You’re on a night shift in the ED and receive a patch about a 75-year-old female with altered LOC. EMS reports an empty bottle of doxepin was found in her home. The patient is tachycardic and hypotensive, and on arrival has a GCS of around 12. You quickly look up the class of medication that doxepin belongs to, and realize it’s a TCA.
What do you need to worry about in this patient, and which treatments should you start?
Mechanisms of Action
To understand the complications and management of TCA overdose, it’s helpful to consider the mechanisms of action of TCAs1,2:
- sodium channel blockade => QRS widening, dysrhythmias, decreased inotropy leading to decreased cardiac output and hypotension
- alpha receptor blockade => decreased systemic vascular resistance and hypotension
- GABA blockade => seizures
- norepinephrine and serotonin reuptake inhibition => initial hypertension and subsequent hypotension; increased risk of serotonin syndrome when combined with other serotonergic drugs (e.g., SSRIs, MAOIs)
- potassium channel blockade => QTc prolongation
- anticholinergic toxidrome
- antihistaminergic sedation
ECG Signs of TCA Overdose 3–5
- Sinus tachycardia (likely the first to appear, due to the anticholinergic effects)
- Wide QRS > 100 ms
- Prominent R wave in aVR (R > 3 mm, R/S > 0.7). May also see Right Axis Deviation, RBBB pattern, and a prominent R wave in V1.
- QTc prolongation > 430 ms
- Rarely, a Brugada-like pattern can be seen in V1-V3
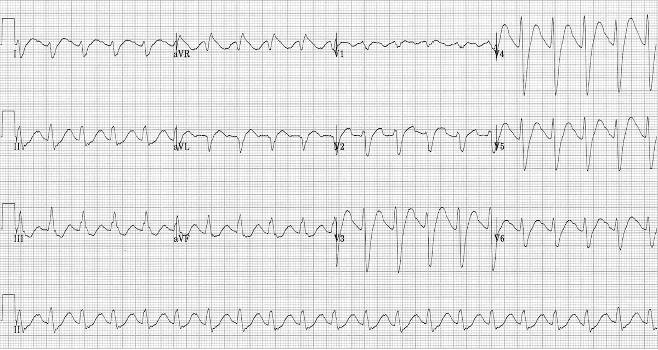
The ECG is the best predictor of the clinical course in TCA Overdose, as opposed to drug levels. In one study, QRS width > 100 ms carried a 33% risk of seizures, and QRS > 160 ms carried a 50% risk of dysrhythmias. No seizures or dysrhythmias occured below these respective thresholds.6
Management Priorities
1) Manage ABCs – Treat hypotension with IV fluids and vasopressors if needed. Norepinephrine or epinephrine are first-line choices. There is limited experimental evidence in animals suggesting that epinephrine may be more effective at reducing the cardiotoxic effects of TCAs. Norepinephrine is a physiologically sensible choice, given the alpha blocking effects of TCAs, as well as their inhibition of norepinephrine reuptake.1,3
Intubation should be considered early, especially in a known massive overdose. Consider intubating earlier for GCS<8, refractory seizures, hypoventilation, or airway compromise3.
2) Gastric decontamination – If less than 1 hour from ingestion (or unknown time), give activated charcoal. This requires the patient to be protecting their airway, or intubated, as there is a significant risk of aspiration with activated charcoal (a risk not completely eliminated by intubation). Particularly in a massive overdose, consider giving activated charcoal even up to 4 hours post ingestion. The anticholinergic effects of the drug slow gastric emptying, so there may still be some benefit from late gastric decontamination. Consider gastric lavage for a massive overdose within 1 hour of ingestion, again necessitating a protected airway.3
3) Sodium bicarbonate – Start with 1-2 mEq/kg boluses of a 1 mEq/mL solution (50-100 mEq, or 1-2 amps), repeating every few minutes until the QRS narrows. Then start an infusion of 150 mEq bicarb in 1L D5W with 40 mEq KCL at ~250 mL/hr (titrated to QRS and pH targets). Goals of therapy are QRS < 100 ms and pH 7.5-7.55.3,7
Mechanisms of Action:
- Sodium to counteract sodium channel blockade (decreases the time required for cells to depolarize, narrowing the QRS).
- The full mechanism by which bicarbonate improves toxicity is incompletely understood. Alkalinization of the blood increases protein-binding to TCAs, which decreases the amount of unbound TCA able to bind to sodium channels. It also increases the amount of unionized TCA in the blood, leading to decreased binding to sodium channel receptors. Finally, it may also more directly affect cardiac depolarization.
The exact contribution / clinical significance of each of these effects is unclear, but data from both animal and in vitro studies support the efficacy of both the sodium and bicarbonate components on narrowing the QRS.7
There is no definitive evidence to guide dosing decisions with respect to the necessity of an infusion versus boluses alone, or even definitive targets.3,7Based on a 2003 survey, most poison control directors still recommend a bolus followed by an infusion.8 Multiple case reports of TCA overdose treated with upwards of 75 amps of sodium bicarbonate (!!) do suggest that large volumes of sodium bicarbonate can safely be administered if indicated (although a VBG should be checked after giving more than 2-4 amps).9,10
4) Benzodiazepines – indicated for treatment of seizures or agitation. Do not use phenytoin.3
5) Monitor electrolytes and pH with serial measurements – Look out for hypocalcemia and hypokalemia (secondary to bicarbonate-induced alkalosis), which can worsen hemodynamic instability and dysrhythmias, and may require replacement.7
Second-Line Therapies:
These therapies all have minimal evidence that stems largely from case reports or experimental/animal studies.
Hypertonic saline – Similar mechanism as sodium bicarbonate in overwhelming the sodium channel blockade. Although there is a greater volume of evidence supporting sodium bicarbonate, some studies have found that hypertonic saline works equally well (and the two are unlikely to ever be compared in a large randomized control trial). Hypertonic saline is a good option in several circumstances:
- Significant alkalosis (pH > 7.55)
- Significant hypokalemia
- Sodium bicarbonate is unavailable
- Hypotension or dysrhythmias refractory to sodium bicarbonate1,11
Intralipid Emulsion – Indicated (if available) for the treatment of refractory hypotension or dysrhythmias, after failure of sodium bicarbonate treatment. This should be administered in consultation with the poison center or a toxicologist. An initial bolus of 1.5 mL/kg of 20% lipid solution is a reasonable starting point, which can be repeated if no improvement after several minutes, and followed by an infusion if there is clinical improvement.1,3
Lidocaine – A counterintuitive option, given that it is also a sodium channel blocker, but the proposed mechanism of action involves outcompeting TCAs in binding to sodium channels. Unlike TCAs, which act more slowly, lidocaine rapidly unbinds from sodium channels, resulting in more unbound channels available to generate a cardiac action potential. Indicated for the treatment of refractory dysrhythmias.12,13
Magnesium Sulfate – For refractory dysrhythmias, especially in the context of prolonged QTc.3 However, the effects of the prolonged QTc interval in TCA overdose are rarely clinically significant, as the sinus tachycardia typically seen has a protective effect by shortening the QTc.
ECMO – If available, ECMO should be initiated for refractory dysrhythmias, hemodynamic instability, or cardiac arrest. Although rarely used, several case reports have reported successful outcomes (including survival to hospital discharge and complete neurologic recovery) following the use of ECMO in these circumstances.14
More FOAMed on this Topic
- Emergency Medicine Cases: Massive TCA Overdose https://emergencymedicinecases.com/critcases-massive-tca-overdose/
- EMCrit Podcast 98: Cyclic (Tricyclic) Antidepressant Overdose https://emcrit.org/emcrit/tricyclic-antidepressant-overdose/
- EM:RAP Episode 138: TCA Overdose https://www.emrap.org/episode/march2013/tcaoverdose
This post was copy-edited by @jamievanderende.
References
- 1.Walls R, Rosen P. Rosen’s Emergency Medicine: Concepts and Clinical Practice. 9th ed. Elsevier; 2018.
- 2.Bruen C. Toxicology Board Review. Resus Review. Published May 2, 2013. https://resusreview.com/2013/toxicology-board-review/.
- 3.Body R, Bartram T, Azam F, Mackway-Jones K. Guidelines in Emergency Medicine Network (GEMNet): guideline for the management of tricyclic antidepressant overdose. Emergency Medicine Journal. Published online March 24, 2011:347-368. doi:10.1136/emj.2010.091553
- 4.Burns E. Tricyclic Overdose. Life in the Fast Lane. Published February 7, 2021. https://litfl.com/tricyclic-overdose-sodium-channel-blocker-toxicity/
- 5.Kiran H, Ravikumar Y, Jayasheelan M, Prashanth. Brugada like pattern in ECG with drug overdose. J Assoc Physicians India. 2010;58:120-122. https://www.ncbi.nlm.nih.gov/pubmed/20653158
- 6.Boehnert MT, Lovejoy FH Jr. Value of the QRS Duration versus the Serum Drug Level in Predicting Seizures and Ventricular Arrhythmias after an Acute Overdose of Tricyclic Antidepressants. N Engl J Med. Published online August 22, 1985:474-479. doi:10.1056/nejm198508223130804
- 7.Bruccoleri RE, Burns MM. A Literature Review of the Use of Sodium Bicarbonate for the Treatment of QRS Widening. J Med Toxicol. Published online July 10, 2015:121-129. doi:10.1007/s13181-015-0483-y
- 8.Seger DL MD, Hantsch C MD, Zavoral T MD, Wrenn K MD. Variability Of Recommendations For Serum Alkalinization In Tricyclic Antidepressant Overdose: A Survey Of U.s. Poison Center Medical Directors. Journal of Toxicology: Clinical Toxicology. Published online January 2003:331-338. doi:10.1081/clt-120021999
- 9.Pierog JE, Kane KE, Kane BG, Donovan JW, Helmick T. Tricyclic antidepressant toxicity treated with massive sodium bicarbonate. The American Journal of Emergency Medicine. Published online November 2009:1168.e3-1168.e7. doi:10.1016/j.ajem.2008.11.026
- 10.Elsamadisi P, Sclafani A, Eche IM. Delayed Cardiotoxicity From a Massive Nortriptyline Overdose Requiring Prolonged Treatment. Journal of Pharmacy Practice. Published online April 14, 2019:543-547. doi:10.1177/0897190019838700
- 11.Eken C. Hypertonic saline: An alternative therapy in TCA overdoses failed to respond sodium bicarbonate. Clinical Toxicology. Published online January 2008:488-488. doi:10.1080/15563650701636374
- 12.Giwa A, Oey E. The return of an old nemesis: Survival after severe tricyclic antidepressant toxicity, a case report. Toxicology Reports. Published online 2018:357-362. doi:10.1016/j.toxrep.2018.03.009
- 13.Foianini A, Joseph Wiegand T, Benowitz N. What is the role of lidocaine or phenytoin in tricyclic antidepressant-induced cardiotoxicity? Clinical Toxicology. Published online January 2010:325-330. doi:10.3109/15563650.2010.487050
- 14.Ikejiri K, Akama Y, Ieki Y, et al. Veno-arterial extracorporeal membrane oxygenation and targeted temperature management in tricyclic antidepressant-induced cardiac arrest. Medicine. Published online March 5, 2021:e24980. doi:10.1097/md.0000000000024980
Reviewing with the Staff
Management of TCA toxicity primarily focuses on the backbone of toxicology, providing excellent supportive care with airway support, blood pressure support and treatment of seizures as needed. A few unique management options are worth delving into further.
No specific antidote exists for TCAs (and no, physostigmine should not be considered in these patients!). Large ingestions are at risk for severe toxicity and therefore decontamination, where feasible, becomes important. Early presentations (<1hr) after a likely ingestion of a large amount of TCA is one scenario I would consider intubation and gastric lavage. This should only be performed if the provider is comfortable with the procedure and has the time and resources to do so. If the patient is unstable or there are limited resources, stabilization should always take priority. TCAs will adsorb to activated charcoal so this is another good decontamination method if the patient is awake and alert or has been intubated. Activated charcoal can still be considered past the 1hr traditional cut-off, such as up to 4hrs post ingestion, due to its anticholinergic action that may slow gastric emptying or potential of large pill burden (1).
Sodium bicarb for the treatment of sodium channel blocker toxicity had been used successfully in TCAs and for other sodium channel toxins. The mechanism has been debated, but is likely a synergistic effect of the hypertonic sodium bolus and the systemic alkalization (2). This works to both lessen the degree of sodium channel blockade and decrease the amount of TCA bound at the cardiac sodium channel respectively. The contribution of each may vary depending on the specific drug involved due to slightly different binding kinetics on the target cardiac receptors (2).
Initial treatment with sodium bicarb boluses to improve hemodynamics, arrhythmias and to narrow the QRS can be followed by a bicarb infusion to maintain serum alkalinity. Bicarb infusions rely on the theory of decreased TCA toxicity at the sodium channel at alkaline pH, however they have not been shown to decrease or prevent recurrence of the sodium blockade (3). Choosing to use either intermittent bolus dosing or bolus dosing followed by an infusion are both reasonable, recognizing that recurrent boluses may still be required while on a bicarb infusion (4).
While some patients may require a significant number of sodium bicarb boluses over the entire course of their treatment, it’s important to be careful of overzealous administration and risk of iatrogenic harm. Frequent reassessments of serum pH and sodium during bolus treatment will help avoid development of severe hypernatremia and alkalosis (5,6). If pH targets become elevated at 7.55 or if significant hypokalemia limits further bicarb use, hypertonic saline (3%) is reasonable to try using 1-2mL/kg per dose (7).
Finally, remember to consider rescue treatments such as intralipid for rapidly decompensating patients or cardiac arrest. ECMO is slowly gaining more evidence (limited to case reports currently) for its use in severely poisoned patients and can also be considered depending on local availability (8).
References
1. American Academy of Clinical Toxicology, European Association of Poisons Centres and Clinical Toxicologists. Position paper: single-dose activated charcoal. Clinical Toxicology. 2005 Jan 1;43(2):61-87.
2. Bruccoleri RE, Burns MM. A Literature Review of the Use of Sodium Bicarbonate for the Treatment of QRS Widening. J Med Toxicol. 2016 Mar;12(1):121-9. doi: 10.1007/s13181-015-0483-y. PMID: 26159649; PMCID: PMC4781799.
3. Hoffman JR, Votey SR, Bayer M, Silver L. Effect of hypertonic sodium bicarbonate in the treatment of moderate to severe cyclic antidepressant overdose. A J Emerg Med. 1993; 11(4): 336-341.
4. Seger DL, Hantsch C, Zavoral T, Wrenn K. Variability of recommendations for serum alkalinization in tricyclic antidepressant overdose: a survey of U.S. Poison Center medical directors. J Toxicol Clin Toxicol. 2003;41(4):331-8. doi: 10.1081/clt-120021999. PMID: 12870873.
5. Wren K, Smith BA, Slovis CM. Profound alkalemia during treatment of tricyclic antidepressant overdose: a potential hazard of combined hyperventilation and intravenous bicarbonate. Am J Emerg Med. 1992:10(6): 553-555.
6. Chang KY, Lee IH, Kim GJ, Cho K, Park HS, Kim HW. Plasma exchange successfully treats central pontine myelinolysis after acute hypernatremia from intravenous sodium bicarbonate therapy. BMC Nephrol. 2014;15:56.
7. McCabe JL, Cobaugh DJ, Menegazzi JJ, Fata J. Experimental tricyclic antidepressant toxicity: a randomized, controlled comparison of hypertonic saline solution, sodium bicarbonate and hyperventilation. Ann Emerg Med 1998;32: 329-333.
8. Ikejiri K, Akama Y, Ieki Y, Kawamoto E, Suzuki K, Yokoyama K, Ishikura K, Imai H. Veno-arterial extracorporeal membrane oxygenation and targeted temperature management in tricyclic antidepressant-induced cardiac arrest: A case report and literature review. Medicine (Baltimore). 2021 Mar 5;100(9):e24980. doi: 10.1097/MD.0000000000024980. PMID: 33655968; PMCID: PMC7939188.



