Main Points:
- Postpartum Hemorrhage (PPH) should be considered when there is any blood loss that has the potential to cause hemodynamic instability within the first 24 hours postpartum
- PPH is a life-threatening condition
- Management options depend on the etiology (think 4Ts!)
Case presentation:
Surrounded by her husband King Viserys, midwives and maesters, Queen Aemma was due to give birth any minute. Longing for a male heir, the King was under considerable pressure to secure the succession to his throne. In her own words, the Queen set the scene by describing the “childbed” as a battlefield. Unfortunately, these words become truth as Aemma quickly starts to lose blood during the birth of her child. Dystocia ensued, and the maesters presented the option to the king of performing an emergency c-section to potentially save the baby or choosing to do nothing and lose both.
Without Aemma’s consent, he chooses the scenario with the possibility of a male heir. The servants held her down to the bed with soft restraints while the maester performs a vertical incision below the umbilicus and extracts the newborn, all without any anesthesia. Soon after, Aemma loses consciousness while lying in a pool of her own blood. She becomes unresponsive and dies.
There was no effort from the midwives or maesters to resuscitate Queen Aemma. Only King Viserys remained by her bedside, clutching her right arm as he contemplated his choice. Aemma’s quick deterioration reflects an intimidating yet very real and potentially life-threatening risk of childbirth: post-partum hemorrhage.
Background
What is PPH?
Postpartum hemorrhage (PPH) is classically defined as blood loss >1000mL after delivery, or signs and symptoms of hypovolemia in the setting of bleeding within 24 hrs postpartum (1). This is an updated definition from previous, which was defined as >500mL blood loss after vaginal delivery, and >1000mL after c-section. Most importantly, any blood loss that has the potential to cause hemodynamic instability within the first 24 hours postpartum should be considered postpartum hemorrhage (2). However, these definitions include retrospective analysis of blood loss over time and may be of limited use in the acute clinical setting. Clinically, one should be wary of PPH when a patient begins bleeding profusely during or shortly after delivery, becomes hypotensive, tachycardic, or begins to appear drowsy/with altered LOC.
PPH occurs in approximately 5% of all deliveries and is considered a leading cause of maternal death worldwide (2). Similarly, secondary PPH is classified as excessive vaginal bleeding from 24 hours to 6 weeks post-partum.
Table 1 outlines the common causes of PPH:
| Etiology (4Ts) | Risk factors |
| Tone (uterine atony): Most common cause | multiparity, chorioamnionitis, prolonged use of oxytocin, general anesthesia, multiple gestation, polyhydramnios, fetal macrosomia, and uterine fibroids (3) |
| Tissue (retained placenta) | incomplete placenta, succenturiate lobe of placenta, or history of previous uterine surgery (3) |
| Trauma (laceration) | operative vaginal delivery and precipitous delivery (3) |
| Thrombin (coagulopathy) | in-utero fetal demise, placental abruption, sepsis, disseminated intravascular coagulopathy (DIC), inherited coagulation defect (3) |
Basic Clinical Approach
The basic clinical approach to PPH follows the same pathway we are all familiar with, starting with physical exam, vitals (!), and rapid identification. As with any unstable patient, following a systematic approach, such as ABCs, is recommended. Ensuring IV access with large bore IVs is present, as well as applying oxygen and ensuring ongoing monitors on the patient are all fundamental necessities in the management of PPH.
Specific to PPH, one must evaluate for the potential etiology, via the “4Ts” (Table 1). This involves a bimanual examination for a “boggy” uterus, inspection of IV sites for bleeding (suggestive of DIC), rapid inspection of genital tracts for any signs of laceration or trauma, and keeping the potential of retained placenta in mind.
Ongoing vital sign monitoring is imperative: pregnant women may not show signs or symptoms of blood loss until >25% of blood volume is lost (3). Keep your eyes peeled for hypotension, tachycardia (often the earliest sign of PPH (4)) other signs of shock, and large volumes of blood loss.
Certain maneuvers can be helpful, including elevation of the patient’s legs to help with venous return, and insertion of a foley catheter to assist with uterine atony as well as giving the ability to monitor the patient’s ongoing fluid status.
Laboratory investigations should include CBC, type and cross, fibrinogen, and coagulation studies. Imaging studies have a limited role in PPH.
Finally, obstetrics should be consulted or involved in the care of both primary and secondary PPH.
Management
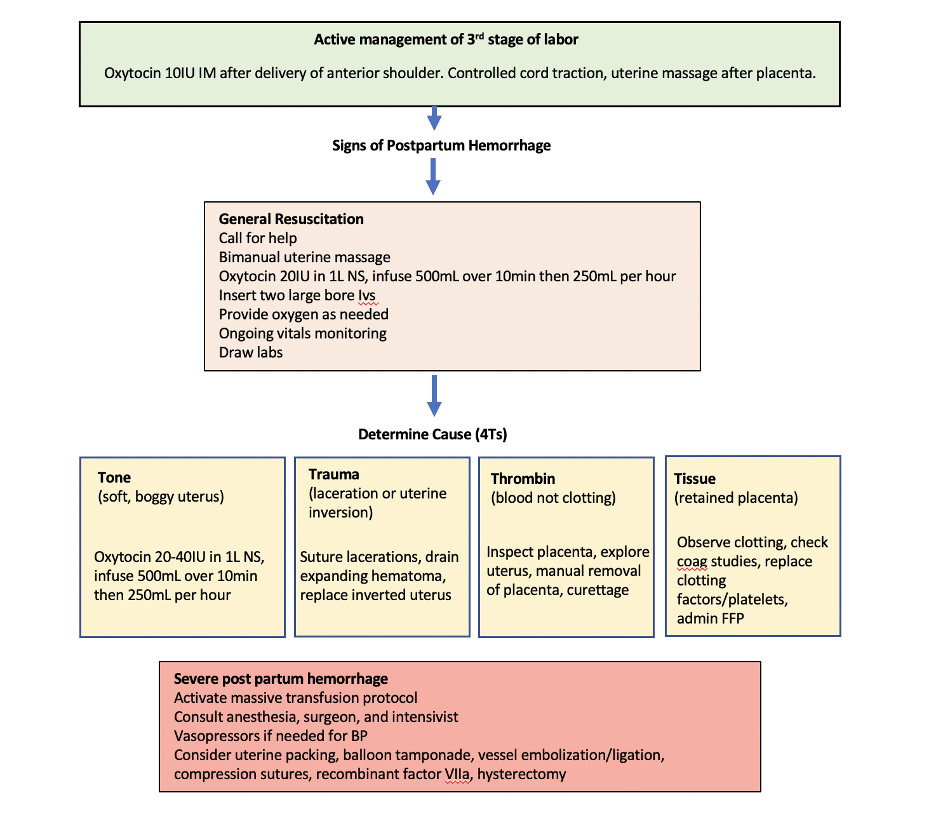
The key to managing postpartum hemorrhage is correctly identifying the cause: An overview of PPH management is provided in Figure 1 and described in detail below. At any point in this pathway, consideration of activation of massive transfusion protocol may be warranted. Clinical discretion regarding patient stability must be used.
Tone (Uterine Atony)
Decreased tone is usually identified by externally palpating the uterus. A uterus with atony feels boggy and soft. If this is the case, then begin with bimanual uterine massage (compress uterus between two hands, one internal and one external). Medical management with uterotonic agents such as Oxytocin is considered standard of care. 20 units of oxytocin in 1 L normal saline can be given IV (routine for normal delivery), or 10 units oxytocin can be given IM to the buttock if IV access has not yet been obtained. In the setting of PPH, an additional 20 units IV (or 10 units IM) may be given. Table 2 provides an overview of uterotonic agents.
Table 2. A brief overview of uterotonics:
| Oxytocin | Produced by the posterior pituitary. Rapidly causes uterine contraction. No contraindications and minimal side effects. Has been shown to be more effective than misoprostol (4). | 20-80 units IV (in 1L NS), or 10 units IM |
| Methylergonovine | Semi-synthetic ergot alkaloid. Rapid onset, causes sustained uterine contraction. Contraindicated in patients with hypertension. | 0.20mg IM q2-4 hours |
| Carboprost (Hemabate) | Synthetic prostaglandin F2alpha, analog of PGF. Contraindicated in severe hepatic, renal, and cardiovascular disease. Caution in patients with asthma as may cause bronchospasm. | 0.25mg IM q 15min (max 2mg or 8 doses) |
| Misoprostol | Prostaglandin E1 analog. Slower onset than others. | 1000mcg rectal (once) |
TXA may be considered as an adjunct if uterotonics fail, however, its use is an area of ongoing research. Early research suggests that, if given within 3hrs postpartum, it reduces mortality due to bleeding but not overall mortality (4). Uterine tamponade with an intrauterine balloon filled with up to 500mL NS can also be considered. Other means of addressing atony-related hemorrhage include pelvic artery embolization (generally performed by interventional radiology) and surgical options (B-lynch sutures, hypogastric artery ligation, or hysterectomy).
Trauma
Trauma is usually identified by visual inspection. If able to visualize the laceration (of vagina/cervix) attempts can be made to cauterize or close the laceration. Both lacerations as well as hematomas are best dealt with in the OR. Techniques to stop bleeding from larger lacerations include ligation of bleeding vessels, use of figure-8 sutures, and layered closure.
Uterine Inversion can also occur following delivery. An inverted uterus generally appears as bluish-gray mass coming from vagina and may cause shock without obvious blood loss. Providers should attempt to replace the uterus using the Johnson Method: Grasp the uterus, direct fingers towards posterior fornix, and lift the uterus while pushing it back into the abdomen. Once reverted, the use of uterotonic agents is recommended. If there is difficulty reverting uterus, adjuncts that support uterine relaxation can be helpful and include MgS04, terbutaline, nitroglycerin, or general anesthetic.
Thrombin
Pathologies inhibiting the formation of thrombin are usually diagnosed through blood work and ongoing bleeding/oozing despite mechanical tamponade. They can be treated depending on their cause by replacing factors and support intravascular volume. It is important to monitor coagulation status with serial blood work. In massive hemorrhage, a thromboelastogram (TEG) may be helpful and is a current area of future research.
Tissue
The presence of retained products of conception in the uterus may be a reason for poor uterine atony and ongoing blood loss and can often be removed manually. If this fails, or if the patient has a known or suspected invasive placenta (placenta accreta, increta, etc), hysterectomy may be needed.
Potential Complications of PPH
There are many potential complications of PPH which can be difficult to manage even with modern day management techniques. These include anemia, fatigue, anterior pituitary ischemia (also known as Sheehan syndrome), and dilutional coagulopathy. In severe cases, PPH can lead to myocardial ischemia and even death. It is important to debrief with patients (as well as staff involved) as traumatic delivery has been shown to cause post-traumatic stress disorders and post-partum depression in many patients.
Back to the case
Our analysis of Queen Aemma’s case reveals a harrowing narrative: no attempt at resuscitation was attempted. She was left in her bed to bleed to death. As authors, we can only speculate that the lack of knowledge from the Maester’s at that time led to the premature “palliation” of the Queen. We use the word palliation lightly as the Maesters did not even attempt to sedate the Queen and make her more comfortable prior to the surgery. Next time, we recommend Milk of the Poppy as both a sedate and analgesic for surgery.
Had the Maesters attempted resuscitation, we would recommend firstly to stop the bleeding. Given this was a cesarean section, closing the incision and uterotonic products would be the first-line treatment. Replacement of blood and clotting factors would also be emphasized. It is unknown if the Maester’s had developed the knowledge or technology required to transfuse blood products at this time, however even collecting her lost blood and replacing it intravenously may have sufficed. Nevertheless, none of the above procedures were performed. No truer words were spoken but by her: “You will lie in this bed soon Rhaenyra. This discomfort is how we serve the realm”.
This post was copyedited by Farzan Ansari (@AnsariFarzan_)
References
1. Committee on Practice Bulletins-Obstetrics. Practice Bulletin No. 183: Postpartum Hemorrhage. Obstetrics Gynecol. 2017;130(4):e168-e186
2. Resources: CPSI. Hospital Harm Measure. (n.d.). Retrieved October 17, 2022, from https://www.patientsafetyinstitute.ca/en/toolsResources/Hospital-Harm-Measure/Pages/default.aspx
3. Wormer KC, Jamil RT, Bryant SB. Acute Postpartum Hemorrhage. [Updated 2022 May 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK499988/
4. Evensen, A., Anderson, J. M., & Fontaine, P. (2017, April 1). Postpartum hemorrhage: Prevention and treatment. American Family Physician. Retrieved October 17, 2022, from https://www.aafp.org/pubs/afp/issues/2017/0401/p442.html



