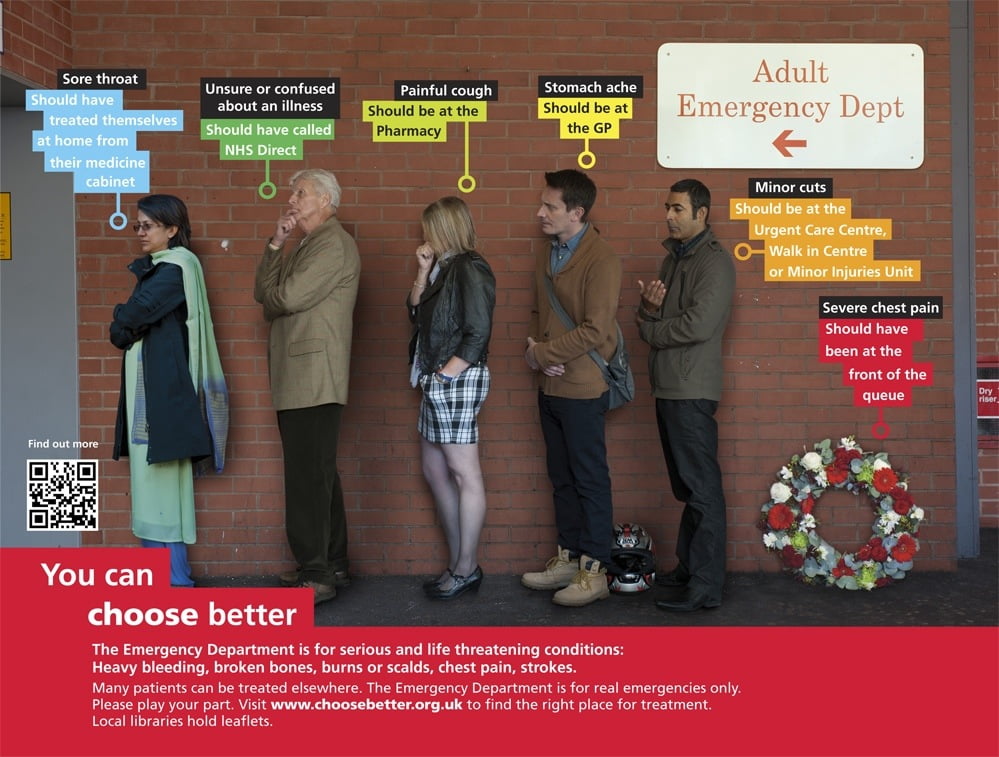
It recently came to my attention that the UK has been deploying a public health message with regards to ER wait times; more specifically, it looks like a public education campaign aimed at redirecting “inappropriate” visits away from emergency rooms. The premise is that many minor and non-life-threatening conditions can be (and should be) treated outside the ER, and that the onus is on the patients themselves to basically triage their own ailments.
Although at first glance this may sound like a reasonable solution to ER wait times, it may actually be inappropriate blame-shifting without supporting evidence.
There is certainly no question that extreme ER wait times are associated with bad outcomes; more and more studies are being published that associate long wait times with undesirable quality of care, including antibiotic delay in pneumonia, poor pain control, and suboptimal time to therapy for heart attacks.
However, it is important to remember that those are associations, and not cause-and-effect relationships. It is more likely that the poor clinical outcomes and prolonged ER wait times are both symptoms of a greater underlying problem: an overstretched acute care system.
Nonetheless, efforts to help reduce ER wait times would go a long way to preventing disastrous stories like this. The NHS’ latest effort seem to suggest that patients are contributing to the problem by inappropriately utilizing ER services for non-emergent medical conditions.
Two immediate concerns with this approach pop into mind: firstly, there are inherent dangers of asking the average non-medically trained citizen to self-triage their own acuity (some of this was explored in greater detail in a prior post on publishing ER wait times). Most who decide to visit an ER are genuinely concerned and worried that something terrible is going on with their health. Actively discouraging such patients to seek timely medical attention (especially during off hours) may lead to greater missed diagnosis and treatment.
More importantly, there is little evidence to suggest that patients presenting with “minor” conditions actually contribute to significant delays in sick ER patients. A study published in 2007 retrospectively examined a database encompassing all Ontario Emergency Departments, and found that the volume of low-acuity patients arriving to the ER had practically little/no effect on length of stay for medium- or high-acuity patients (i.e. the sicker ones who need more timely attention).
In addition, a large proportion of ER volume are created by healthcare professionals themselves – the ultimate discharge instruction for all patients (whether after a surgery, a regular GP checkup, or even a previous ER visit) is for them to present themselves to the ER for anything of concern. Everyone uses the ER as their own 24-hour safety net.
Bottom line: there is insufficient evidence at this time to support that so-called inappropriate self-triage by patients actually lead to poorer clinical outcomes associated with long ER wait times. Having said that, it is certainly true that ER visits for many of the complaints we see today are much more costly to our healthcare system than if they were dealt with elsewhere – and in many instances, would’ve provided better care than possible in the crowded ER with no continuity of care.
But is it reasonable to put the blame on patients themselves? Perhaps, instead, we need to develop novel strategies to meet patients’ needs beyond making Emergency Departments the sole safety-net for the whole healthcare system. Blame-shifting without concrete evidence will not only yield little results…it may lead to unintended consequences.
Update: And here’s a TV ad that spawned from the same campaign. What do you think? Effective education, or scare tactic?