What is an emergency medicine doctor? The answer likely differs between a major academic centre and a rural hospital. Perhaps the simplest definition is any physician who staffs an emergency department (ED).
When it comes to training, emergency medicine (EM) certainly holds the title of most heterogeneous specialty in Canada. While some physicians complete a five-year residency in EM and are Royal College certified, others complete a one-year EM fellowship after two years of family medicine training. This second group is collectively referred to as EM certified as they have passed their respective EM specific board exams. There are pros and cons to both pathways to emergency medicine.1
Besides these two routes, family physicians can and do practice EM. Research from 2003 estimated that 45% of physicians practising EM are family doctors without the EM fellowship.2 A 2017 survey of doctors working in EDs in Canada heard from 2,924 family physicians without the EM fellowship, compared to 3,536 EM-certified respondents.3 While most of these physicians work in rural settings, some do work their way into practising at medium or large community centres, and even academic sites. The same 2017 report reveals 38.9% of family physician respondents work in urban centres.3
It is not uncommon for a second-year family medicine resident keen on EM to go unmatched to an EM fellowship. In 2022, 102 residents who applied to the various enhanced skills programs did not match, including to EM.4 If you find yourself in this position, it is important to know there are still options for a career in EM. There is also a need for more EM physicians in Canada. There is currently an estimated shortage of 1,000 EM doctors across Canada.3 Canadian EDs have closed at an unprecedented rate in 2022, due to both nursing and physician shortages.5
There are many paths to emergency medicine for a family physician. The first option is simply to dive in. Depending on your exposure to EM in your family medicine residency, this may be a viable option. A recent family medicine graduate who has spent all their elective time in EM or related specialties and who has completed the mandatory certification courses may feel prepared to staff a rural or remote ED. Given that many fellowship applicants are spending their elective time in the ED and getting a jump on courses, if they do find themselves unmatched to EM, they may already be well-prepared for rural EM.
The dive-in path is not for the faint of heart and requires a fine balance between confidence and humility. The extremely risk-averse physician could become overwhelmed with anxiety, and the extremely risk-tolerant physician may fall into hubris. For both patient safety and physician wellness, this type of practice requires good support from department leadership. Having a helpful and experienced backup physician close by is an absolute necessity for the new-to-practice family physician in the ED.
While most departments staffed by family physicians are single coverage (i.e. one physician on shift at a time), there are also opportunities to be a second or third physician in the department to help with volumes. This allows for informal mentorship and in-house backup for acute cases. Some departments will also accommodate so-called buddy shifts in which two new graduates work together. This usually means splitting the hourly rate in centres that don’t operate on a fee-for-service model.
Avenues to expand emergency medicine skills as a family physician
There are both recommended and required courses for the family medicine doctor who works in the ED. Advanced Trauma Life Support, Advanced Cardiac Life Support, Pediatric Advanced Life Support, and Neonatal Resuscitation Program are typically mandatory. These can be supplemented with point-of-care ultrasound, airway, orthopedics, and emergency obstetrics, as well as courses in cardiology, which are available through various academic institutions or from individual physicians.
In addition to formal offerings, self-directed learning is an essential part of building competency for any budding emerg doc. Luckily, EM is a field that has enthusiastically embraced so-called free open access medical education . There is a blog post or podcast for nearly every topic.
Some regions also offer an EM mentorship program, where a family doctor mentee is paired on each shift with a more experienced physician. The number of shifts offered and the funding models for these programs vary by region. This may be a good option for anyone who feels they need a bit of extra supervision during the transition into independent practice.
There are also options for the family physician who feels they need more fulsome training before forging into the field. Many family medicine residency programs fund additional residency blocks for rural enhanced skills. These can be a choose-your-own-adventure curriculum to shore up various acute-care skills required for rural practice. They typically start immediately after second year of residency. Many general practitioner anaesthetists (i.e. family physicians with a one-year anaesthesia fellowship) include emergency shifts in their practice, so an anaesthesia fellowship may be a good route for a family physician who wants to combine EM and either rural medicine or anaesthesia.
Two programs exist in Canada tailored to rural family physicians to increase their competency in EM: the Supplemental Emergency Medicine Experience (SEME) in Ontario, which has sites at the University of Toronto and the Northern Ontario School of Medicine, and the Nanaimo Emergency Education Program (NEEP) in British Columbia. Both these programs span 12 weeks and offer structured weekly academic sessions in addition to supervised emergency practice and elective time.6,7
For the family physician with designs on larger centres or an academic appointment, some combination of these options can help build clinical acumen and gradually work up to busier departments with higher acuity. Some doctors may choose to challenge the EM board exam, which involves writing the same test taken by colleagues in the EM fellowship. This can be done as a practice-eligible candidate (vs. residency-eligible candidate) once a physician has completed 400 hours per year of EM for four consecutive years.8
Finally, there is always the option to reapply to EM fellowships through CaRMS. Some programs outside of Ontario accept applications from practising family physicians.
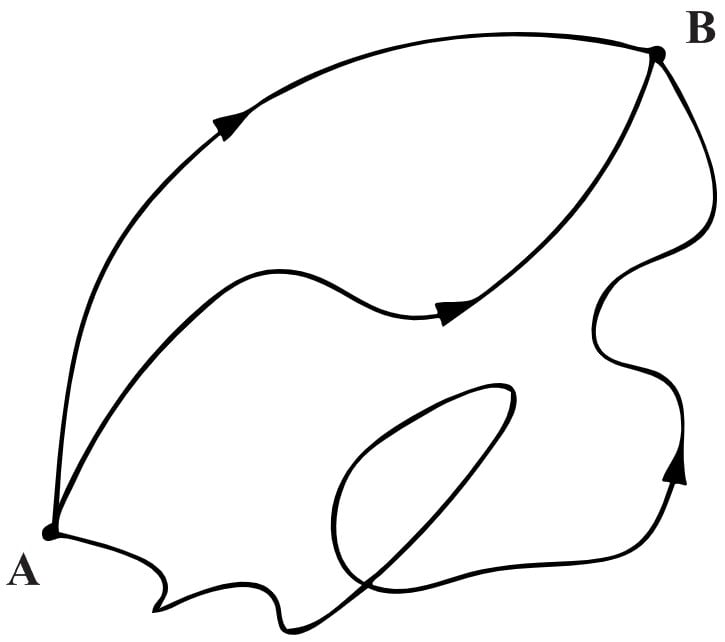
The pathway to becoming an emerg doc is far from linear. Which branches you take depends on many factors, including risk tolerance, location, family considerations, finances, personality, mentorship, and support. While family physicians may need to get creative when it comes to building their skills, they are clearly needed in EDs across the country. If you are a family medicine resident or physician who did not match to an EM fellowship, don’t despair. Get to work on becoming the great emerg doc you want to be!
This post was copyedited by Geordon Omand and was edited by Daniel Ting.
References
- 1.Thoma B. FRCPC or CCFP-EM: What is best for you? CanadiEM. Published March 21, 2022. Accessed June 4, 2022. https://canadiem.org/frcpc-or-ccfp-em-what-is-best-for-you/
- 2.Steiner I. Emergency medicine practice and training in Canada. CMAJ. 2003;168(12):1549-1550. https://www.ncbi.nlm.nih.gov/pubmed/12796335
- 3.Sinclair D, Abu-Laban R, Toth P, et al. Emergency Medicine Training & Practice in Canada: Celebrating the Past & Evolving for the Future. Collaborative Working Group on the Future of Emergency Medicine in Canada; 2016:154. https://caep.ca/wp-content/uploads/2017/07/cwg0001_cwg-em_report_-_august_-_final_web.pdf
- 4.Whalen A. CaRMS. CaRMS. Accessed June 4, 2022. https://www.carms.ca/
- 5.Leung W, Andrew-Gee E, Xu X, Bascaramurty D, Alanna S. What’s happening in ERs across Canada? Dispatches on wait times, crowding and closures. The Globe and Mail. https://www.theglobeandmail.com/canada/article-canada-emergency-rooms-wait-times-staffing-shortage/. Published July 16, 2022. Accessed July 16, 2022.
- 6.. Supplementary Emergency Medicine Experience. Family and Community Medicine: University of Toronto. Accessed June 4, 2022. https://www.semedfcm.com/
- 7.. Nanaimo Emergency Education Program. Nanaimo Emergency Education Program. Accessed June 4, 2022. https://neepdocs.ca/
- 8.. Eligibility and Application. The College of Family Physicians of Canada. https://www.cfpc.ca/en/education-professional-development/examinations-and-certification/examination-of-added-competence-in-emergency-medic/eligibility-and-application