This episode of CRACKCast covers Rosen’s Chapter 69, Elder Abuse. In the last of our series on vulnerable populations, this episode covers elder abuse. Unfortunately, this is all too common, but by staying vigilant and knowing clues on history and physical we as emergency practitioners have the ability to save and improve lives!
Shownotes – PDF Here
[bg_faq_start]Rosen’s in Perspective:
- The elderly and “oldest” old population is growing.
- Because the elderly population are becoming an ever increasing proportion of ER patients we need to be aware of elder abuse and neglect
- We need to start screening for it more often!
- One review from 2008 identified 6% of older people living in the community experiencing abuse in the last month! with only 1 of 14 being reported
- The elderly are a very vulnerable group:
- Financially
- Due to cognitive decline
- Physical deconditioning
- Isolation
- Physicians may be the only person an aged individual sees outside their family – so we may the patient’s only chance to get to safety
- Most perpetrators are family members/caregivers that live with the abused/neglected/taken advantage of
1) List 6 types of elder abuse
Six types (one study’s breakdown of each):
- Physical abuse – 11%
- Physical / bodily injury
- Also includes over/under medication****
- Restraints
- Force-feeding
- Sexual abuse – 1%
- Any non-consensual (or incapacitated) sexual activity
- Can include physical/sexual advances, indecent exposure
- Emotional / psychological abuse – 15%
- Intentional infliction of suffering, pain, distress on someone with verbal/non-verbal means
- Demeaning comments, name calling, threats of deprivation/isolation/humiliation
- Neglect – 58%
- “Failure or refusal of caregivers to fulfill any of their duties or obligations to an elderly individual which HAS or IS likely to result in serious harm”
- Tough to prove
- Intentional infliction of suffering, pain, distress on someone with verbal/non-verbal means
- Abandonment
- Financial OR material exploitation – 15%
Many people experience multiple types of abuse
Three main categories where this may occur:
- Domestic elder abuse
- Happens in the home or caregivers home
- Institutional elder abuse
- Occurs in a residential facility
- Self-neglect / self-abuse
- The behaviour of the elderly person that threatens their own well being
- They fail to provide themselves with basic necessities: food, water, shelter, medications, personal hygiene
- ****This does not include mentally competent individuals who understand the consequences of their decisions****
- The behaviour of the elderly person that threatens their own well being
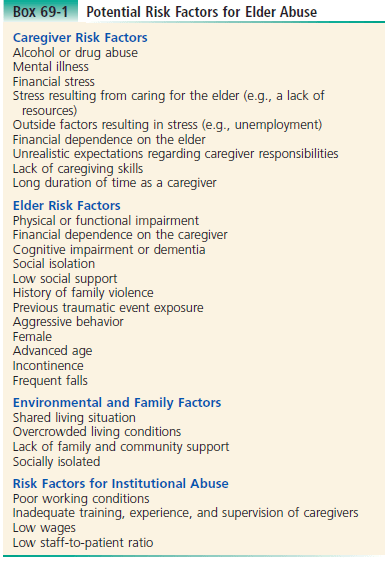
2) List 10 risk factors for elder abuse
Caregiver risks – promoting abuse; risk factors placing the elders for abuse; environmental factors; institutional abuse risks
3) List 10 questions to screen for elder abuse
- Very important to interview the caregiver and the patient privately!
- Must be non-judgemental and non-threatening
- “Caring for your mother/father must be a difficult task, do you ever feel anger or resentment toward them?”
- “What are some of the biggest stressors facing you?”
- Start off with basic questions including inquiry about daily care requirements, routines, medication and medication administration
- Must be non-judgemental and non-threatening
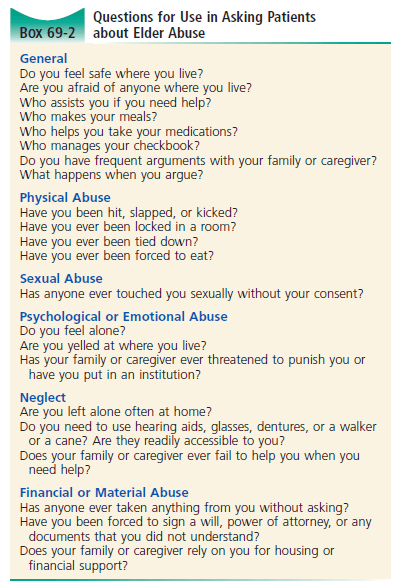
- Do you feel safe where you live?
- Who takes care of you?
- Have you been hurt by anyone who was supposed to take care of you?
- Does anyone force or bully you into giving them financial support or your money?
4) What are some indicators on the medical history and physical exam that may suggest ongoing elder abuse?
- This is where our pre-hospital friends can help us out:
- Identifying features of the patient’s home/family situation suggesting neglect or abuse (cleanliness, heat, water, infestations)
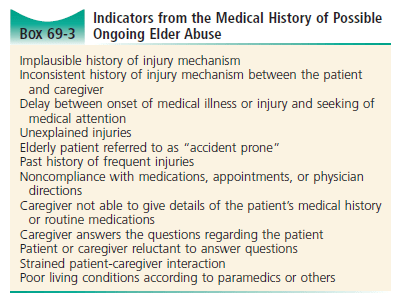
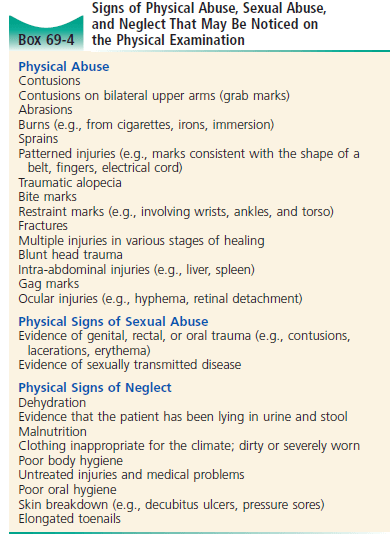
Thorough investigations should be ordered based on this history and physical examination.
Again, documentation is super important:
- Key things to note:
- Terms and descriptions used in the patient’s own words
- Include the mechanism of injury
- The social situation (living arrangements)
- Descriptions:
- Fractures, lacerations, contusions.
- Size, shape, location, colour
- Fractures, lacerations, contusions.
- Terms and descriptions used in the patient’s own words
5) Discuss ethical and legal implications of elder abuse. Who needs to be reported?
Again, the specific details of legal matters varies – in some states in the USA physicians are mandated to report any suspected case of elder abuse. It is very important to inform patients that you may have a requirement to report suspected cases of maltreatment before asking the screening questions.
Informing the patient that your goal is to end the abuse cycle AND help the patient and the family access resources; NOT punish the abuser.
In the great white north….
From Dr. Sampsel:
“We don’t have Adult Protective Services in Canada. Only mandatory reporting is for residents of nursing or retirement residences. If the patient does not wish to have any help and is capable of making that decision, we cannot do anything further.”
In summary for those of us in BC: check out the show notes below for more information!
[bg_faq_end]This post was edited and uploaded by Ross Prager (@ross_prager)