This episode of CRACKCast covers Chapter 56 of Rosen’s Emergency Medicine, Hip and Femur. This episode reviews the anatomy, pathophysiology, and management of both common and uncommon hip injuries that may present to the emergency department. As well, we would like to thank everyone who tunes in and supports our podcast. We wish you all the best in 2017!!
Shownotes – PDF Here
[bg_faq_start]Rosen’s In Perspective:
- Hip #’s account for 70% of the medical costs associated with fractures!
- 4:1 women to men
- Mostly osteoporotic, postmenopausal women
- May also affect 2-14 yr olds
- Perthes disease
- AVN of the femoral head (more common in boys)
- Slipped capital femoral epiphysis (SCFE)
- Peaks at 13.5 yrs (more common in boys!)
- Anatomy
- Features:
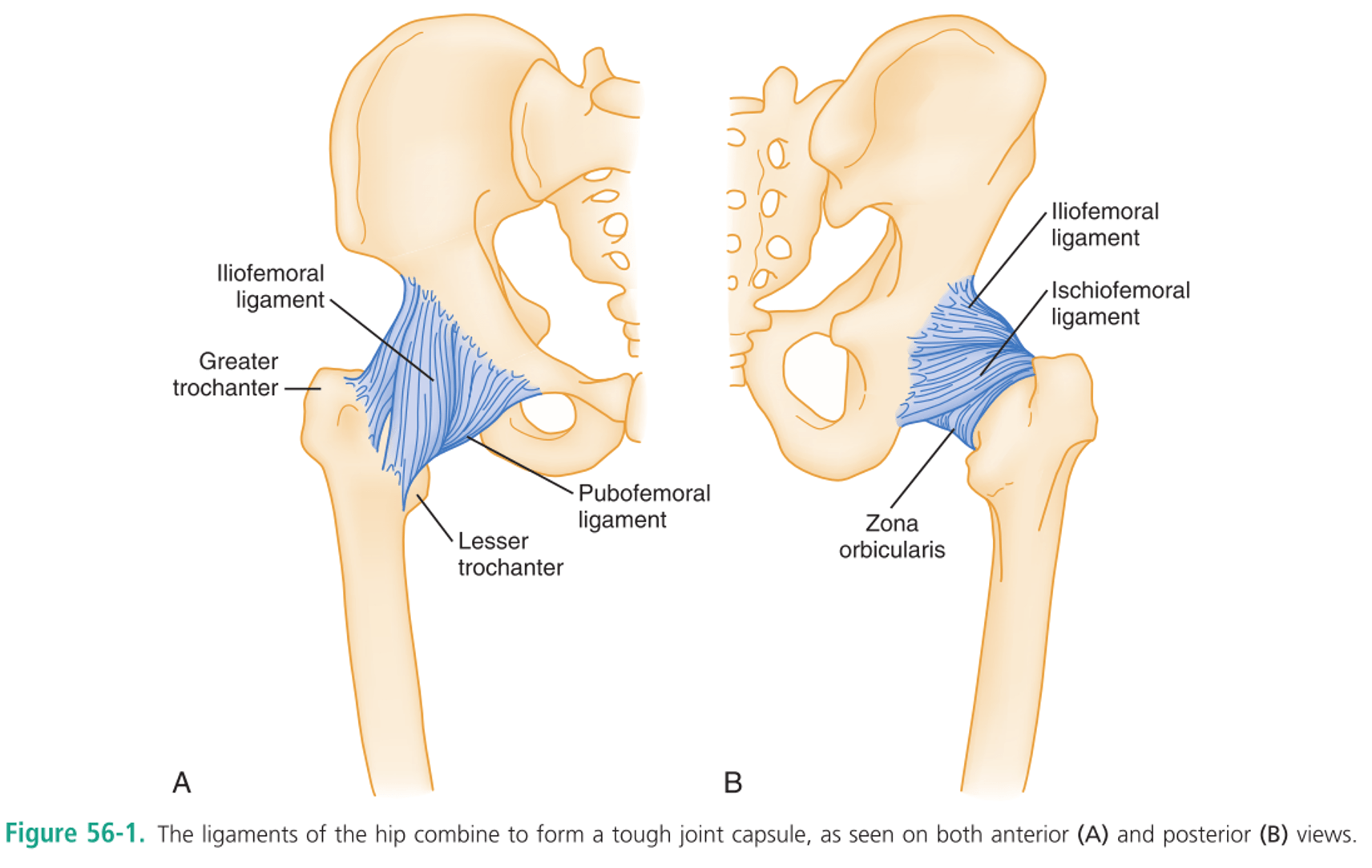
- Hip joint capsule wrapped in tough iliofemoral/pubofemoral/ischiofemoral ligaments
- Features:
- Perthes disease
- Bony architecture:
- Femoral head / neck / greater trochanter / lesser trochanter / intertrochanteric / shaft

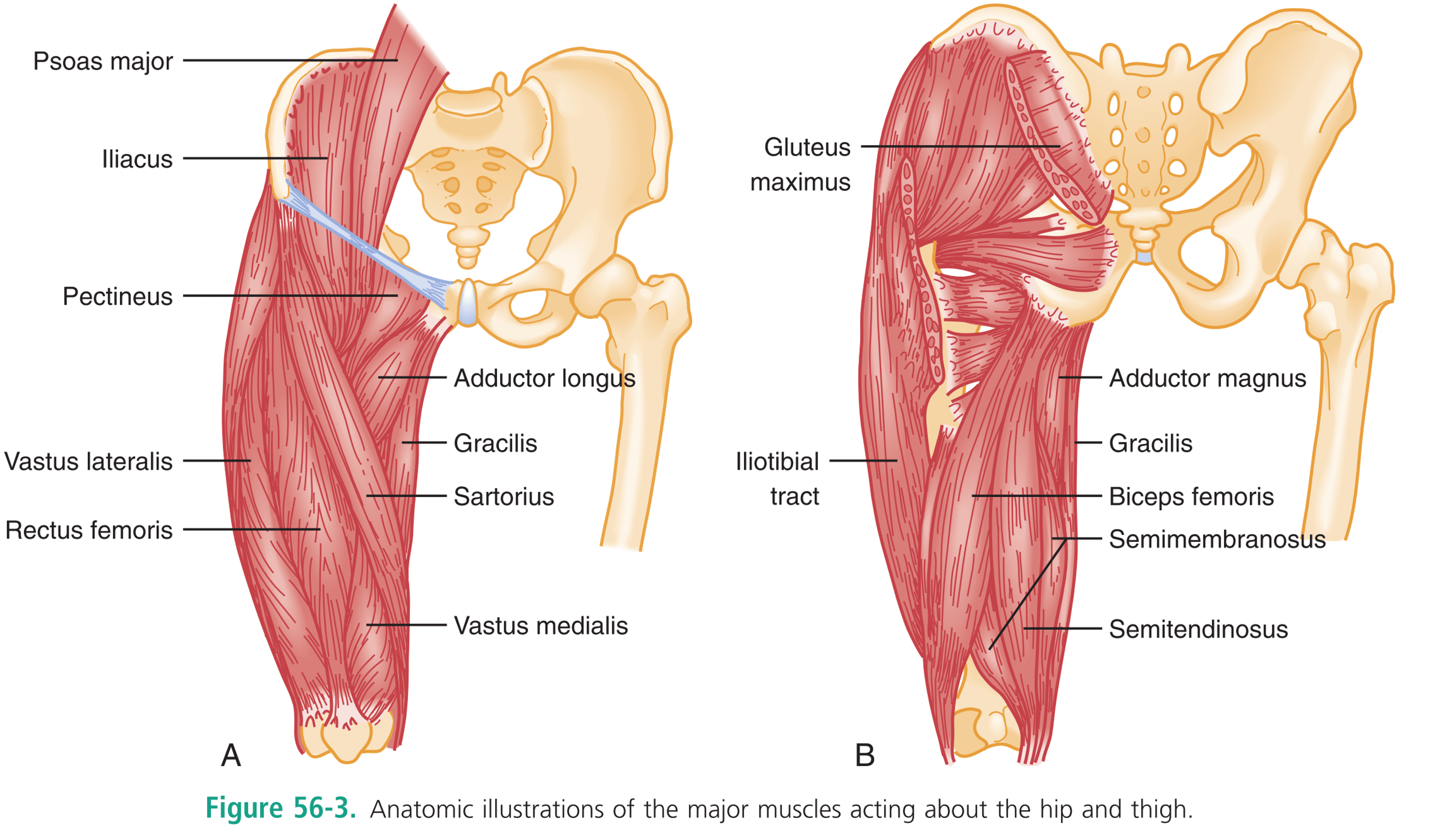
- Muscles of the thighs
- Quads
- Vastus lateralis, rectus femoris, vastus medialis, sartorius
- Adductors
- Adductors longus, gracilis, pectineus
- Hamstrings
- Biceps femoris
- Semimemb/semitendinosus
- Abductors
- Quads
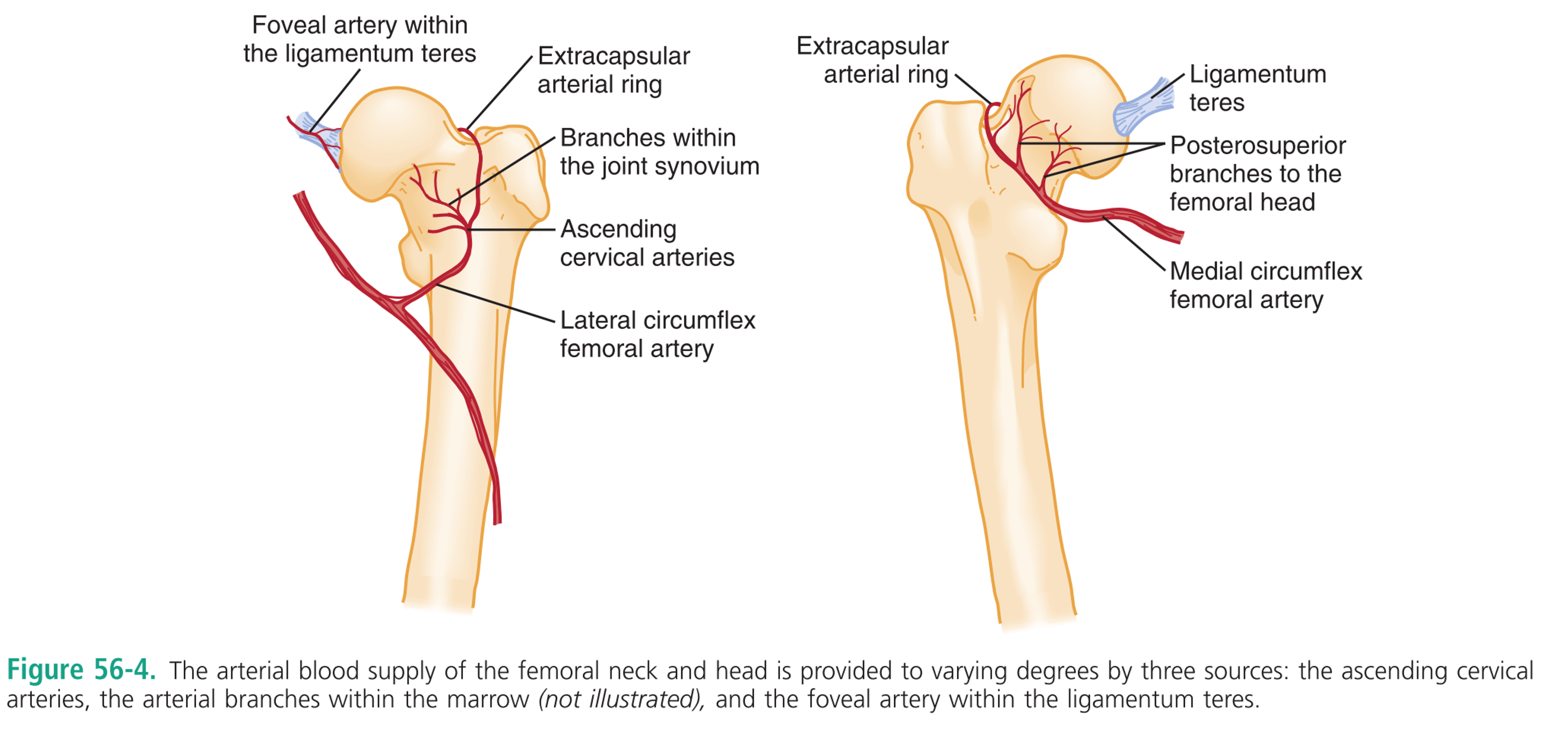
- Arterial supply to the femoral head
- Ascending cervical arteries
- Intraosseous cervical vessels
- Foveal artery (in the ligamentum teres)
- Venous system
- Nerves
- Femoral
- Branches off the lumbar plexus
- Sciatic
- Largest peripheral nerve in the body
- Arises from the sacral plexus
- Extends from the inferior border of the piriformis
- Innervates the adductors and hamstrings
- Pathophysiology
- Hip fractures:
- 20% of people die in the year after a hip # due to osteoporosis
- Hip osteoarthritis
- Hip fractures:
- Femoral

- Hip radiography:
- Three methods
- Shenton’s line
- Normal S and reverse S curves
- Trace the trabecular lines
- 2-10% of hip fractures are radiographically occult
- MRI is the gold standard
- CT has a 66% misdiagnosis rate compared with MRI!
- Three methods

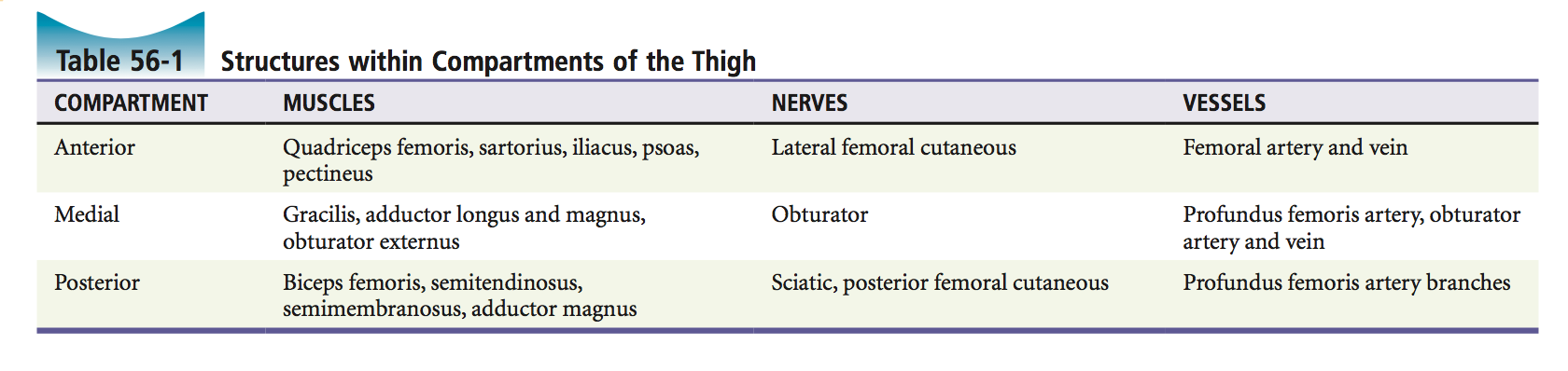
1) List 3 compartments of the leg and their contents
2) List 8 causes of Avascular Necrosis (traumatic and atraumatic)
- High suspicion for anyone with increasing atraumatic hip, buttock, thigh, knee pain
- Aka:
- Osteonecrosis, ischemic necrosis
- May be bilateral in 40-80% of cases
- Mean age 38 years
- Risks:
- Atraumatic:
- Chronic corticosteroid use
- Chronic ETOH abuse
- Sickle cell anemia
- Dysbarism
- Chronic pancreatitis
- HIV
- Traumatic:
- Post-hip dislocation
- 5% if reduced in 6 hrs, 50% if reduced in 12 hrs
- Post-femoral neck fracture
- Athlete with an energy deficit or overtraining
- Post-hip dislocation
- Atraumatic:
- Risks:
3) List the 5 most common primary cancers that metastasize to bone
- Breast
- Kidney
- Lung
- Thyroid
- Prostate
Memory aid: “The double organs”
[bg_faq_end][bg_faq_start]4) List 15 causes of hip pain without an obvious fracture
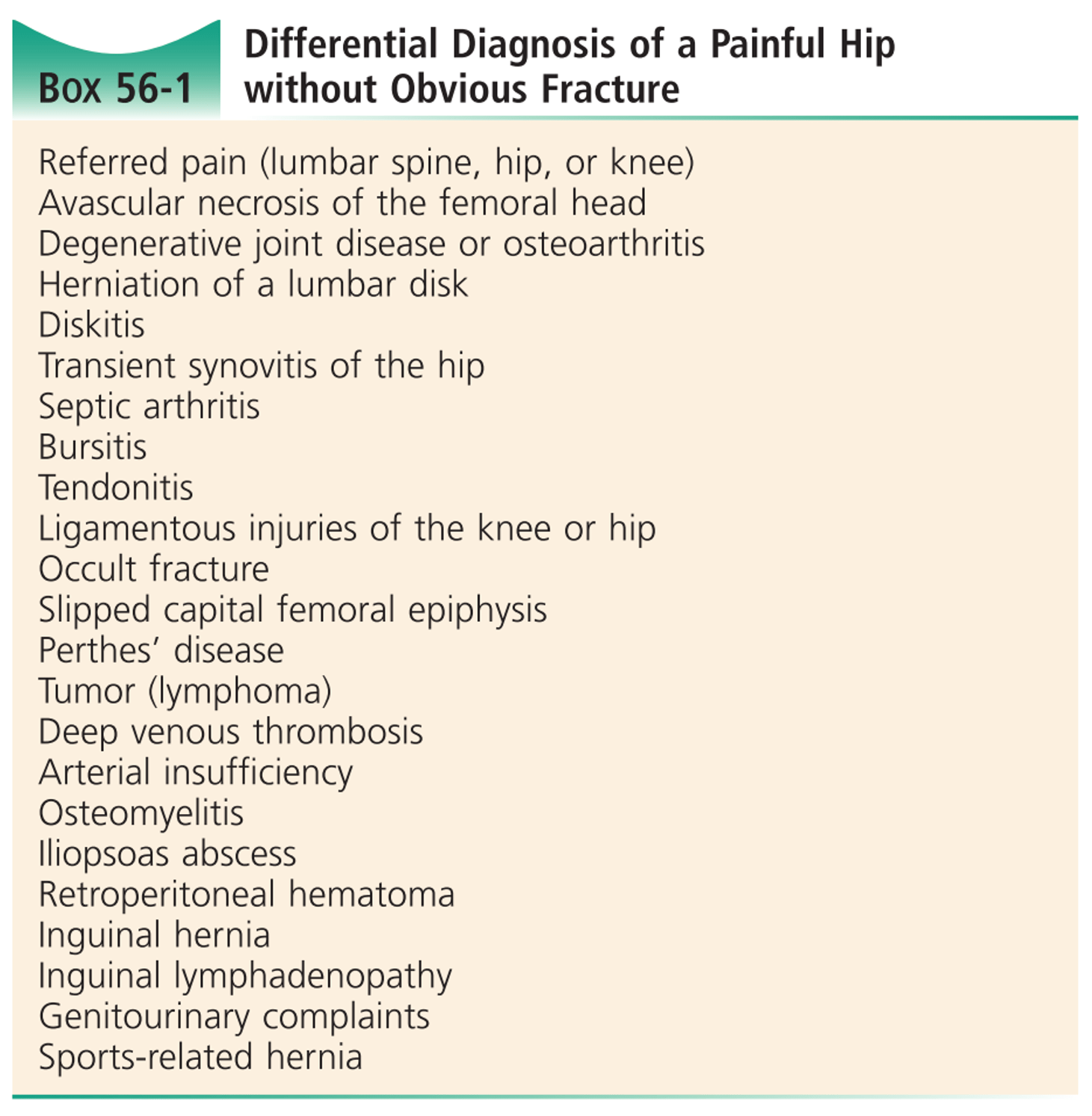
- Referred pain – lumbar/spine/knee
- Diskitis
- Lumbar disk herniation
- Knee pathology
- Hip bone pathology
- AVN of the femoral head
- Perthes disease / SCFE
- Occult fracture
- Bone tumour
- Osteoarthritis
- Transient synovitis / septic joint / osteomyelitis
- Hip soft tissue pathology
- Bursitis
- Iliopsoas abscess
- DVT
- Arterial insufficiency
- Abdominal pathology
- Inguinal hernia
- Retroperitoneal pathology
- PID
- Nephrolithiasis
- GU pathology
- UTI
- Testicular torsion
- External genitalia abnormalities
- Sports med stuff
- Sports hernia
- FAI
- Labral injury
- Osteitis pubis
5) List 6 techniques for closed reduction of the hip
- Huge force is needed to dislocate the hip – so look for a # (70% of the time) and other multi-system injuries
- Examination:
- Posteriorly – internally, flexed, adducted hip (knee rests on opposite thigh)
- Anteriorly – externally rotated, abducted, slightly flexed hip (leg appears longer)
- Focus on the sciatic nerve and the femoral vessels
- – Weakness of the extensor hallucis longus
- – Weakness of foot dorsiflexion
- – Numbness over the dorsum of the foot
- Diagnosis:
- AP view of the pelvis will identify most dislocations
- Subtle signs:
- Loss or accentuation of the lesser trochanter
- Asymmetric view of the femoral head
- Loss of Shenton’s line
REDUCTION TECHNIQUES (posterior dislocations):
- This is a true emergency – they need reduction within 6 hours
- Biggest limiting factor is the overall condition of the patient
- Use deep procedural sedation
- A femoral neck fracture may be a relative contraindication to reduction
- Allis technique
- Supine, pelvic counter-traction force into the stretcher
- Knee and hip flexed partially
- Steady upward traction on the hip/knee while flexing to 90 degrees and gently rotating the hip
- With the captain morgan technique

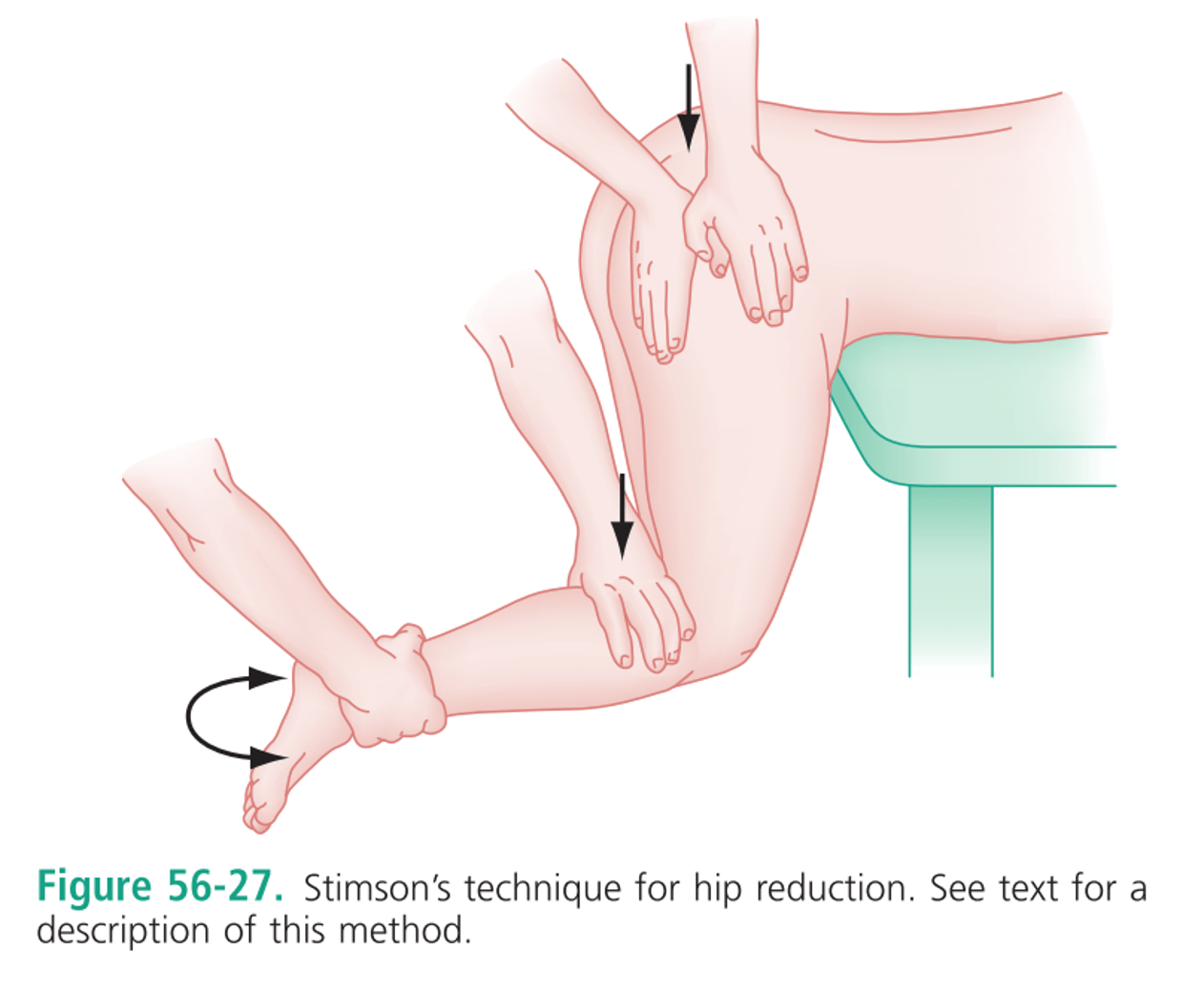
- Stimson’s technique
- Similar to the shoulder Stimson’s technique – need the person lying prone with their pelvis hanging over the edge of the bed
- Whistler method
- Uses your extended arm, and your legs to shift a posterior dislocation forward
- Flex the patient’s unaffected leg at the knee
- Flex the knee on the affected side, slide your arm underneath placing your hand on the knee on the unaffected side, and use this as the fulcrum
- Lift with your legs (avoid lifting with your back!)
- Gently internally/externally rotate the affected hip whilst lifting
- Ensure you have an assistant placing downward pressure on the pelvis/ASIS
From: http://edprocedures.com/hip-reduction-whistler-technique/
- Rochester method (similar to Whistler method)
- Patient is placed supine with uninjured hip and knee flexed (this knee acts as a pivot point for the surgeon’s hand);
- One of the surgeon’s hands is place underneath the injured knee and over top of the uninjured knee;
- This manuever flexes both the patient’s injured hip and knee;
- The other hand grabs the ankle (injured side) and this can be used to generate traction (by pressing down on ankle) and at the same time the ankle can be used to control hip rotation;
- Reduction is obtained by traction, internal rotation, and then external rotation once the femoral hip clears the acetabular rim;
From: http://www.wheelessonline.com/ortho/closed_reduction_of_posterior_hip_dislocation
- Traction-countertraction method
- And many others
See: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4821229/ for an exceptional list of 12 different techniques with figures
Pitfalls:
- Acetabular/femoral head fragments may obstruct the reduction
- Even more reason to consider CT imaging
- Assess stability by gently moving the hip through a ROM – to see if it re-dislocates
- Must carefully inspect post-reduction radiographs to ensure full reduction, consider getting a CT
- At high risk for AVN long term
The hip prosthetic dislocation:
- Increasingly common
- May occur within the first 3 months or up to 10 years post
- Usually posterior dislocations, and may occur with trivial activity
- No risk for femoral head AVN (if they have a prosthetic head!)
- Be sure to assess for sciatic nerve injury
- Most orthopods should be notified
6) Describe 4 types of hip dislocation
- Usually dislocated (in relation to the acetabulum):
- 80-90% = Posteriorly – internally, flexed, adducted hip (knee rests on the opposite thigh)
- MVC (dashboard forces on the flexed abducted hip)
- 10-15% = Anteriorly – externally rotated, abducted, slightly flexed hip (leg appears longer)
- Forceful extension, abduction & external rotation of the femoral head
- MVC’s or hyperextension during a fall
- May also be:
- Obturator dislocation – towards the obturator foramen
- Pubic dislocation – towards the pubis
- 2-4% = Central dislocation
- Femoral head is pushed through a decimated acetabulum
- Luxatio erecta femoris
- Forceful extension, abduction & external rotation of the femoral head
- 80-90% = Posteriorly – internally, flexed, adducted hip (knee rests on the opposite thigh)
Wisecracks
[bg_faq_start]1) Pediatric hip and femur pathology
a) Hip dislocations
- Growth centres in the pediatric hip – lead to high risk of growth arrest with hip trauma
- Much of the pediatric hip is radiolucent – so don’t only focus on the ossified centres
- Small children are at higher risk of hip dislocations than femoral neck fractures (less developed acetabulum)
- “In a school-aged child athletic injuries are the major cause of traumatic hip dislocations”
b) Classification of femur fractures
- Hip and femur fractures:
- From high-energy, violent trauma
- Hip fractures are NOT classified using the Salter-Harris
- Delbet classification system:
- physis
- transcervical area
- cervicotrochanteric
- intertrochanteric
- Femur fractures:
- Spiral shaft fractures should prompt consideration for NAT and pathologic fractures (bone cyst, fibrous dysplasia, osteogenesis imperfecta, malignancy)
- Femur fractures:
- Delbet classification system:

c) Describe 6 causes of limp in a child
- Child with a limp:
- Must assess back, hip and knee!
- Etiologies:
- Inflammation / infection – look for a joint effusion on ultrasound
- Transient synovitis
- Non-bacterial inflammatory clinical entity
- Usually boys 3-10 yrs old
- Septic arthritis
- KOCHER criteria:
- http://www.mdcalc.com/kocher-criteria-septic-arthritis/
- Temp > 38.5 in the preceding week
- Non-weight bearing status
- ESR > 40 mm/hr
- WBC > 12k
- 2% if none, 10% if one, 35% if two, etc.
- CRP also useful
- Often need aspiration, bone scans, CT, MRI
- KOCHER criteria:
- Osteomyelitis
- Usually Staph.
- Salmonella in kids with Sickle cell disease
- Viral and rickettsial disease may present sub-acutely
- X-ray findings don’t appear until 2-3 weeks of illness
- Juvenile rheumatoid arthritis
- SLE
- Tuberculous arthritis
- Transient synovitis
- SCFE
- “Ice-cream scoop slip”
- Important to get AP and frogleg views – the femoral epiphysis must be symmetrical on all views bilaterally
- Klein’s line = line drawn along the superior margin of the femoral neck should intersect some part of the femoral head
- Boys > girls, usually age 10 yrs
- Progressive disease over weeks/months with eventual constant knee/hip/thigh/groin pain
- Abducted externally rotated thigh, partially flexed (biggest joint capsule space)
- Perthes disease
- AVN of the femoral head
- Peaks at 6 years of age, boys >> girls
- Unilateral, painless limp → then progressively painful
- Avulsion injuries
- Leading to isolated # of the lesser/greater trochanter
- Greater trochanter = hip abductors (gluteus medius, piriformis, quadratus femoris, etc).
- Lesser trochanter = iliopsoas
- Surgery for > 2 cm displacement
- Early mobilization as tolerated
- Leading to isolated # of the lesser/greater trochanter
- Inflammation / infection – look for a joint effusion on ultrasound
This episode was edited and uploaded by Colin Sedgwick (@colin_sedgwick) and Ross Prager (@ross_prager)



