This episode of CRACKCast covers Rosen’s Chapter 66, Child Maltreatment. This episode covers an often overlooked but serious issue that presents to the ED and outlines the signs to look for when child injuries are suspicious for maltreatment.
Thank you to Dr. Sampsel for her assistance with this episode!
Shownotes – PDF Here
[bg_faq_start]Rosen’s in Perspective
Child maltreatment is an often overlooked entity presenting to our emergency departments.
Multiple entities: Physical abuse, sexual abuse, emotional abuse, child neglect (physical, emotional, educational), and factitious disease by proxy / aka Munchausen syndrome aka medical child abuse
We have an ETHICAL and LEGAL obligation to investigate and report all potential child maltreatment to the authorities.
In British Columbia, this entity is Child Protection Services, and our legal legislation is the Child, Family and Community Service Act, (24hr hotline: 1-800-663-9122)
Although we are mainly focused on determining intentional versus unintentional injury versus underlying medical pathophysiology, the hallmarks of intentional or non-accidental trauma in children are: cutaneous bruises, burns, skeletal fractures, internal hemorrhage, organ perforation, and brain injury (coup-contrecoup/SAH/SDH/DAI)
Remember, accidental bruising tends to be over bony prominences: think forehead, elbows, shins, bruises over the neck, medial thighs, behind the ears are all suspicious.
“Those kids who don’t cruise, don’t bruise”
Other injury patterns to look out for are bruising patterns (belts, cords, shoe imprints), bites (children have <2.5cm between canine incisors vs adults have >3cm) and burns (immersion, cigarette, iron, chemical). Note: Accidental burns are usually spill pattern: severe proximal to coffee pot etc, milder more distal and have spill pattern (drip appearance). Versus immersion burns (glove stocking distribution).
[bg_faq_end][bg_faq_start]1) List 5 high risk fractures for child abuse

Metaphyseal fractures:
- Due to pulling on an extremity
- Heal without a bony callus
- Usually in kids < 2 yrs old
Pearls:
- Kids don’t usually get rib fractures during CPR
- long bone fractures in pre-ambulatory kids are suspicious
- Infants usually can’t roll over until 3 months (at the earliest)
2) What is your DDx for intentional injury?
Unintentional injury!
- Trauma from falls, primary medical conditions (leukemia, coagulopathy, osteogenesis imperfecta, etc.)
3) List 6 DDx for physical abuse and 6 DDx for sexual abuse
Physical:
- ALTE (now known as….BRUE)
- Seizure
- Intestinal injuries (eg bike handle)
- Pancreatitis (commonly drug induced when not intentional trauma)
- Liver / spleen injury
- Underlying coagulopathy familial – acquired or leukemia
- Glutaric aciduria type I (causing ICH)
- Osteogenesis imperfecta
Sexual:
- Accidental trauma (straddle injury)
- Hymen remains uninjured
- dermal melanocytosis (formerly called mongolian spots),
- lichen sclerosus atrophicus
- Unknown cause – hypopigmentation with adjacent skin developing blood blisters and petechiae
- Hymen is unaffected
- May involve the anus or perihymenal areas
- Impetigo,
- Urethral prolapse
- Usually african american girls aged 5-8 yrs
- Should get urology consultation for ligation
- Anal fissures
- Infectious causes:
- STI’s
- Shigella
- Group A beta-hemolytic strep – causing perianal strep infection
- Candida
- Pinworm infestation
- Chigger infestation
- Vaginal foreign bodies
- Priapism (due to sickle cell disease)
- Usually african american girls aged 5-8 yrs
4) What are some conditions that may mimic child abuse?
Rashes:
- Phytophotodermatitis
- Due to a phototoxic reaction that develops on sun-exposed areas that have been in contact with fruit juices
- Appearance: erythema, blistering then becoming brown skin rashes
- Dermal melanocytosis (formerly called mongolian spots)
- Bullous impetigo
- Confused with second degree burns
- Due to a phototoxic reaction that develops on sun-exposed areas that have been in contact with fruit juices
Trauma:
- Unintentional burns
- Accidental fractures (eg clavicle or humerus at birth, Toddlers # (aka. CAST fracture))
- Osteogenesis imperfecta
- 1:20000 incidence; multiple types of it
- Look for blue sclerae
- Brownish teeth
- 1:20000 incidence; multiple types of it
Deficiencies:
- Rickets of prematurity
- Scurvy
Infections:
- Congenital syphilis / rubella
- Encephalitis / Meningitis / Post hypoxic edema
5) What cluster of injuries is seen in shaken baby syndrome?
- Head trauma
- Traumatic axonal injury → cerebral edema
- With retinal hemorrhages (85% of cases have this)
- “Due to vitreo-retinal traction due to centrifugal forces”
- Seen as dot, blot, shear and flame hemorrhages
- Skeletal injuries
- Abdominal injuries: *there may be no visible external signs of trauma*
- Pancreatitis
- Liver and spleen lacerations
- Duodenal hematomas / viscus perforations
**Can have no scalp hematoma or skull fractures**
 |  |
 |  |
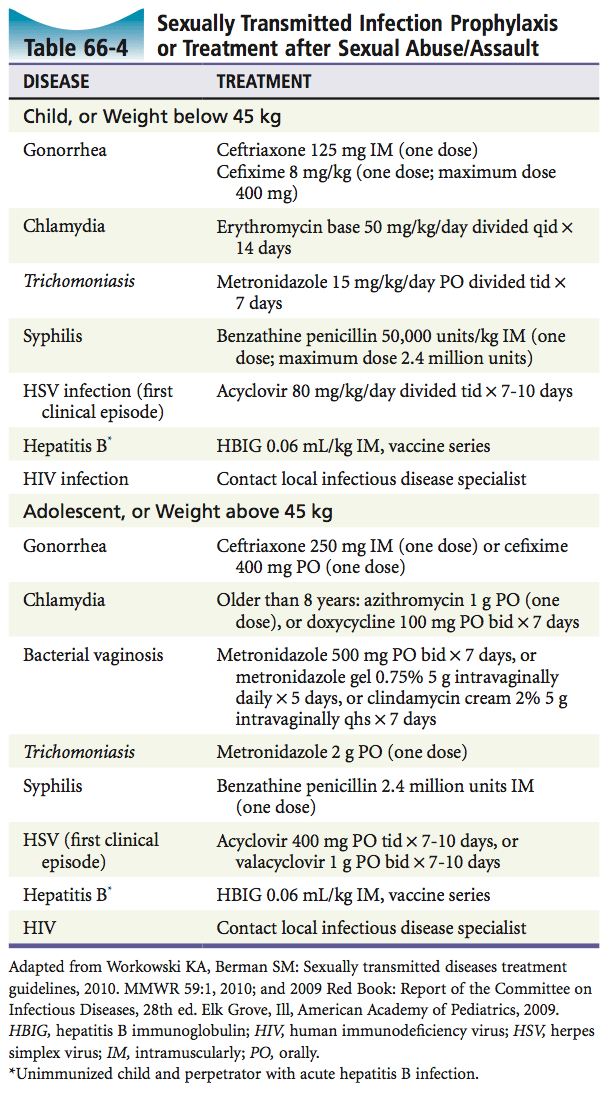
6) List 6 diseases that may require prophylaxis in child sexual abuse and the drugs with dosage that you would use above and below 45kg?
- In cases of acute assault Rosen’s mentions that the pubertal patient should be prophylactically treated for gonorrhea, chlamydia, and trichomoniasis
- Pre-pubertal children are at much lower risk of contracting an STI; so they can be followed clinically
This post was uploaded and copyedited by Colin Sedgwick (@colin_sedgwick)


