/rebelcast-crashing-asthmatic/
http://www.emdocs.net/critical-asthma-patient-pearlspitfalls-of-management/
https://coreem.net/core/basic-asthma-management/
https://coreem.net/tag/crashing-asthmatic/
[1] 10 different causes of a wheeze
[2] List 8 risk factors for death from asthma
[3] List 6 objective findings of severe asthma
[4] 10 therapies for an acute severe asthma exacerbation
Let us break this down into treatments supported by:
- Good evidence
- Sketchy evidence
- No evidence/not recommended
Good Evidence
Our work-horses are:
- O2 for sat titrated >90% or >95% in pregnant woman or known heart disease
- Short acting Beta Agonist (eg ventolin)
- Anticholinergics (eg Atrovent or ipratropium)
- Corticosteroids (eg prednisone or methylprednisilone) – no taper necessary if not pre-existing use or not used for >14days
- Magnesium sulfate – calcium channel– blocking properties, inhibition of cholinergic neuromuscular transmission, stabilization of mast cells and T lymphocytes, and stimulation of NO and prostacyclin.
Sketchy Evidence
- Inhaled Anesthetic agents (like sevo or desflurane). Note: be careful of hypotension seen with concurrent use of volatile anesthetics, acidosis, beta agonists and theophylline.
- Intravenous Ketamine initial bolus 0.5-1mg/kg followed by infusion of 0.5-3mg/kg/hr
- Enoximone – only in europe: selective phosphodiesterase III inhibitor
- Parenteral beta-agonists – evidence that inhaled beta agonists are superior to IV: exception is severe anaphylaxis requiring epinephrine (IM or IV)
- High-dose inhaled glucocorticoids: opposing evidence for effect: net recommendation is PO intake in exacerbations
- Helium-oxygen: heliox. The good ole last ditch attempt. Conflicting evidence: not recommended
- Leukotriene receptor antagonists: Basically not recommended to work in exacerbations except those induced by aspirin or NSAID use. Some small evidence that their use (eg montelukast or zafirlukast)
No evidence
- Methylxanthines (eg theophylline) – stop using it! Increase adverse events when mixed with beta agonists. Only recommended to maintain people on it if they are on it in the community
- Empiric antibiotics – you guessed it. With signs of overt infection (eg lobular pneumonia) not helpful. Possible that high procalcitonin levels may reflect bacterial infection
- Nebulized furosemide – thought to help exercised induced asthma, but no data to support its use
[5] Discuss a ventilation strategy for the critically-ill asthmatic patient
- Induction agent: Ketamine/Propofol/Etomidate. No benefit superiority proven yet, but ketamine and propofol have proven bronchodilation. Use Paralysis : succs or roc
- Vent mode: VC! : control mode as they are paralysed! Volume over pressure limited modes in patients with airflow obstruction issues.
- Tidal volume 6-8cc/(ideal body weight in kg): lung protective strategy
- Minute ventilation (respiratory rate multiplied by tidal volume): less than 115 mL/kg/min
- Allow increased expiratory time by decreasing I:E ratio (1:3 or 1:4 up to 1:5)
- Low PEEP (start approx 5 or 80% intrinsic PEEP)
- Start FIO2 at 100 percent then titrate downwards for SpO2 above 90% or PaO2 above 60 mmHg
For more see EMRAP’s vent strategy here: https://www.emrap.org/episode/shockasthmaand/criticalcare
[6] Discuss disposition and discharge planning for an acute asthma exacerbation presenting to the ER
Wise Cracks
[1] What is delayed sequence intubation? Can it be used for severe asthma exacerbation?
As Rosen’s cover’s NIPPV has shown to prevent intubation of ASTHMA in the ICU setting. In this line, the prolific crew at EMCRIT and Dr. Weingart himself has come up with a different approach to approaching the patient in respiratory extremis.
http://www.annemergmed.com/article/S0196-0644(14)01365-1/abstract
[2] What about pregnancy and asthma is so important?
Pregnant woman have increased O2 demand, decreased FRC, and baseline hyperventilation that is compensated for by a metabolic acidosis. ABGs in pregnancy normally show a pH 7.4-7.45 with a paCO2 of 28-32. So easy to miss the tiring, hypercapnia in pregnancy with a “normal” gas of 7.35 and PCO2 of 35-45. Pay attention to the CLINICAL PICTURE!
[bg_faq_end]
This post was uploaded and copyedited by Riley Golby (@RileyJGolby)