This episode of CRACKCast covers Rosen’s Chapter 55, Pelvic Trauma. These patients can decline quickly from blood loss, so recognition and determining injury severity early is important to stabilize them.
Shownotes – PDF Link Here
[bg_faq_start]Rosen’s in Perspective
- Key message: be scared! Patients can easily exsanguinate into their pelvis from pelvic ring fractures
- Also requires large amount of force – look for other injuries
- Epidemiology:
- Primarily result from MVCs and ped struck trauma.
- Less commonly (5-10%) falls from height
- Mortality is 9-22% – independent predictor of death
- Anatomy
- Complex structure, but at the core is a ring protecting visceral components (GI tract, vasculature, nerves)
- Major components of stability: posterior arch (weight bearing), symphysis pubis anteriorly.
- Unstable ring fractures mostly due to disruption of ligaments of posterior arch.
- Vascular
- Lots of vascular structures! Internal and external iliac arteries.
- Superior gluteal artery commonly injured in posterior arch fractures.
- Obturator and internal pudendal arteries commonly injured in ramus fractures.
- Veins form venous plexus and have no valves and adhere closely to pelvic walls – can hemorrhage easily and are not compressible.
- Neurologic
- Cauda equina in sacral spinal canal
- Injury to posterior pelvis/sacrum can cause lower neurologic deficits & autonomic dysfunction
- Check rectal tone, post-void residual, etc.!
1) Describe common pelvic fractures and their classification
- It can be useful to consider both types of classification (stability as well as mechanism)
- Key is underlying principles of stability and co-injury over detailed specifics.
- Broad classification: stable vs. unstable fractures
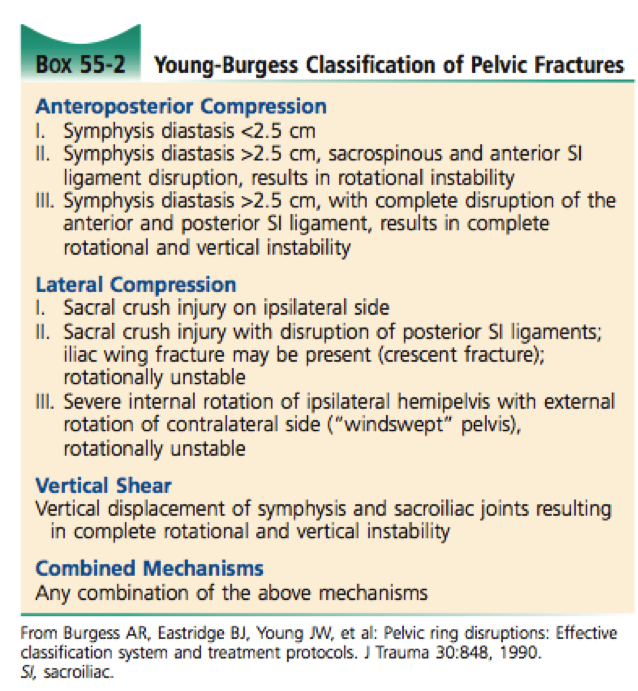
Young-Burgess classification
- Based on mechanism of injury
- Anterior-Posterior Compression (APC)
- APC I: symphysis < 2.5cm (stable)
- APC II: symphysis > 2.5cm, SI disruption (partially stable)
- APC III: symphysis > 2.5cm, SI shearing (completely unstable)
- Lateral Compression (LC)
- LC I: ipsilateral sacral crush injury (stable)
- LC II: ipsilateral sacral crush injury, disruption of posterior SI ligaments, possibly iliac wing fracture (partially unstable)
- LC III: internal rotation of ipsilateral hemipelvis with external rotation of contralateral hemipelvis (‘windswept pelvis’) (partially unstable or completely unstable)
- Vertical Shear (VS)
- Vertical displacement of symphysis and JI joints
- ALWAYS UNSTABLE
- Combined Mechanism (CM)
- ALWAYS UNSTABLE
Tile classification
- Type A, B, and C (C is worse)
- All about rotational (hinging pelvis) stability and vertical (shearing) stability
A – Stable Injuries
- Rotationally and vertically stable
- Fracture of bones outside the pelvic ring itself.
- Avulsion fractures
- Athletic injury, sudden forceful muscular contraction
- Common in older children/teens – physeal avulsion
- Ischial tuberosity, iliac crest epiphysis, ASIS
- Can avulse AIIS from kicking (rectus femoris contraction) but can also be normal os acetabuli.
- Conservative treatment, surgery rarely needed
- Isolated iliac wing fracture
- Inferior public ramus fracture
- Transverse sacral or coccyx fracture
- Mechanism:
- Forced flexion
- Fall from height
- Below S4 unlikely to result in neurologic injury
- Treated conservatively
- Above S4 common neurologic injury
- Need careful neurologic exam and surgical referral
- Undisplaced fractures of the pelvic ring
- Be careful and always search for second ring fracture
- Commonly isolated fracture of inferior and superior pubic ramus
- If displaced – look for another fracture!
- Fracture of both rami on ipsilateral side can be associated with unrecognized impaction fracture of posterior pelvis
- Get a CT if clinically any posterior pelvic pain or instability
- In one study, 95% of elderly patients with isolated ramus fracture had sacral fractures on MRI!
- Lateral compression mechanism (Young-Burgess I) associated with 7% mortality
- Four-pillar fractures of both pubic rami on both sides (“butterfly segment”)
- Straddle mechanism – direct blow to symphysis
- High rate of concomitant injuries – Computer Tomography
- High rate of injury to GU tract
- Mechanism:
- Avulsion fractures
B – Partially Stable
- Rotationally unstable, vertically stable
- High energy impacts – mechanism determines injury types
- B1: Open book fracture
- Typically from AP force
- Radiology:
- Symphysis widening > 2.5cm
- Widening of SI joints
- Can have severe vascular & neurologic compromise
- Complete separation of hemipelvis from shearing (vs. hinging of SI joint) is completely unstable (Tile C) – need CT to tell.
- B2: ‘Closed book fracture’
- Typically from lateral compression
- Overriding of pubic symphysis (internal rotation of hemipelvises)
- Decreases volume of pelvis, typically associated with less blood loss than AP injuries
C – Unstable
- Rotation unstable, vertically unstable
- Result from vertical shearing force on the pelvis
- g. fall from height, ‘submarining’ under dashboard
- SI joint has been disrupted from vertical shearing force
- Look for avulsion of ischial spine, avulsion of lower lateral lip of the sacrum, and injury to L5 transverse process on radiology – all insertion sites of important ligaments
- Potential for large volume blood loss, significant hypovolemia, PEA arrest
- C1 – unilateral
- C2 – bilateral
- C3 – bilateral with involvement of acetabulum
- Remember – vertical fractures of the sacrum count as well – transverse do not (orientation to the pelvic ring is different)
- Denis classification (see later)
Denis classification
- Classification of vertical sacral fractures
- Higher numbers are worse in terms of potential for neurologic injury and pelvic instability
- Denis I – lateral to sacral foramina
- Denis II – through sacral foramina
- Denis III – medial to sacral foramina, involving spinal canal
2) List 3 categories of complications of pelvic fractures
- Associated injuries
- Urologic
- More common in men, anterior pelvic fractures
- Check for blood at the meatus
- Retrograde urethrogram to check for urethral injury
- Don’t forget bladder can be injured as well.
- Neurologic
- Worse with worsening instability (Tile A < B < C)
- Worse with more medial vertical sacral fractures (Denis I < II < III)
- Cauda equina possible
- Gynecologic
- Can have open pelvic fracture into vagina
- Look for blood at introitus
- Careful manual examination
- Gastrointestinal
- Open pelvic fracture into GI tract
- High risk of infection
- Careful digital internal examination
- Urologic
- Hypovolemia/shock
- Can easily lose 10-15 units of blood volume into pelvis
- Consider in trauma patients in PEA
- APC had highest average transfusion requirements (15 units), VS next (9 units), LC least (4 units)
- Infection
- Open pelvic fractures can be occult and open into “dirty” areas such as GI tract of vaginal vault
3) Describe the approach and management of hemodynamically unstable pelvic fracture
- Access -> stabilize -> control hemorrhage -> resuscitate with blood -> definitive treatment
- Ensure excellent IV or central access above the pelvis
- Consider early activation of massive transfusion protocol
- Typical to require 10 – 20 units of pRBCs in first 24 hours
- Do not delay definitive treatment in order to attain normotensive vitals
- Bind/stabilize pelvis with sheet or pelvis binder
- Consider requesting orthopedic external fixation of pelvis
- Recently some articles published about REBOA (resuscitative endovascular balloon occlusion of the aorta)
- Trained ED physicians only! Still experimental
- Balloon catheter threaded into thoracic aorta and inflated to occlude lower body perfusion
- Prevents further hemorrhage, increases afterload and brain perfusion
- See Qasim et al., 2015 for excellent review (http://emcrit.org/wp-content/uploads/2016/03/REBOA-Review.pdf)
- Also successfully performed prehospital by London HEMS!! What a bunch of bad asses (Sadek et al., Oct. 2016 – http://www.resuscitationjournal.com/article/S0300-9572(16)30136-8)
- Assess for associated injuries
- Patients with both retroperitoneal hemorrhage from pelvic fracture and intrabdominal hemorrhage have a mortality rate of 40%
- Make sure to involve ortho, general surgery, and interventional radiology in planning approach for whether to go to OR for pelvis or abdomen first, or combined setup.
- Ortho may also place pelvic packing during laparotomy
- Remember: pelvic injuries bleed into retroperitoneal space, but FAST exam looks at intraperitoneal space. False-negative FAST exam has an odds ratio of 3.5 in patients with pelvic trauma! Don’t rely on it!
- Rosens talks about DPL… yeah no.
- Patients with both retroperitoneal hemorrhage from pelvic fracture and intrabdominal hemorrhage have a mortality rate of 40%
- Angiography and embolization for suspected arterial bleeds
- Orthopedic referral
4) List 5 radiographic clues to posterior arch fractures
- This is box 55-3 in Rosens
- Avulsion of L5 transverse process
- Avulsion of ischial spine
- Avulsion of lower lateral lip of the sacrum
- Displacement at the site of a pubic ramus fracture
- Asymmetry or lack of definition of bony cortex at the superior aspect of the sacral foramina
5) What is the management of penetrating pelvic trauma?
- Complex anatomy, very high likelihood of visceral, vascular, and/or neurologic injury
- Overall mortality is 6-12%
- All cases of penetrating pelvic trauma should have emergent surgical consultation and should be covered with broad spectrum antibiotics
- DRE is important to assess for injury to the rectum.
Wisecracks:
1) How are open pelvic fractures diagnosed and managed?
- Important to look for occult open fractures
- Can be intravaginal, intrarectal
- Look for blood at introitus, injury to the perineum or gluteal region, and make sure to perform a DRE and vaginal examination
- Be careful with internal exams in order to not lacerate finger on bone fragments
- Active bleeding can be controlled with direct pressure
- Cover early with broad spectrum antibiotics and anaerobic coverage
2) What is the classification of acetabular fractures?
- Finally! A universal classification!
- Type A – anterior or posterior column fracture
- Posterior more common
- Forceful impact to flexed knee (dashboard injury)
- Anterior less common
- Extension of superior ramus fracture into acetabulum
- Posterior more common
- Type B – anterior and posterior column, segment of acetabulum still attached to ilium
- Often T-shaped fracture
- Type C – anterior and posterior column, no segment of acetabulum still attached to ilium
- All of these need CT and orthopedic referral
3) How are coccygeal fractures managed?
- Conservatively!
- Rest
- Analgesia
- Sitz baths
- Stool softeners
- If ongoing intolerable pain, can consider non-emergent orthopedic referral for local steroid injection or coccygectomy
This post was uploaded and copyedited by Riley Golby (@RileyJGolby)