This post has been co-written by Drs. Kathy Boutis and Maxim Ben Yakov.
The dogmas of the past are now being challenged for the most common minor pediatric fractures, distal radius buckle fractures and minor distal fibular fractures. Since these fractures are stable and have an excellent prognosis, they do not need to be routinely immobilized in a cast nor followed by an orthopedic surgeon. This article reviews the evidence that recommends that management of the distal radius buckle fracture.
Distal Radius Buckle Fractures
Buckle fractures of the distal radius represent about 50% of pediatric fractures of the wrist.1
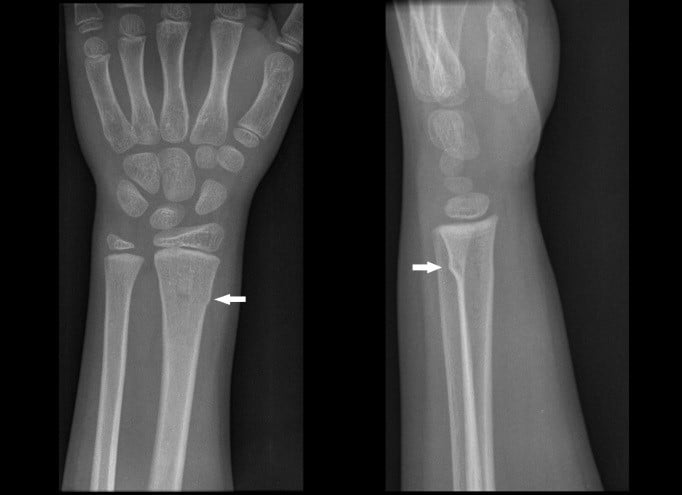
Figure 1: Buckle Fracture of the Distal Radius
The cosmetic and functional prognosis of this fracture is excellent even if it associated with an ulnar buckle/styloid fracture.2,3 Data from eight randomized control trials conducted in the UK, Canada and the US has demonstrated that treatment with a removable splint is at least as effective as a short arm cast with respect to recovery of physical function.4 Further, these RCT’s demonstrated that parents and families preferred the removable splint, and splinting was found to be more cost-effective for the health care system.
Treatment with immobilization with a removable splint is used as needed to reduce pain and to protect against re-injury. The duration of splint use and return to play should be guided primarily by pain and the degree of buckle fracture noted on the x-rays. Most children use the splint regularly for two to three weeks and about 99% are fully recovered by four weeks.2 Activities that could lead to re-injury should be avoided until the child has been free of symptoms for two weeks (about 6-8 weeks from time of injury). Follow-up with an orthopedic surgeon is not routinely necessary and these children can be safely followed up with a primary care physician.3,5,6 An orthopedic surgeon should be consulted if the child’s condition is not improving over time or the child has not fully recovered by six weeks.
The key caveat is to ensure that the radiological diagnosis of distal radius buckle fracture is correct. Radiographs should be scrutinized for other diagnoses since minimally displaced greenstick and Salter–Harris II fractures of the distal radius may be mistaken for buckle fractures6. These injuries require rigid immobilization and orthopedic consultation.
Figure 2: (A) Salter-Harris II distal radius; (B) Greenstick of distal radius
References
Reviewed by Drs. Brent Thoma and Teresa Chan. This post has been copyedited and uploaded by Sonja Wakeling (@SonjaWakeling).




