You are working an overnight shift in the emergency department when a 40 year-old male passenger involved in a high-speed motor vehicle collision arrives. His vital signs include a blood pressure of 88/56 mmHg, heart rate of 112, and respiratory rate of 16. His Glasgow coma score is 12 (3E, 4V, 5M). En route, your patient received 2L of normal saline with no change in his blood pressure. On exam, his abdomen is tender in the and his pelvis feels stable, but he becomes increasingly confused after your exam. After the team has intubated the patient, you notice the medical student has wheeled the portable ultrasound machine into the trauma bay. He hands you the probe expectantly.
The Question
In the adult patient with blunt abdominal trauma, what is the role of the Focused Assessment Sonography in Trauma (FAST) examination?
The FAST Exam
The FAST exam is a useful diagnostic test for adult trauma patients that present with possible abdominal injury. The Canadian Association of Emergency Physicians (CAEP) has endorsed FAST as a point-of-care ultrasound modality in the emergency departments [1]. Advanced Trauma Life Support (ATLS) guidelines consider it an adjunct to the primary survey [2]. In the context of abdominal trauma, the primary use of the FAST exam is the detection of . We can use it to detect as little as 200 mL of fluid in the abdomen[3].
There has been some debate amongst trauma specialists about the utility of the FAST exam [4,5,10]. In particular regarding its sensitivity and specificity, and whether it reduces the incidence of unnecessary imaging, such as computed tomography (CT), or invasive interventions, such as diagnostic peritoneal lavage (DPL) and exploratory laparotomy [4].
The usefulness of the FAST exam is in primarily in ruling in intra-abdominal injury; its specificity in the hands of emergency physicians in this setting has been proven [4,9]. If the emergency physician detects fluid, the specificity of the FAST exam for this finding is high, between 96.0 and 100.0% [4-10]. A negative sonogram does not, however, definitively rule out an intra-abdominal injury; the reported sensitivity of the FAST exam is between 42.0% and 96.0% [4-10]. These numbers are a moving target, since the sensitivity and specificity of the FAST exam depends on a number of other factors, including operator experience, time since injury, and volume of pathological intra-peritoneal fluid.
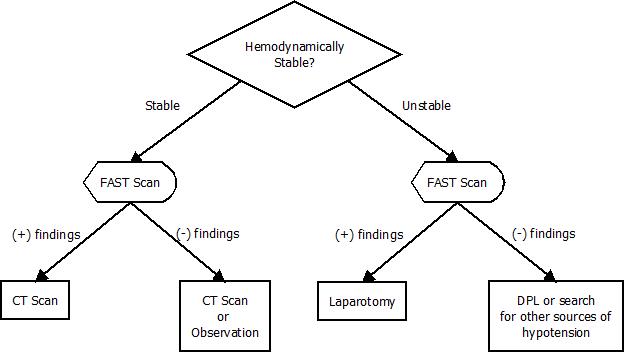
In the setting of acute trauma, these characteristics support its use as a screening test to decide on further management. If the patient is hemodynamically-stable and the FAST exam is positive, they usually will require a CT scan to further characterize their injuries. If the FAST exam is negative, CT may be clinically indicated to definitively rule out intra-abdominal injury.
If the patient is hypotensive, a positive FAST exam strongly indicates the need for therapeutic laparotomy. A negative FAST exam does not preclude hemoperitoneum, so one may need to employ alternate clinical tools in order to search for other sources of hypotension.
The Bottom Line
The FAST exam is highly-specific for intra-abdominal injury, and useful in the hemodynamically-unstable patient. An algorithm summarizing these findings is shown in Figure 1.
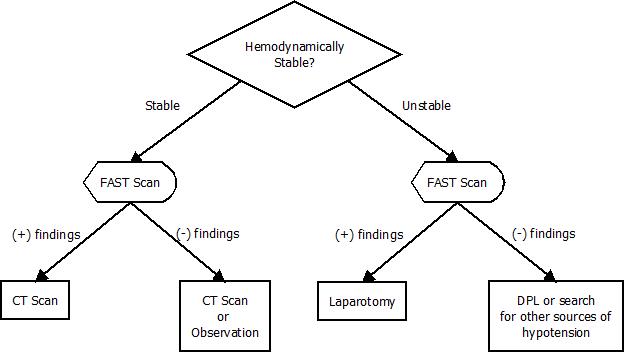
Figure 1: Algorithm for the interpretation of the FAST exam. DPL: Diagnostic peritoneal lavage
Back to the Case
You perform the FAST exam, and notice an anechoic area around the spleen consistent with fluid. The patient is transferred to the operating theatre, where he is found to have a grade IV splenic laceration. The patient undergoes a splenectomy, and is discharged home after a short course in the ICU. By screening the patient with a FAST exam during the primary survey, you avoided a CT scan and arrived to the OR for definitive management expeditiously.
[bg_faq_start]References
- R Henneberry et al. Use of point of care sonography by emergency physicians. CJEM 2012; 14(2):106-112.
- ATLS Subcommittee. Advanced Trauma Life Support: the ninth edition. J Trauma Acute Care Surgery 2013 May; 74(5):1363-6.
- M Liu, C Lee, K P’Eng. Prospective comparison of diagnostic peritoneal lavage, computed tomographic scanning, and ultrasonography for the diagnosis of blunt abdominal trauma. J Trauma 1995; 39(2):375-380.
- D Stengel et al. Emergency ultrasound-based algorithms for diagnosing blunt abdominal trauma. Cochrane Database of Systematic Reviews 2013, Issue 7.
- M Miller et al. Not so FAST. J Trauma 2003 Jan; 54(1):52-9.
- W Ascher, S Parvin, R Virigilio. Echographic evaluation of splenic injury after blunt trauma. Radiology 1976; 118:411-415.
- P Bode et al. Abdominal ultrasound as a reliable indicator for conclusive laparotomy in blunt abdominal trauma. J Trauma 1993; 35(2):27-31.
- J McGahan et al. Use of ultrasonography in the patient with acute abdominal trauma. J Ultrasound Med 1997; 16(10):653-662.
- B Lee et al. The utility of sonography for the triage of blunt abdominal trauma patients to exploratory laparotomy. AJR Am J Roentgenol 2007;188(2):415-421
- D Stengel et al. Systematic review and meta-analysis of emergency ultrasonography for blunt abdominal trauma. Br J Surg 2001 July; 88(7):901-12.